
What Are the Signs of Choking in a Child?
 To act with the required precision promptly, identifying the choking victim and assessing their state is the first and foremost step to mitigating the impact of any type of disaster, whether it be a major one or a minor one. A few signs to watch out for include when the first res ignores the fact that the child is playing with innumerable objects, which provides for choking hazards, or when the child is eating. Secondly, when a child struggles to breathe and speak and starts wheezing, it is also a sign of the beginning of a choking scenario. Their hands around their throat are a sign of choking. In addition, if an object entirely blocks the child, they will be unable to talk; action is of the utmost importance here.
To act with the required precision promptly, identifying the choking victim and assessing their state is the first and foremost step to mitigating the impact of any type of disaster, whether it be a major one or a minor one. A few signs to watch out for include when the first res ignores the fact that the child is playing with innumerable objects, which provides for choking hazards, or when the child is eating. Secondly, when a child struggles to breathe and speak and starts wheezing, it is also a sign of the beginning of a choking scenario. Their hands around their throat are a sign of choking. In addition, if an object entirely blocks the child, they will be unable to talk; action is of the utmost importance here.
How to Recognize When a Child is Choking
To determine whether an event constitutes a choking incident for a child, there are physical or behavioral signs. The first stage is the reflex of coughing. This will be observed as a child who is choking tries to breathe and, in the process, makes a slight sound in an attempt to push the object blocking the throat away. A minimal pointing of the tongue could be noticed as well. If the blocking continues, one can also gauge the degree of wheezes produced during the strained breaths. If the reverse worsens, you may be concerned about lacking somewhere in ordinary speech or falsely normal. Further, the child’s face may appear stressed, pale or bluish, and even dry due to lack of sufficient oxygen intake. Lastly, the almost universal hand movement towards the throat of the child’s hands describes choking according to international sign language. If you observe any of these signs, thinking and acting fast to administer first aid without wasting time is essential.Common Choking Hazards for Children
Choking is something that I want to prevent, and achieving that starts with breaking down the choking hazards presented to children. Common culprits are small, round foods such as figurines or items that young children can ingest. These foods should be sliced into small bits, and constant care must be given to these children whenever they are fed. Children can also swallow small round toys or other household objects such as coins or buttons. Even with toys, always go for those suitable according to the child's age and position everything outside their reach. Also, keep on the lookout because balloons and plastic bags, which seem harmless, can pose a dire choking hazard. Therefore, throughout the duration kids are present, supervision is needed.When to Call 911 in a Choking Situation
How to Administer First Aid for a Choking Child
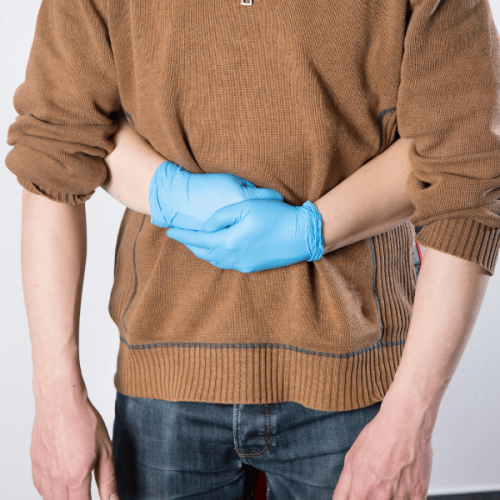
 When providing first aid to a choking child, it is critical to use appropriate and effective techniques that take into consideration the age of the child. For children under a year old, start by placing the baby across your forearm so that the head is lower than the body. Firmly smack the baby back in five regions on the heel of the hand. If this action does not ease the barriers, roll the baby over and firmly use two of your fingers to chest thrust five times below the nipple. Encourage children over one year to cough if they can; if they cannot, then the Heimlich maneuver becomes applicable: whether standing or kneeling from behind the child, give them a side bear hug with one of your hands in a fist. Position the fist above the navel and allow your other hand to cover it. Shake upwards five times quickly to make the enclosed item upwards until it is out. This should be followed by a medical evaluation even in the instance where the child appears to recover to ease the chances of other choking incidences completely.
When providing first aid to a choking child, it is critical to use appropriate and effective techniques that take into consideration the age of the child. For children under a year old, start by placing the baby across your forearm so that the head is lower than the body. Firmly smack the baby back in five regions on the heel of the hand. If this action does not ease the barriers, roll the baby over and firmly use two of your fingers to chest thrust five times below the nipple. Encourage children over one year to cough if they can; if they cannot, then the Heimlich maneuver becomes applicable: whether standing or kneeling from behind the child, give them a side bear hug with one of your hands in a fist. Position the fist above the navel and allow your other hand to cover it. Shake upwards five times quickly to make the enclosed item upwards until it is out. This should be followed by a medical evaluation even in the instance where the child appears to recover to ease the chances of other choking incidences completely.
