Knowing how to save human life with appropriate techniques is of utmost importance so as to guarantee the protection of children. For instance, one skill that would qualify as critical would be how to respond when a child has a choking episode. The pediatric choking algorithm offers consistent and clear instructions regarding the management of a supervisory episode. This article intends to give relevant information and practical tips to the key stakeholders including the caregivers, educators, and parents or anyone who will be tasked with the childcare duties. With a basic understanding of the pediatric choking algorithm, peoples’ consciousness can be prepared in such a manner that they can respond very quickly and accurately in such emergencies. Such a response can determine the difference between an individual surviving or succumbing to the situation.
 The obstruction of foreign objects can provoke children to display specific symptoms depending on the severity of their choke. Children who are suffering from an obstruction may present with difficulty swallowing air, wheezing, or, in more advanced cases, having no air passage at all. A cough may allow a sense of breath to sneak out or, inversely, may not get the child to breathe, both symptoms indicating a strong blockage. Thus, wheezing or audible stridor may be some other symptoms. Distress may also be suspected by all the gripping seen around their own throat. In worse cases, there tends to be lip tint or even skin color known as cyanosis that is due to oxygen deficiency. These signs, if ever perceived by a person, can be quite crucial as they inform a person to step into action at the earliest before things can deteriorate into something much worse.
The obstruction of foreign objects can provoke children to display specific symptoms depending on the severity of their choke. Children who are suffering from an obstruction may present with difficulty swallowing air, wheezing, or, in more advanced cases, having no air passage at all. A cough may allow a sense of breath to sneak out or, inversely, may not get the child to breathe, both symptoms indicating a strong blockage. Thus, wheezing or audible stridor may be some other symptoms. Distress may also be suspected by all the gripping seen around their own throat. In worse cases, there tends to be lip tint or even skin color known as cyanosis that is due to oxygen deficiency. These signs, if ever perceived by a person, can be quite crucial as they inform a person to step into action at the earliest before things can deteriorate into something much worse.
 A choking child can be extremely frightful, and to help them, one needs to first perform the following steps so that stands a good chance of clearing the obstruction in their airway:
A choking child can be extremely frightful, and to help them, one needs to first perform the following steps so that stands a good chance of clearing the obstruction in their airway:
 It is imperative to know how to do Basic Life Support for a child who is choked. In cases when the child is not able to breathe, cry, or make any noise, it is important to act immediately.
To begin with, begin with five firm strikes to the back. Move behind the child with one arm around the chest and lean the child’s body forward while standing. Then, use the heel of the palm on the other hand to strike the child firmly in the middle between both shoulder blades. If back blows do not clear the obstruction, proceed with abdominal thrusts. With the child behind you, place your fist above the belly button, hold it with the other hand, and thrust it straight up. Alternate giving back slaps and abdominal thrusts until the foreign body is either coughed out or the child is unconscious, in which case heart massage is to be employed. In situations like these, remaining calm and remembering these steps could prove to be crucial.
It is imperative to know how to do Basic Life Support for a child who is choked. In cases when the child is not able to breathe, cry, or make any noise, it is important to act immediately.
To begin with, begin with five firm strikes to the back. Move behind the child with one arm around the chest and lean the child’s body forward while standing. Then, use the heel of the palm on the other hand to strike the child firmly in the middle between both shoulder blades. If back blows do not clear the obstruction, proceed with abdominal thrusts. With the child behind you, place your fist above the belly button, hold it with the other hand, and thrust it straight up. Alternate giving back slaps and abdominal thrusts until the foreign body is either coughed out or the child is unconscious, in which case heart massage is to be employed. In situations like these, remaining calm and remembering these steps could prove to be crucial.
 The differences between choking situations in infants and in older children are the airway anatomy and the choking response strategy. Infants’ airways are inherently smaller, and with their poor chewing skills, they are prone to choking on small-sized items like small pieces of liquid and foods like grapes or nuts that can easily become lodged in their airways. The protocol for infants who choke involves five back slaps followed by chin-up thrusts while the baby’s neck is held tilted down. On the other hand, older children may choke on larger pieces of food or objects but are able to follow prompts when instructed to cough forcefully. Other choking responses require abdominal thrusts, which are popularly referred to as the Heimlich maneuver. They must also not apply extreme pressure in order not to cause harm. It is important for caregivers to understand these variations so that timely and appropriate age-specific assistance is provided.
