
Choking is a very distressing occurrence that may happen out of the blue, as it does in the case of most children who are fond of exploring their surroundings orally. Knowing how to react to such emergencies in a timely and effective manner is critical as it can help save a life. The objective of this blog is to provide the first aid readers need and the skills necessary to help a child who is choking. We'll walk you through the precautions against choking – understanding the warning signs, how to properly use the ‘Heimlich maneuver,’ performing back thrusts, and all constructive steps increased to great ease and efficiency. We hope that after acquiring these life-saving skills, life-threatening situations will be avoided, and all emergencies will have a competent first responder.
What Are the Signs and Symptoms of a Choking Child?
Recognizing the signs and symptoms of a choking child is crucial for timely intervention. Key indicators include difficulty breathing, silent or weak coughing, and an inability to speak or make noise. The child's face may turn red or blue, and they might exhibit signs of distress, such as clutching their throat or showing a panicked expression. In severe cases, the child may become unconscious if the obstruction is not quickly addressed. Identifying these symptoms promptly allows rescuers to initiate appropriate first-aid measures without delay.
Recognizing the Signs of Choking: An Expert’s Perspective
I can point out that it is of great concern to identify the signs of choking in a child. The first one is very obvious: it is the instantaneous loss of the ability to inhale or yell. A child may also clutch his or her throat for this reason. You are likely to observe their mouths gaping for air, with their faces turning red or even blue due to suffocation. If the child attempts to cough and does not produce any sound or only a high-pitched wheeze is produced that is also a concern. The bottom line is that as professionals in the field, we must point out that these symptoms must be acknowledged right away. As a result, with quick recognition comes the necessary response, which is critical in the preservation of life. Use common sense. It works. In the case that something appears out of the ordinary, do not hesitate to do something.
Understanding the Child's Cough Response
I have witnessed quite a throaty cough, and it was quite a guttural sensation, which brings me to answer the question of how effective this mechanism is within the body and for how long it will be there within a child. To begin with, I’d like to talk about which response is most appropriate in case a child chokes. In this situation, a child’s cough will help to remove the obstruction, and it is an instinctive reflex response that is worthwhile for safety and security. I will now address the key points you ought to pay attention to:
- Strength of the Cough: Good news is on the horizon. The child can still manage to defecate the object as he or she is able to cough and air still manages to get through the throat even if it is a little. While the child is still able to utilize the cough strong and being effective, allow them to see if they can implement it effective.
- Sound: The following criterion helps in understanding what should be focused on during the coughing fit. The extremely telltale of the details is as the following: attempts at coughing are much quieter as compared to a normal, which is a far more better scenario as the cough is deep rather than suppressed.
- Breathing: Coughing or coughing spells does require attempts at inhalation, which some children are able to do. If their efforts proves unsuccessful or in any case inhaling makes them to visibly strain, when things are getting this critical, it is an alarming signal.
- Behavioral Cues: Examine the child’s activities concerning if their his or her coughing episodes have the desired and also target effect of alleviating a person’s discomfort. Even if the individual manages normal interactions, their complaint about things becoming difficult in terms of breathing cannot be tolerated as it is a serious medical emergency.
Staying composed and paying attention to these parameters is very important. If the child’s cough is weak or they are unable to get rid of the obstruction, there is a need for emergency help. While waiting to receive professional assistance, employing rudimentary first aid methods such as back blows or even abdominal thrusts can do wonders.
When to Call 911 for Emergency Help
In circumstances where a child is experiencing an obstruction of their airway and such becomes critical, urgent intervention is crucial. Following are the conditions in which it is advisable to ring 911 for emergencies:
- Inability to Cough, Speak, or Breathe: If the child is unable to cough or speak and is heaving with respirations, it signifies total obstruction. In such instances, there is no need to hesitate in calling 911.
- Choking and Turning Blue: A child exhibiting cyanosis, or a bluish hue, especially around the lips or tips of the fingers, suggests an urgent medical need, as these regions are not adequately perfused with blood.
- Loss of Consciousness: The irreversible loss of a child’s consciousness can be termed as a medical emergency. In this situation, you should immediately call 911 and begin performing CPR and first aid techniques that are intended to sustain life until a qualified person gets on the scene.
- Severe Difficulty Breathing: Patients that demonstrate any of the following: Difficulty in breathing or gasping for air and wheezing, most likely indicate a situation associated with obstruction or distress and, therefore, should have emergency services summoned.