Steps to Dislodge the Object
When a child is choking, I make sure to follow these life-saving procedures. First, I start by saying the procedure first for children; if the child is not hurt, then look whether it is severe or not: to the infant, the child that does not continue to cough for herself, I place the child on my forearm supporting the head and performing five jobs cut thumbs on the child’s back followed by chest thrusts to the head in repition till the barrier get stopped. For older children, one person grabs them while standing behind them, covers their waist with one arm, and puts her other hand on their head to pull it sideways along with some rapid elbow thrusts, known as the immersion technique. All the above, I continue to remain calm – and am ready to call the ambulance in case the efforts do not work and the child starts losing consciousness. Once the obstacles were removed, I always sought medical advice on whether or not there would be other concerns.How to Give Back Blows and Chest Thrusts
While checking for the signs of choking by performing back blows and chest thrusts on an infant or older child, it is essential to follow any guidelines or techniques. Parents/supervisors of children above 1 year should use these thrusts as a replacement. For children below one year of age, taking the baby into your forearm by placing one hand under the chest needs to be done first. The baby’s head must remain lower than the chest as this gives room for the doctor to make quick movements. If the situation does not change, this process must be repeated: a semi-inclined position should be created, along with five sharp jabs between the shoulder blades using the heel of the other palm. Fingers need to be positioned on the breastbone just below the nipple line and need to be used to perform five sharp thrusts with a ringing down and up motion while continuously keeping the head tilted. Children above the age of one should be encouraged to cough again while awake and responsive. If they appear unable to perform the cough or it is weak, you should perform the Heimlich maneuver while the child is awake. This requires you to stand or kneel behind the child while making a fist with one hand and placing it slightly above the tummy. After that, use your second hand to hold this fist and make several vigorous upward movements into the child's abdomen until the item that has lodged in the throat comes out. Keeping yourself relaxed and acting fast is extremely important in this scenario. Looking around always helps in case the child goes unconscious, and an emergency procedure has to be performed; 911 should always be called, and if certified, CPR must be performed. After successful removal, always have the child seen by a doctor to avoid future concerns.Using the Heimlich Maneuver on Different Ages
What to Do If the Child Becomes Unresponsive
 To provide aid to a child who has stopped breathing as a result of choking, it is essential to call for help and immediately begin performing CPR. First, you want to place the child face up on a hard surface, then check the child and see if they are breathing or have a pulse. If there is no breathing or pulse, initiate CPR, focusing on giving chest compressions. If the child is an infant, compress their chest using your thumb or two fingers at a depth of about 1.5 inches and about thirty times at a rate of one hundred to one hundred and twenty compressions per minute. However, if they are older children, chest compressions using one hand (sometimes two hands are needed) slightly more than 2 inches deep (about 5cm) should work.rk After every 30 compress, repeat the process of breathing into the mouth of the child with the mouth and nose sealed unless they are an infant; then repeat this twice. Provided there are no emergency medical services, keep repeating CPR until the child breathes or paramedics arrive. As a child caregiver, it would greatly benefit you to acquire the proper training to use CPR correctly.
To provide aid to a child who has stopped breathing as a result of choking, it is essential to call for help and immediately begin performing CPR. First, you want to place the child face up on a hard surface, then check the child and see if they are breathing or have a pulse. If there is no breathing or pulse, initiate CPR, focusing on giving chest compressions. If the child is an infant, compress their chest using your thumb or two fingers at a depth of about 1.5 inches and about thirty times at a rate of one hundred to one hundred and twenty compressions per minute. However, if they are older children, chest compressions using one hand (sometimes two hands are needed) slightly more than 2 inches deep (about 5cm) should work.rk After every 30 compress, repeat the process of breathing into the mouth of the child with the mouth and nose sealed unless they are an infant; then repeat this twice. Provided there are no emergency medical services, keep repeating CPR until the child breathes or paramedics arrive. As a child caregiver, it would greatly benefit you to acquire the proper training to use CPR correctly.