The differences between choking situations in infants and in older children are the airway anatomy and the choking response strategy. Infants’ airways are inherently smaller, and with their poor chewing skills, they are prone to choking on small-sized items like small pieces of liquid and foods like grapes or nuts that can easily become lodged in their airways. The protocol for infants who choke involves five back slaps followed by chin-up thrusts while the baby’s neck is held tilted down. On the other hand, older children may choke on larger pieces of food or objects but are able to follow prompts when instructed to cough forcefully. Other choking responses require abdominal thrusts, which are popularly referred to as the Heimlich maneuver. They must also not apply extreme pressure in order not to cause harm. It is important for caregivers to understand these variations so that timely and appropriate age-specific assistance is provided.
 Elementary first aid training educates people with life-saving skills. It makes certain that the vital seconds after an accident or a medical emergency are not wasted and basic procedures like CPR, clotting the blood of the victim, or helping a person who is choking, which can be done for the time being until the real deal doctors show up, can be carried on. Empowered with training directs quick actions so that there is no time to panic, which the trained are likely to do. With such training, a community is more robust, and the probability of favorable results in crisis situations is high.
Elementary first aid training educates people with life-saving skills. It makes certain that the vital seconds after an accident or a medical emergency are not wasted and basic procedures like CPR, clotting the blood of the victim, or helping a person who is choking, which can be done for the time being until the real deal doctors show up, can be carried on. Empowered with training directs quick actions so that there is no time to panic, which the trained are likely to do. With such training, a community is more robust, and the probability of favorable results in crisis situations is high.
What Are the Signs and Symptoms of Pediatric Choking?
 The obstruction of foreign objects can provoke children to display specific symptoms depending on the severity of their choke. Children who are suffering from an obstruction may present with difficulty swallowing air, wheezing, or, in more advanced cases, having no air passage at all. A cough may allow a sense of breath to sneak out or, inversely, may not get the child to breathe, both symptoms indicating a strong blockage. Thus, wheezing or audible stridor may be some other symptoms. Distress may also be suspected by all the gripping seen around their own throat. In worse cases, there tends to be lip tint or even skin color known as cyanosis that is due to oxygen deficiency. These signs, if ever perceived by a person, can be quite crucial as they inform a person to step into action at the earliest before things can deteriorate into something much worse.
The obstruction of foreign objects can provoke children to display specific symptoms depending on the severity of their choke. Children who are suffering from an obstruction may present with difficulty swallowing air, wheezing, or, in more advanced cases, having no air passage at all. A cough may allow a sense of breath to sneak out or, inversely, may not get the child to breathe, both symptoms indicating a strong blockage. Thus, wheezing or audible stridor may be some other symptoms. Distress may also be suspected by all the gripping seen around their own throat. In worse cases, there tends to be lip tint or even skin color known as cyanosis that is due to oxygen deficiency. These signs, if ever perceived by a person, can be quite crucial as they inform a person to step into action at the earliest before things can deteriorate into something much worse.
Recognizing Airway Obstruction
Identifying and treating an airway obstruction in young children, which can lead to choking, is something I have learned how to deal with after a lot of experience. In such cases, my first action is always to examine how the child breathes and record whether he makes any sounds. If a child can neither speak nor cry or make sounds, then that is a total obstruction, but if a child gasps, coughs, or wheezes, then that indicates a partial obstruction. The child’s behavioral changes are also dealt with in a similar manner; a choking sign like the hands held around the throat is a good cue. Excessive salivation and poor coughing are also important. Such symptoms, if diagnosed quickly, help me to take effective measures as I follow the pediatric choking algorithm at this point to remove the obstruction and secure the airway.Signs a Child May Be Unable to Breathe
I want to emphasize that recognizing the signs of a child who is likely to be in respiratory distress is extremely important, and here is what to look out for:- Breathing Difficulties:Maori- Rogers (n/d) points out that if a child has some impediment in breathing regularly than there is a cause for concern. Stridor is characterized as a raspy and high pitched sound and may indicate that a possible obstruction exists in the child’s larynx or trachea.
- Inability to Make Sounds: The duh screening is one test that assesses whether or not a child possesses airway skills. If a child is unable to speak, cry or make any noise, it might signal that there is a complete obstruction in their airway. Instant measures to ease the symptoms ought to be taken.