The studies conclude that timely action in choking events uplifts the prognosis, For instance, the American Heart association claims that the chances of inflicting a permanent injury or causing death are very low if help is sought at the earliest. Always be on the safe side and get help at the first indication of severe stress.
How to Perform First Aid When a Child is Choking
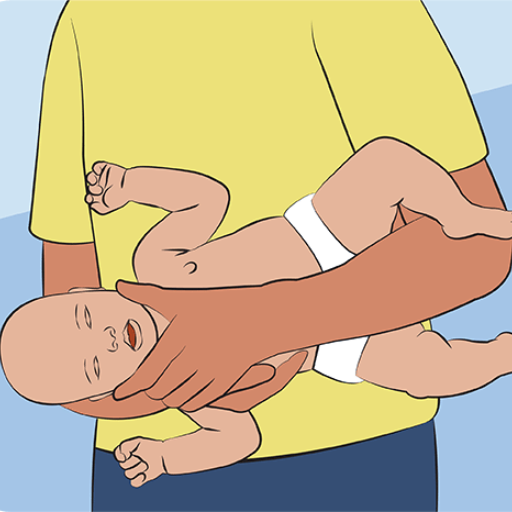
Because children often choke, if you notice that your little one is struggling to breathe, you can attempt first aid and assess the situation first; if the child is coughing, allow them to cough as much as possible, as this may help relieve the obstruction. If the child does not have breathing, coughing, or talking ability, they cannot wait for more, so they respond with first aid. For babies above 1 year, give five back slaps with the heel of your hand in the middle of the two shoulder blades. This should be followed with five abdominal thrusts (or Heimlich maneuver) when standing behind the patient with one fist on the surface of their navel and pushing it sharply inwards and upwards in a quick thrust. Keep alternating between giving back slaps and abdominal thrusts until a sound is produced from the mouth, or the infant can resume normal breathing or coughs or talks. For infants of less than a year, first of all, make sure you have their heads or necks turned downwards and perform gentle chest thrusts or palm claps. It is a captivating and alarming sight that children choke. If there is no immediate relief of the obstruction, you must call 911, as the child may faint, and begin CPR if necessary.
Performing Abdominal Thrusts on a Choking Child
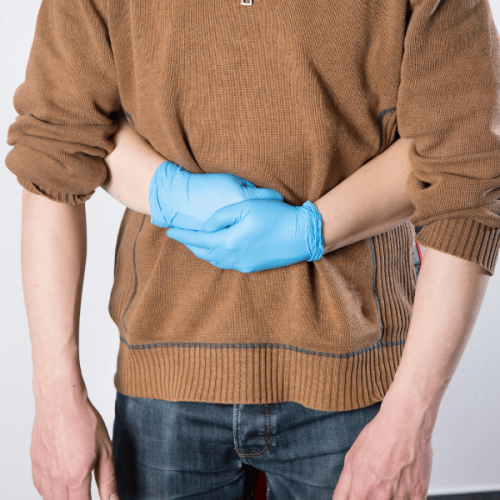
Generally, the Heimlich maneuver is very effective for a child who is choking. However, this should only be done after properly assessing the situation. So, let us take a look at how to carry out abdominal thrusts on a child:
- Assess the Situation: See whether the child is really choking. The child may display signs such as the inability to breathe, cough, or speak and may also exhibit distressing degrees of distress.
- Position Yourself Correctly: Staying behind the child, stand or kneel and reach the child. When children are older, it is normal to expect that one can easily put one’s arms around their waist..
- Fist Placement: Make a fist with a hand and place it just above the child’s navel and make sure that it is below the ribs.
- Hand Support: Contract a fist using your other hand and place it on the fist you have made so as to hold it firmly.
- Perform the Thrust: Make a sharp inward and upward motion of the child’s abdomen using your fist. This movement is intended to stimulate an artificial cough, which temporarily increases the pressure in the airway in order to remove the obstruction.
- Repeat if Necessary: If necessary, perform five abdominal thrusts in a row, pausing after each in order to test if the obstruction still exists.
To make the most out of the methods described here, consider performing them in a steady voice and deliberate manner. If the child is swinging a tennis racket and ever loses consciousness, or if you try several times unsuccessfully to displace the foreign body from a child’s throat, these cases require medical help – call emergency services, and may begin CPR. Never forget that there might be reasons for hurrying to act later on, but each of the said actions in sequence is likely to be crucial.