Conducting CPR on a Choking Child
If a child is choking and is unresponsive, follow these steps. Before doing anything else, check if help has been called. Lay the child on his back on a hard, flat surface and look for breathing or a pulse. If there are signs of no circulation, begin CPR right away. For children under one, a combination of compressions is put on the center of the chest using two fingers. 30 presses, one and a half inches deep, are made in a rhythm of 100 to 120 per minute. After conducting the pushes, open the mouth and pinch the nose of the baby while watching the chest, and blow air into the child’s mouth twice. For children older than one year, one or both hands perform chest compressions about 2 inches deep, maintaining a rate of 100-120 compressions per minute. Two breaths are then given, ensuring a proper seal is made by placing the child’s mouth and pinching the nose if the child is older. Proceed with 30 chest compressions followed by two breaths till help arrives at the scene or the child starts breathing. If trained, while giving the breaths, check for any obvious obstructions in the mouth after every set of compressions and attempt to remove them only if visible using a finger. Caregivers should take courses for CPR certification to be ready in emergencies and ensure they can perform actions quickly and adequately.How to Perform Infant and Child CPR
The CPR process for an infant commences after placing the child on a firm surface and assessing for respiration and pulse. In the event of an adverse finding, the infant is anointed with two-finger compressions targeting the center of the chest for around one and a half inches deep at a rate of one hundred to two hundred compressions in a minute. Following this, I have two rescue breaths for the child by covering the mouth and the nose until the chest heaves. The procedure for a child above the age of one begins in the same way; only once breathing and pulse are checked and determined absent is the child's size considered. Besides the child's size, the pressing action's depth is two baby inches, and the rate is similar. After every set of 30 compressions, I am liable to give out two rescue breaths, pinching the nose and covering the mouth if it is necessary. The steps have to be adhered to, including restraining anxiety while making sure that I have the proper training to avoid getting overwhelmed until one professional distance arrives or the child wakes up.What to Do Until Help Arrives
How to Prevent Choking Hazards at Home
 Eliminating choking hazards at their very essence is about implementing the required norms of behavior, especially in the areas of the household where children are situated. Ensure that children do not have easy access to small items, including toys that have components that can be detached, buttons, and coins. Check toys for damage as they will wear out, and also make sure there is no deviation in the purchase according to the age limits. Promote healthy practices concerning food by encouraging children to cut food into small sizes and ensuring that the intake of a particular food with more significant risks, such as nuts, large chunks of fruit, apples, and hard candy, is avoided. Ensure children do not watch TV or run while eating, and supervise their meals. Moreover, always keep the house tidy to prevent children from using and swallowing inappropriate objects that may be left lying on the floor. Ensuring a safe home and improving caregivers’ consciousness regarding choking risks will enormously lessen the occurrence of choking incidents among children.
Eliminating choking hazards at their very essence is about implementing the required norms of behavior, especially in the areas of the household where children are situated. Ensure that children do not have easy access to small items, including toys that have components that can be detached, buttons, and coins. Check toys for damage as they will wear out, and also make sure there is no deviation in the purchase according to the age limits. Promote healthy practices concerning food by encouraging children to cut food into small sizes and ensuring that the intake of a particular food with more significant risks, such as nuts, large chunks of fruit, apples, and hard candy, is avoided. Ensure children do not watch TV or run while eating, and supervise their meals. Moreover, always keep the house tidy to prevent children from using and swallowing inappropriate objects that may be left lying on the floor. Ensuring a safe home and improving caregivers’ consciousness regarding choking risks will enormously lessen the occurrence of choking incidents among children.
Identifying and Reducing Small Objects Risks
It is imperative to be on the lookout for constantly and have measures in place to protect children where small objects, potentially harmful, might be present. She explains that anything the size of a part that could fit into a roll of toilet paper, magnates, batteries, toy sections, or even household products should be interpreted as a choking hazard. Regular and comprehensive checking of the house is necessary to keep such items out of reach of children. Advanced child-proofing techniques, such as locking up loose objects or locked drawers, have considerably reduced accidents. Children and caregivers should be informed of the risk such small parts pose and what to do if small objects are choked. For example, this calls for children to be consistently observed when playing so that it is not missed if they swallow a dangerous object. Integrating these activities into regular schedules will help take more extraordinary precautions against the negative impact of small objects, leading to safer environments for the children.Teaching Children to Chew Properly
To cultivate proper eating habits in the children, I start by chewing well and swallowing only after the food has been chewed properly. I then introduce them to various food textures, starting with the softer ones and moving on to the harder ones, depending on the texture they can manage. I encourage them to eat relaxed to help build the correct chewing habit. I also add foods that integrate chewing from both sides of the mouth to assist in muscular development and coordination. To help the children with their chewing learning experience, I praise them for their efforts towards chewing well so they find the situation pleasant. With a generally enjoyable experience for the child, I can enhance their chewing habits, ensuring oral health and safety.Supervising Meal and Playtime for Child Safety
What Resources Are Available from the American Red Cross?
 The American Red Cross has a range of resources to improve safety and readiness in various settings. These resources include First Aid, CPR, and AED courses that help people learn how to save lives during emergencies. The organization also provides Mobile Apps at no charge that provide essential information in an emergency and guide users through the most common first aid scenarios. More so, the Red Cross has a collection of online guides and resources on topics ranging from preparing for disasters to water safety for families and communities, which help mitigate risk and build resilience. These materials are in place quickly and are intended to make people feel less scared and more confident to take decisive action during an emergency.