- Universal Choking Signal: If a child is found doing this, it is a sure sign of choking, especially if the child is holding her throat or chest; the child is possibly experiencing choking.
- Cyanosis: Lip and nail bed cyanosis in infants indicates a serious lung problem; development of a pale bluish hue of the child’s lips or skin, throat and neck which refers to lack of oxygenation and is a sign that warrants further investigation the child’s airway may be fully occluded.
- Gagging or Coughing: In circumstances where part of the airway is blocked, this is referred to as an obstruction, a child may be able tele cough or gag with support. Notwithstanding if an airway cough is ineffective, the
- General Agitation or Panic:A child can’t seem to comprehend much, and because they are theoretically unsophisticated, they can be easily shaken up when they go through an episode where they are unable to breathe firmly, leading to them exhibiting panic and distress or moving around vigorously to indicate their discomfort.
Identifying a Completely Blocked Airway
A child who has a respiratory emergency consisting of a completely blocked airway can be recognized by the signs that have been present on him or her before. In simpler terms, it can be diagnosed like this:- Inability to Breathe: The child can also seem to be very breathless. They will not perform any inhalation which is perilous.
- No Sounds: A completely blocked child’s airway makes it impossible for the child to cry, speak or even make a sound. The reason for this is, no air would enter or leave the lungs contributing to this silence.
- Clutching at the Throat: There are times when a child will place his hands on the throat reflexively. It’s the same gesture people make when they are choking – only it is more universal.
- Change in Color (Cyanosis): Airway obstruction means no oxygen is getting to the body, resulting in a bluish coloration of the lips or face. This is another crucial indication that the body has not been receiving sufficient oxygen.
- Panicked or Distressed Movements: Due to the airways being obstructed, a child can start to panic and exhibit unusual movements and magnification of very scared and alarming behavior.
How to Provide First Aid for a Choking Child?
 A choking child can be extremely frightful, and to help them, one needs to first perform the following steps so that stands a good chance of clearing the obstruction in their airway:
A choking child can be extremely frightful, and to help them, one needs to first perform the following steps so that stands a good chance of clearing the obstruction in their airway:
- Encourage Coughing: If the patient is able to cough, advise them to continue in order to clear the offending object.
- Perform Back Blows: Stand behind the patient, hold them in a forward position, and using the heel of your palm deliver not more than 5 sharp blows between the shoulder blades.
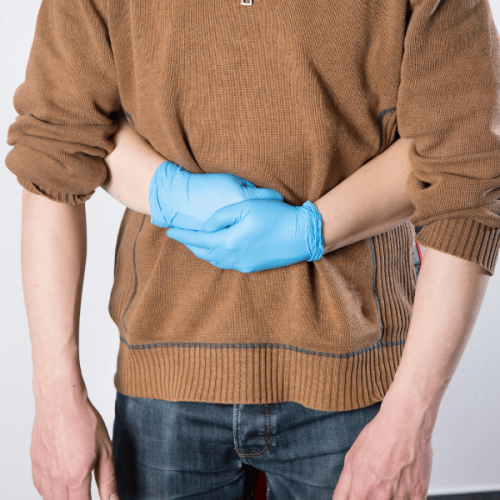
- Execute Abdominal Thrusts (Heimlich Maneuver): If the blockage has not cleared even after back blows, stand behind the person, make one fist just above their navel, clasp that fist with the opposite hand, and deliver not more than five thrusts of this fist in a quick, vertical direction towards the patient’s head.
- Alternate Between Back Blows and Abdominal Thrusts: Repeat the cycle of back blows for five and abdominal thrusts for five and continue to do so until the object is removed or the child is not responding.
- Call Emergency Services: If the child is not responsive or unconscious then one should call services for emergency and start CPR if the person is trained.
Administering Back Blows and Abdominal Thrusts
Having dealt with several emergency cases and administering first aid, I can deal with a clinical scenario involving children choking, and I know how critical proper back blows and abdominal thrusts are. These maneuvers, when done correctly, are capable of opening up the airway. From my own experience, I know that the trick is to do them accurately, but more importantly, to do them gently. For that reason, when performing back blows, the child must be sufficiently forward so that gravity can help clear the airway. In addition, such methods also fundamentally alter the chances of success: proper placement of the hands just above the navel during an upward shove increases the odds a great deal. These techniques, in conjunction with remaining calm during the entire process, are not only beneficial in performing the maneuvers but also have a calming effect on the child, thus managing the child’s emotional state during panic.Clearing Airway Obstructions
I can guarantee that effective clearing of airway obstructions depends on a proper definition of all crucial parameters involved. These are as follows:- Proper Technique: A proper implementation of back blows, abdominal thrusts and other relevant advanced or basic techniques is very productive in freeing someone from an obstruction. It has been also found that if these techniques are properly ordered in regard to the force that is to be applied and where the pressure point is to be located they tend to work better than expected.