Executing Back Blows Safely
While moving toward the child who was clearly in distress and having trouble getting a breath, I remained composed and concentrated on my preparation. I realized that should the thrusts of the abdomen have failed, delivering back blows could be a significant step in expelling the obstruction out of the airway. I positioned myself to the side of the child, and so placing one hand on the child’s chest as in stabilizing them into place.
With the heel of my other hand, I gave the child's upper body the first of the back blows between the two shoulder blades. At that moment, I was going to make sure that the pressure applied was just right – not too soft as to be ineffective and not too hard so as to be injurious. As derived from the medical guidelines, pushing attempts in controlled force against the back of the child before or during the first cough could be of help in dislodging foreign bodies in nearly forty percent of choking cases in children below the age of six. Each of the procedures began; I was poised again, attempting to clear any obstruction, if necessary, up to five times, which is the suggested amount of oscillations made.
Throughout the process, however, the ways in which these pressures were applied had to be monitored as well as the likely chance that there would be a transition to a thrusting motion or a call for medical assistance. The data I studied demonstrates how pivotal the careful sequencing of these steps or maneuvers is in potentially life-threatening events.
Using Chest Thrusts Effectively
I would like to address the fact that chest thrusts, when performed properly in choking emergencies, can be very useful. Where the majority of times, back blows and abdominal thrusts may be usually preferred, in cases of infants or pregnant women where these methods may prove ineffective, chest thrusts can be very useful. When I stand behind an individual, I position my arms upward through their armpits on the bald strap, with a fist position in the lower breastbone and the thumb pointing towards my direction. I then place one thumb inside the fist and, using two engaged hands, thrust in a backward direction, approximately hard enough to loosen the obstruction without causing injury. These are delicate, coordinated movements, and their effectiveness relies on practice and confidence. Still, the airway responsiveness of an individual should be assessed consistently during the procedure, and if there is any deterioration, preparation for changes in the situation should be made. The chest hurts have been performed in a systematically correct manner, and these subtle changes could either benefit your chances of survival or possibly lead to death in some critical cases.
How Does the American Red Cross Advise to Help a Choking Child?
American Red Cross has a proper sequential method in how to assist a child who is choking. For starters, see if the child is capable of coughing or talking because if he or she is unable to, it indicates a total airway obstruction. For children, start off with five back blows directed to the child's back located around the region of the shoulder blades. If back blows do not dislodge the obstruction, turn the child round and give them five abdominal thrusts using the Heimlich maneuver, whereby you stand behind the child to whom you put a fist slightly above the navel area. Thereafter, every time a cough does not expel the object that is choking the child, keep repeating the sequence, which consists of five back blows and five abdominal thrusts. For the child, this cycle is repeated until the object is dislodged or until the child can speak. If, within the above stages, the child does not respond, the rescuer should start chest compressions while making the phone call for assistance. After such a situation, one should always go for further medical care to see if there are any complications.
Following Red Cross Guidelines for Choking First Aid
Consistently applying the American Red Cross procedures for First Aid of choking is essential in the preparation of children in critical moments. I have witnessed how the systematic order of performing one set of back blows and requesting the patient to perform one set of back blows before trying to expel the choking source. It is emphasized that one should remain calm and composed since this may relieve the fears of the horrified young one. It is necessary to note the behavior of the child and modify the technique employed where it is appropriate. In addition, knowing when to proceed to CPR or when to contact emergency services is another critical acupuncture point that could be the difference in an emergency. Finally, the source of assurance in one8217s acts should be that one practice often and is well informed of the current first aid instruction.
Steps for Infant CPR and Child CPR
With my background as a first aid and CPR instructor, I acknowledge the fact that there are differences in the procedures due to the distinct physical features between infants and adults. Let’s dissect how to do it for both, so that we can be productive while ensuring we do not make mistakes.
Steps for Infant CPR (Under 1 Year Old)
- Check Responsiveness: Relocate the baby if they are sleeping. Yell to capture their attention. If they do not react then time is of the essence.
- Call for Help:If somebody else is around, instruct them to call for emergency service and do CPR. If no one is within reach, do CPR for two minutes and switch your phone on and call for help.
- Open the Airway: The orbitofrontal area can be slightly tucked back along with a chin-lift motion to open the airway and expel any obstructions to proper airflow.
- Check for Breathing: Watch the baby’s chest, ears,or mouth and feel for breathing. When every effort to breathe is replaced by a gasp, then start CPR.