The American Red Cross has a range of resources to improve safety and readiness in various settings. These resources include First Aid, CPR, and AED courses that help people learn how to save lives during emergencies. The organization also provides Mobile Apps at no charge that provide essential information in an emergency and guide users through the most common first aid scenarios. More so, the Red Cross has a collection of online guides and resources on topics ranging from preparing for disasters to water safety for families and communities, which help mitigate risk and build resilience. These materials are in place quickly and are intended to make people feel less scared and more confident to take decisive action during an emergency.
Learning First Aid for Choking through Courses
Gaining knowledge of first aid skills intended for emergencies, such as choking, is worthwhile. Numerous governing bodies, notably the American Red Cross Society and other bodies such as the American Association for Cardiovascular and Pulmonary Rehabilitation and St. John Ambulance, provide relevant workshops to remedy choking issues. The courses in question tend to be holistic as they focus on theoretical concepts and the practical side of things, for instance, maneuvers such as the Heimlich, where backward and inward pressure is applied to the stomach, back blows, and chest thrusts. This relevant training is crucial in ensuring the participants recognize the distinction between adult and child choking and the correct course of action. As they have learned during the training, the individuals can gauge the severity of the choking episodes and react, thus providing civil and locational security. Also, addressing the in-person and online approaches ensures that these skills are taught to many.How to Stay Prepared for Choking Emergencies
Many approaches can be used in dealing with choking situations; however, being informed and having the right attitude are essential. First, ensure that you take proper certified first aid courses with appropriate use of the heinous maneuver, back blows, and chest thrusts, as these focus on the key points, as the American Red Cross and the American Heart Association can assist in that regard. One can never ignore the fact that there is about a shot, and that is why the application of adult choking and child choking focuses on what can alleviate the situation. Apart from formal education, it may also be essential to furnish the background with appropriate facilities. A first-aid kit containing essential antiseptics, medical scissors, and a typical list of instructions is invaluable during unforeseen circumstances. Ideally, these kits should be placed in high-traffic areas like kitchens, playrooms, and cars. Equally important is the assistance from mobile apps incredibly dedicated to this purpose, which not only provide triage but also help reinforce memorized sequences of actions with the aid of the app on a real-time basis. Regular review sessions and simulations with family or close friends also help strengthen the choking emergency protocols so that response sequences are smooth and well-timed. Overall, preparation improves the time it takes to get someone’s attention during choking episodes and increases the possibility of doing something beneficial.References
Frequently Asked Questions (FAQ)
Q: What is the first step to help a choking child?
A: The first step is to shout for help and ensure someone calls emergency medical services while you start helping the choking child.
Q: How should you help a choking infant under 1 year?
A: For a choking infant under 1 year, position the infant face down along your forearm, supporting their head. Use the heel of your hand to give five back blows between the shoulder blades. If the object doesn't come out, turn the baby face up and give five chest compressions using two fingers on the center of the chest.
Q: What steps help a child older than 1 year who is choking?
A: For a child older than 1 year, stand or kneel behind the child and wrap your arms around their waist. Make a fist with one hand and place it above the child's navel. Grasp the fist with your other hand and give quick, upward abdominal thrusts until the object comes out or the child can breathe.
Q: How can you prevent pushing the object more profoundly in a child's airway?
A: Avoid blindly sweeping a finger in the child's mouth as it can push the object deeper. Only attempt to remove the object if you can see it.
Q: What should you do if the child is still choking after initial attempts?
A: Continue with cycles of five back blows and five abdominal thrusts until the object comes out or emergency medical help arrives. If the child becomes unconscious, start CPR.
Q: How do you perform CPR on a child who is choking and becomes unconscious?
A: Start with chest compressions. Give 30 chest compressions using the heel of your hand for a child over 1 year, then provide two rescue breaths. Continue CPR until the child starts breathing or emergency medical personnel take over.
Q: When should you call for emergency medical help during a choking incident?
A: Call for emergency medical help immediately if the child can't breathe, cough, or make sounds and if initial attempts to dislodge the object are unsuccessful.
Q: How can you recognize if a child might be choking?
A: Signs that a child might be choking include inability to cough or speak, difficulty breathing, and clutching their throat. The child may also appear panicked or unable to cry.
Q: What is the importance of using the heel of your hand during first aid for a choking child?
A: The heel of your hand provides the strength needed for effective back blows, which help dislodge the object from the child's airway.














 Login with Google
Login with Google Login with Facebook
Login with Facebook