- Child's Physical State: It’s crucial to evaluate the child’s physical state before you proceed with any of the procedures. If the child is alert and is able to speak or cough self aid is always the better approach, in this case, supplement that action with a cough or encouragement to cough in order to bring the obstruction out spontaneously.
- Leaning Forward: While giving back blows ensure that the child is in a standing position with the child leaning forward. That position allows the use of gravity to get the object out.
- Hand Positioning for Abdominal Thrusts: Abdominal thrusts require your hands to be positioned correctly which is 4 fingers including the thumb above the navel all the firmly pulled up quickly.
- Calm Demeanor: It is very important to remain calm and composed during the entire process. Such an attitude will not only bolster your technique but will also help calm the child, making them feel secure and assured that everything will be alright.
Steps When a Child Becomes Unresponsive
The goal of this exercise is to enhance healthcare professionals' understanding of the use of airway management techniques in children who become unconscious from airway obstruction. Furthermore, let us outline the theoretical process into simple steps so as to make it possible for you to get as prepared as possible:- Call for Help: The first step is to undertake the effort of salvation and calling emergency services in the first place. The earlier the professional medical help has been initiated the better it is.
- Check for Responsiveness: Lightly tap the child and shout to see if he or she responds. If no response is obtained, then continue with the child’s management.
- Open the Airway: With the child lying on the back, tilt the child’s head back gently to ensure the airway is clear. This aids in determining whether there is spontaneous respiration by the child.
- Check Breathing: Instruct the witness to remember to look, listen, and feel, for breath for about 10 seconds maximum. If the child is not breathing at all or only gasping breathing, give CPR.
- Initiate CPR:
- Compressions First: Place the heel of the other hand on the upper half of the child’s sternum and elbow the other hand into the palm of the lower one. Push down hard and at a fast rate of around 100 – 120 compressions per minute. Give 30 compressions then, give two rescue breaths.
- Rescue Breaths: If the head is not already in the right position, turn the nose so that the child will be able to breathe out and forward. Adjust the nose under the pressure of a mouth or theirs and breathe the kid’s chest for a single or 1 second. Observe for the chest to move. If the chest does not seem to move, use the chin to tilt the head back and attempt again.
- Continue Cycle: Getting Started: Continue performing 30 compressions and two rescue breaths until the paramedics arrive OR JAS starts breathing.
How to Perform BLS for Pediatric Choking?
 It is imperative to know how to do Basic Life Support for a child who is choked. In cases when the child is not able to breathe, cry, or make any noise, it is important to act immediately.
To begin with, begin with five firm strikes to the back. Move behind the child with one arm around the chest and lean the child’s body forward while standing. Then, use the heel of the palm on the other hand to strike the child firmly in the middle between both shoulder blades. If back blows do not clear the obstruction, proceed with abdominal thrusts. With the child behind you, place your fist above the belly button, hold it with the other hand, and thrust it straight up. Alternate giving back slaps and abdominal thrusts until the foreign body is either coughed out or the child is unconscious, in which case heart massage is to be employed. In situations like these, remaining calm and remembering these steps could prove to be crucial.
It is imperative to know how to do Basic Life Support for a child who is choked. In cases when the child is not able to breathe, cry, or make any noise, it is important to act immediately.
To begin with, begin with five firm strikes to the back. Move behind the child with one arm around the chest and lean the child’s body forward while standing. Then, use the heel of the palm on the other hand to strike the child firmly in the middle between both shoulder blades. If back blows do not clear the obstruction, proceed with abdominal thrusts. With the child behind you, place your fist above the belly button, hold it with the other hand, and thrust it straight up. Alternate giving back slaps and abdominal thrusts until the foreign body is either coughed out or the child is unconscious, in which case heart massage is to be employed. In situations like these, remaining calm and remembering these steps could prove to be crucial.