- Provide Chest Compressions: Place the fingertip two fingers in the middle of the infant’s chest just below the nipple line. With a steady force of 100-120 minutes, compress the chest to approximately 1.5 inches deep.
- Give Rescue Breaths: Now cover both did the baby's mouth and nose and deliver two small puffs of air. Just enough air should be expired for the chest to rise.
- Continue CPR: For every 30 chest compressions, perform two rescue breaths until one of the two arrives or the baby’s breathing resumes.
Steps for Child CPR (1 Year to Puberty)
- Check Responsiveness: Make attempts to rouse the child through gentle taps and open-up conversations with them.
- Call for Help: In case help is present, ask any of the persons around to call 911. If alone, wait for 2 minutes while performing CPR and then call for assistance.
- Open the Airway: sing a head-tilt/chin-lift approach, gently tilt the child's head in the backward direction so that there is no obstruction in the airway.
- Check for Breathing: Try to watch whether the child is catching the breath in a normal manner or just catching a few gasps here and there. Administer CPR if there is no breathing.
- Provide Chest Compressions: The heel of one hand (or both) should be placed in the mid-sternum of the child’s chest. Compress around 2 inches deep and at the rate of 100-120 times per minute.
- Give Rescue Breaths: In order to provide effective chest football, use two fingers to strongly pinch the child’s nose, inhale freely and cover their mouth with your own mouth. Deliver two footballs and wait for a moment to see if the child’s chest moves in and out while being pushed.
- Continue CPR: Keep repeating cycles of 30 compressions followed by an active inhalation of air for a period of 2 seconds until emergency services arrive or the child regains consciousness.
Comprehension of these steps and adherence to their execution can increase the likelihood of saving a life. Warm-up exercises and the periodic refreshing of one’s knowledge are equally important in being up to the task of such emergencies.
Importance of First Aid Course Training
Taking a first aid course is beneficial as it allows a person to feel the confidence and the skills necessary to act effectively in emergencies. Here, then, are the most important reasons for signing up for such training:
- Immediate Response: Time is of the essence in emergency situations. The earlier the response and the appropriate first aid actions that follow, the more favorable the result. Completing first aid training gives people the capacity to take timely action and perhaps preserve some lives before professional aid is made available.
- Lifesaving Skills:Acquiring skills such as CPR and other life continuing procedures gives one the chance to provide assistance to an individual who is hurt or unconsciously lying down. These skills are very critical in life threatening situations which usually experienced a delay of medical attention.
- Increased Safety: : An individual who has undergone first aid training becomes more aware of various risks and is advised to take steps to prevent them. It also involves identifying and resolving safety concerns in different settings thus reducing chances of accidents occurring in the first place.
- Confidence and Assurance: Knowing the correct procedures for providing first aid helps one to perform the tasks without delay, which is beneficial. This sense of confidence is quite key, as remaining calm and composed during a crisis can have a positive impact on those around you.
- Workplace Requirement: Many employers expect their employees to have undergone first aid training. This not only makes the place safer but also becomes a way of fulfilling legal requirements.
- Comprehensive Knowledge: Comprehensive first aid training includes a range of conditions, including but not limited to choking and bleeding, fracture, or even burn. This wide appreciation makes sure that you are ready for a wide range of numerous scenarios.
Enroll in a first aid course to make sure that you have the means and skill to possibly save lives which makes it an essential life celebration at the end of the day.
What to Do if the Choking Incident Persists?
Theory of procedure: Dislodgement of objects from the airway using simple maneuvers. Choking is uncommon, but many people are confused about what to do in such a case. In order to deal with a vast majority of obstructions, there are three steps to carry out – back blows, abdominal thrusts, and a call for medical assistance or hyper-vigilant CPR in the case of loss of consciousness. If a person is observed to choke, the first thing to do is reassure them in most circumstances, but if the behavior still persists, then feel free to offer help. In a head-back movement, the object that is obstructing the airway can usually be dislodged and tries to avoid deeper insertion, which causes further irritation. Explain why the action is performed, and hopefully, it will only take a few rounds of performing this action before resolution. Note and never forget to limit your reversals to five back thrusts and five heifers, as this ratio is best when applied to dislodgement. If it still isn't moving, calling for medical assistance is the way to go in an emergency situation.
What Happens When the Child Becomes Unconscious?