Understanding Basic Life Support (BLS)
Basic Life Support (BLS) is a set of emergency procedures designed to restore blood flow and breathing. It is performed according to the tenets of resuscitation, which include the three components: A - airway, B - breathing, and C - circulation. There are proportions in every pediatric case for BLS to be effective. It all starts with a clear airway where rescue breaths are given with chest compressions to pump blood. BLS in children includes the ability to recognize some early signs like choking and unresponsiveness and to take early remedial action by back blows and abdominal thrusts. These procedures need to be well understood by health workers and caregivers as they may have to confront life-threatening issues in children.Performing CPR When a Child Is Unresponsive
I would like to assume the perspective of an experienced practitioner in pediatric emergency care who has seen both high and low-triage patients. In such critical issues, my foremost concern is ensuring the military exercise protocols determine the cause of unresponsiveness in children. Next, I commence to look for breathing; if there is none or if breathing is not normal, then CPR must be started at once – it is not recommended to spend a few seconds looking around at what else can be done. I start with rescue breaths, which have to be given in such a way that the patient’s chest aorta should be visibly disturbed, while I continue with rescue compressions for blood circulation. I firmly apply compressions, assuming roughly one-third of the chest circumference as a depth with a compression rate of 100–120 per minute, with full chest recoil permitted after compressions. I am very few minutes away from possible additional assistance, and if I have been alone for more than two minutes and the source of the emergency has not yet appeared, I will make sure that the emergency apparatus has been contacted. My training is good and more reinforced, so I calm down and make the best out of myself during such life-risking situations.Using an AED on a Child
This essay is in the first-person plural tense. Using the pronoun ‘we’ rather than the preferred ‘I’. As a pediatric expert in emergency care, people often have the expectation of showing them the appropriate use of an Automated External Shock (AED) for a child. Most importantly, it must first see if the child’s heart has stopped or become irregular, and that is usually the time that AED can be useful. There are several important stages that you should follow, and the following paragraphs present them simply and clearly.- Assess the Situation: Ensure the child is unresponsive with no normal breathing. If so, call for emergency assistance immediately.
- Turn on the AED: Check the child and ascertain that she/he is unconscious and is not breathing in an adequate manner. If that is the case, seek urgent medical help at once.
- Attach the Pads: Pediatric pads should be used, where possible; they decrease the joules which are supplied to children. Place one pad on the child’s chest upper right region and place the other pad below the left side region over the lower ribs. If pediatric pads are not available, regular pads can be placed but precautions have to be adhered that they do not touch one another.
- Follow Device Prompts: During the analysis phase of the AED's diagnosis, ensure that none of the individuals are in contact with the child.
- Administer Shock if Advised: If the AED shock is prescribed, check that all personnel are away from the child and shock the child with the provided button. It is highly unlikely that the first time any medical practitioner ever uses this device, this medical device will seriously trouble any medical practitioner in how to use it.
- Resume CPR: In all circumstances, make sure that CPR is started up again, this includes chest compressions after any type shock has been given. Always listen to the AED and follow its sounds for when to perform further chest compression and when it is time to check the child’s heart again.
What Are the Differences Between Choking in Infants and Older Children?
 The differences between choking situations in infants and in older children are the airway anatomy and the choking response strategy. Infants’ airways are inherently smaller, and with their poor chewing skills, they are prone to choking on small-sized items like small pieces of liquid and foods like grapes or nuts that can easily become lodged in their airways. The protocol for infants who choke involves five back slaps followed by chin-up thrusts while the baby’s neck is held tilted down. On the other hand, older children may choke on larger pieces of food or objects but are able to follow prompts when instructed to cough forcefully. Other choking responses require abdominal thrusts, which are popularly referred to as the Heimlich maneuver. They must also not apply extreme pressure in order not to cause harm. It is important for caregivers to understand these variations so that timely and appropriate age-specific assistance is provided.
The differences between choking situations in infants and in older children are the airway anatomy and the choking response strategy. Infants’ airways are inherently smaller, and with their poor chewing skills, they are prone to choking on small-sized items like small pieces of liquid and foods like grapes or nuts that can easily become lodged in their airways. The protocol for infants who choke involves five back slaps followed by chin-up thrusts while the baby’s neck is held tilted down. On the other hand, older children may choke on larger pieces of food or objects but are able to follow prompts when instructed to cough forcefully. Other choking responses require abdominal thrusts, which are popularly referred to as the Heimlich maneuver. They must also not apply extreme pressure in order not to cause harm. It is important for caregivers to understand these variations so that timely and appropriate age-specific assistance is provided.
Choking Hazards for Infants
Choking hazards are some things I do not take lightly. Infants are a naturally inquisitive bunch, and during the course of exploring their environment, they will often reach out with their mouths in order to familiarize themselves with an object. This inborn behavior, however, heightens the choking risk. Items such as small buttons, coins, beads, or any other small objects of a kind should never be in the access of an infant as they are extremely dangerous. Foods such as whole grapes, nuts, and popcorn are also alarming since the size and texture alone are enough to almost completely obstruct the airways of infants. A safe environment to me involves understanding these risks and dangers and benchmarking such threats through constant laps around the infant’s environment and diet adjustments where necessary. With these preventive measures in place, the chances of choking incidences can be cut down considerably, thus assuring caregivers of the safety of their charges.Performing Back Blows and Chest Thrusts on Infants
There is a strict sequence of actions that should be done in order and moved to the next step if and only if the previous one did not provide results when conducting back blows and chest emphysema on children under one year. In the procedure, the child is first placed face down on the forearm possessor with the head lower than the body, which is secured by the hand. Then, using the heel of the hand, make five stroking gestures targeted on the right and left backbone undersurface centered in between the two shoulders of the baby. If nothing comes out, the child is rotated over the back while stretching the hand to locate the head lower than the body, and five push-ups are made using the two fingers of the hand placed in the middle of the breastbone. This cycle is continued as long as the infant continues to expel solids until the last sequence in the cycle, where the specialist checks if the airways are blocked, passes, and is obliged to repeat the process if the case persists. These measures can be performed with restraint so that no unnecessary force is exerted on the child, and they will be able to help in a case of choking.How to Support the Infant’s Head and Neck
Perhaps the most important component of an infant’s care is to support their head and neck. In my professional experience, I have learned that whenever an infant is picked up or held, their head should be well supported at all times. With one of your hands, gently support the back of the child's head while the other arm and hand support the child’s neck and back. This approach avoids any sudden action that may likely stress these vulnerable areas. Also, remember to always hold the head and neck of the infant when putting them down on a stable surface so that there is no pressure on these parts until the infant is on a stable surface. However, as the infant develops and the muscles of the neck get stronger, their capacity to hold their own heads will increase, therefore the need for such support will be reduced. However, until that point in time, whenever that cervical load bearing is achieved, you are required to provide support in a gentle manner to avoid stress on the infant’s safe.How Can Proper First Aid Training Help Save Lives?
 Elementary first aid training educates people with life-saving skills. It makes certain that the vital seconds after an accident or a medical emergency are not wasted and basic procedures like CPR, clotting the blood of the victim, or helping a person who is choking, which can be done for the time being until the real deal doctors show up, can be carried on. Empowered with training directs quick actions so that there is no time to panic, which the trained are likely to do. With such training, a community is more robust, and the probability of favorable results in crisis situations is high.
Elementary first aid training educates people with life-saving skills. It makes certain that the vital seconds after an accident or a medical emergency are not wasted and basic procedures like CPR, clotting the blood of the victim, or helping a person who is choking, which can be done for the time being until the real deal doctors show up, can be carried on. Empowered with training directs quick actions so that there is no time to panic, which the trained are likely to do. With such training, a community is more robust, and the probability of favorable results in crisis situations is high.