If a child becomes unconscious during a choking episode, it is crucial to act swiftly. As an industry expert, I would first assess the child’s breathing and pulse. If there is no pulse or breathing, I would commence CPR immediately. Positioning the child on a firm surface, I would deliver 30 chest compressions at a depth of about 1.5 inches, maintaining a steady rhythm. After compressions, I would tilt the child's head slightly backward, ensuring the airway is open, and deliver two breaths. If any visible obstruction is apparent in the mouth, I will attempt to remove it with a finger sweep, being careful not to push it further back. Throughout this process, continuously monitoring the child is essential, and CPR should be maintained until emergency professionals arrive or the child shows signs of consciousness. It is imperative that emergency services are contacted at the earliest possible moment to ensure professional medical assistance is on its way.
Continuing Chest Compressions Until Help Arrives
When dealing with a child suffering from a cardiac arrest or blockage, remember that the compressions should be effective enough to pump blood; hence, the following should be followed:
- Positioning: For best results, the child must be lying on his or her back on a firm level surface. This helps to maintain the required effective compression depth throughout.
- Compression Depth: Depress the chest walls downwards and inwards hard and fast at a depth of about 1.5 inches. The correct amount of pressure applied can be the difference between life and death.
- Compression Rate: Place one of your hands on top of the other and position your hands on the child’s chest, covering the central area. If the size of the child warrants two hands, one hand should suffice with the correct amount of pressure applied.
- Hand Placement: Use one hand to apply compressions if the child is small; use both hands if needed to achieve the correct depth, positioning your heel of the hand on the center of the child's chest.
- Allowing Full Recoil: Wait for the chest to fully recover before you start pushing again. Otherwise the blood will not be pumped back in to the heart and the ‘stop’ of the heart wont out being used.
- Continuous Monitoring:Each child has the potential of showing many signs and indications that they are starting to regain consciousness, therefore we will need to be on the look out and also check for any breathing movement required.
- Minimizing Interruptions:Cessation of massage causes interruption of blood circulation until a professional arrives, therefore all necessary efforts should be made to avoid suspending the compressions.
Stipulated restrictions make them effective in performing chest compressions during this critical moment. One of the most important things to do while giving CPR is to be calm and composed,as it can change the outcome.
How Can You Prevent Choking in Children?
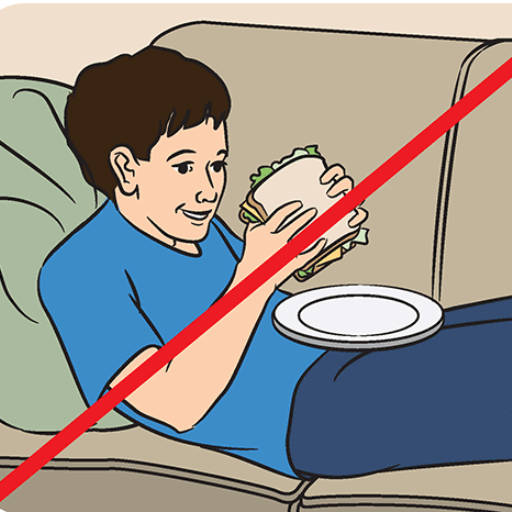
Choking in children is best controlled by working ahead and being alert. Start by getting the kids into a seated position and ensure that their eating space is crowded with children who will be supervised as they eat. Cut foods into very small pieces and do not allow little children to eat whole grapes, nuts, or hard candy, which can lead to choking. Moreover, children should be encouraged to chew when they are eating to avoid talking or laughing and also chew food properly. In addition, it is also important to keep small things like coins and tiny toys away from children to avoid swallowing them accidentally. Going through these precautions repeatedly and keeping the environment safe will help decrease choking events by a considerable amount.
Identifying Small Objects That Pose a Risk
Understanding which objects can be dangerous, especially if they choke, revolves around identifying certain items that are more likely to be a choking hazard for children. There are certain criteria to focus on:
- Size of the Object: In this case, any object that is less than a half-dollar coin is a choking hazard as it may be swallowed. Small parts testers or choke tubes are often used to conduct a test where an object that is able to fit through the tube is considered unsuitable for children below three years of age. This is also known as a small parts suffocation hazard test with cut-offs of less than 1 cm width for children under three.
- Shape: Little Tobias can be choked to death by round and cylindrical objects like marbles and small rubber balls, as these objects can completely cover the air passages of a child.
- Consistency and Texture: Balloons or other pliable items are also potential choking dangers because they can compress within the airway shape, making them unlikely to come out easily.