Learning Steps from the Red Cross
This is a very useful set of skills that must be trained and practiced regularly. First, let's begin with the obvious- it is useful to have a first aid kit with you everywhere. Not all situations require a full on medical evacuation, sometimes the worst that is needed is applying some antiseptic spray and a band-aid. The key here is to be prepared before heading to an event or a gathering, as getting overwhelmed and running through the blood and gore isn't practical. In every event where there is the potential for injury, the best plan is to have a stocked first aid kit. The first aid kit typically includes anti-bacterial wipes, clotting gels like Quick Clot, adhesive dressings, scissors, and gauze. The second precious life-saving first aid skill is learning CPR. Compressions are crucial for portability, where an automatic heart defibrillator is often absent. This knowledge has the potential to change the course of someone's life, as head trauma during a seizure is equally fatal. In short, a heart attack occurs, and this falls within the rule: ‘There is no time to waste; every second is lifesaving. The goal is to always maintain blood circulation, as lasting effects can sadly become irreversible due to deprivation. Thirdly, let's explore how this training ties to community resilience. Imagine if everybody knew what went where in a kitchen and how a knife is used, but none of these people actually knew how to use the several appliances in sequence to prepare. A neighborhood like that sticks out due to its high-risk factor and since everyone is bound to play the role of a villain, amplifying everybody's intrigue for when someone gets injured. In such communities, one would hesitantly find life due to an insane improvement in recovery ratios in situations with plenty of accidents and unfortunate events in general. One can perfect such practical knowledge at the Red Cross. They have a sequence of complete and systematic courses that take you through the entire process, instructionally engineered one step at a time. This is generally what you will be taught:- Assessment Skills: Appraising the gravity of the airline within the ICAO region and addressing which steps of emergency action should be taken.
- CPR and AED Usage: Practicing the technique and rhythm of chest compressions and the operational use of an Automated External Defibrillator.
- Bleeding Management: Methods such as direct pressure and the application of a tourniquet in order to control the bleeding.
- Choking Relief: Procedures such as back slapping and abdominal thrusts which are aimed at removing foreign bodies that are lodged in the airway.
- Minor Injury Treatment: Treating and caring for minor cuts, bruises, sprains, etc., so that the delay in further treatment does not result in any adverse consequences.
Finding First Aid Advice for Parents
In our modern times, parents need first-aid learning resources that are effective and directly aimed at the needs of families. Prominent ONGs such as the Red Cross conduct certified training seminars for parents and other caregivers for choking, fever, and injury for children, among other emergencies. Educational resources are made available through venues such as the Internet and mobile phones, thus enabling parents to be ready for the worst situations. Furthermore, such parents also seek the assistance of medical practitioners to support and put safety measures in place for their children.Reference
- American Red Cross - Adult & Child Choking: Symptoms and First Aid
- NHCPS - Relief Of Choking In Adults, Children & Infants
- Stanford Children's Health - How to Help a Choking Child
Frequently Asked Questions (FAQs)
Q: What is the Pediatric Choking Algorithm?
A: The Pediatric Choking Algorithm is a step-by-step guide designed to help individuals assist a choking child. It outlines the necessary actions to dislodge a foreign object from a child's airway.Q: How can I identify if a child is choking?
A: A child may be choking if they are unable to breathe properly, are coughing weakly or silently, or are unable to speak or cry. They may also clutch their throat or show signs of distress.Q: What should I do first if a child is choking?
A: If the child is coughing forcefully, encourage them to continue coughing. If they are unable to breathe properly or cough, perform five back blows followed by five abdominal thrusts to help dislodge the foreign object.Q: How do I perform back blows on a choking child?
A: Position the child with their head lower than their chest. Using the heel of your hand, give five firm back blows between the child's shoulder blades.Q: How do I perform abdominal thrusts on a child?
A: Stand behind the child and place a fist above the person’s navel in the middle of the abdomen. Hold the first fist with your other hand and press inward and upward toward the child’s abdomen and up toward their chest.Q: When should I call for emergency help if a child is choking?
A: Call 999 or 112 for emergency help if the choking person becomes unresponsive or if you are unable to dislodge the foreign object after several attempts.Q: What should I do if the child becomes unresponsive?
A: If the child becomes unresponsive and not breathing, call 999 or 112 for emergency assistance and begin CPR. Ensure their head is positioned lower than their chest, and avoid putting fingers in the center of their mouth unless you can see a foreign object.Q: Is the procedure for choking in adults different from that for children?
A: Yes, while the basic principles are similar, the procedure for choking in adults involves performing abdominal thrusts instead of back blows and requires adjusting the force according to the adult’s size.Q: How can I learn how to help someone who is choking?
A: Many organizations, such as St John Ambulance, offer courses on first aid and choking procedures. These courses prepare you to respond effectively, and sign up to be prepared and sign up for training can save a life.Q: What are the risks if a foreign object is not quickly removed?
A: If a foreign object is not quickly removed, it can lead to airway obstruction, resulting in the person becoming unresponsive, experiencing cardiac arrest, or even death.1665







 Login with Google
Login with Google Login with Facebook
Login with Facebook