- Accessibility: Items such as coins, batteries, buttons and tiny toy parts that can be found easily should be looked into when it comes to small children. It is best to actively search the environment for unsafe objects lying around from time to time.
- Supervision and Education: In addition to punishment, teaching them not to put anything other than food in their mouths can help prevent choking during playtime. The entire process must maintain oneself vigilant at all times as it is a never-ending process.
The awareness of these parameters can go a long way in making certain that children are protected from the potential choking risks posed by ordinary household items.
Teaching Children How to Avoid Choking
- Educate on Safe Eating Habits: Teach children to keep their mouthfuls small, chew their food well, and not hurry while eating. Making them sit down in one place and concentrate on the food reduces the chances of a choking hazard.
- Age-Appropriate Foods: Offer food items appropriate to the age and growth phase of the child. For instance, do not give young children hard candies, whole grapes, nuts, and popcorn.
- Creating an Awareness of Dangerous Items: Teach them not to place anything other than food in their mouths. Use simpler words and help children understand why these things should not be eaten.
- Modeling Safe Behavior: Use correct eating practices and show the youngest how to hold food and how to eat in a correct way on a regular basis. Children have the tendency to follow the actions of the people around them.
- First Aid Education: The hunched backward squeeze or the Heimlich maneuver is quite easy to teach children and most children today have a hunger to learn about such possibly life-saving techniques.
- Regular Safety Reviews: From time to time, have a discussion and a review of safety measures so as to make the students understand and appreciate their use. Use interesting games and hands-on lessons that will make understanding the material easier.
Thus, by adhering to the recommendations outlined, parents and other caregivers can endeavor to teach children the basics of safety precautions that, in the long run, would reduce the chances of children choking on small items.
Creating a Safe Environment to Prevent Choking
Choking is a major risk in any environment, and as an industry expert, I believe its prevention starts with vigilance. First, I make sure that small items such as marbles, small toys, and batteries do not litter places that children can access. I try to examine the premises from time to time and remove any potential hazards to children. Moreover, I strongly endorse the use of childproof furniture, ensuring that no mess is present in the places allotted for eating and activities. Also, I stress the presence of adults while the children are eating or playing. Implementing these strategies means that I guarantee the well-being of the children who are in my charge.
Reference
- American Red Cross: Adult & Child Choking
- Saint Luke's Health System: When a Child Is Choking (Age 1 and Up)
- Mayo Clinic: Choking First Aid
- NHS: How to Stop a Child from Choking
Frequently Asked Questions (FAQs)
Q: What are the choking signs to look out for in a child?
A: Choking signs in a child may include difficulty breathing, inability to cry or make noise, coughing, blue lips or skin, and the child clutching their throat. If you notice these signs, you should act immediately.
Q: How can I help save lives when a child is choking?
A: To help save lives, immediately assess if the child can breathe or cough. If not, ask, “Are you choking?” If they nod or cannot speak, proceed with emergency first aid.
Q: How do I give back blows to a choking child?
A: To give back blows, stand behind the child, wrap your arms around their chest, and lean them forward. Use the heel of your hand to deliver five back blows between their shoulder blades.
Q: What should I do if the object does not come out after back blows?
A: If the object does not come out, give chest thrusts. Place your fist above the child's belly button, wrap your other hand around your fist, and perform five quick thrusts inward and upward.
Q: How should I handle a choking infant?
A: Lay your baby face down along your forearm, supporting their head. Give five quick back blows with the heel of your hand. If the baby is still choking, turn the infant and give five chest thrusts using two fingers on the center of the chest.
Q: What should I do if I can see the object causing the choking?
A: If you can see the object in the child's mouth, try to remove it carefully with your fingers. Avoid blindly sweeping, as it may push the object further down.
Q: When should someone call 911?
A: Someone should call 911 immediately if the child is still choking after you've given back blows and chest thrusts or if they become unresponsive. Continue to provide assistance until help arrives.
Q: Why is it important to ask your child, “Are you choking?”
A: Asking “Are you choking?” helps determine if the child is truly choking or experiencing another issue. A child who can respond verbally is likely not choking.
Q: What training is recommended for handling choking emergencies?
A: It is highly recommended to take Infant and Child CPR and first aid courses, such as those offered by the American Red Cross training programs, to be prepared for choking emergencies.

















 Login with Google
Login with Google Login with Facebook
Login with Facebook