Infant choking is the most frightening medical emergency as it can lead to death, but there are better chances of survival if the problem is identified and treated quickly. This article will illustrate the aspects involving assessing and helping a case of infant choking if the infant is responsive and still at risk. Moreover, there is a need to explain how medical treatment in these cases should be prescribed because there are distinct physical variances in an infant, for instance, narrow airways and undeveloped motor activities.
This article will first discuss how to differentiate between mild to severe airway obstruction and the signs of choking in infants. Then, it will discuss in detail the first aid procedures, like back blows and chest thrusts, that can be applied to an infant who is still responsive. The article will also stress the importance of understanding emergency first aid procedures like calmness, professional help, and the situation when CPR is needed. The information provided in this article will prepare the readers to intervene effectively in the life-threatening situations described.
What to Do If an Infant Is Choking but Responsive?
When an infant chokes but is still alert, one or more observers need to assess the choking level. Without gonna extremes, for many, persistent cough, gag, and, in complicated cases, struggling to breathe high sounds would indicate a weak claim. That is, the airways of their mouths are roughly halfway to being closed, meaning a good amount of oxygen still goes through to the lungs. Conversely, the oxygen-deprived lungs, which cannot produce a cry, cough, and turn the skin or check the color into blue, sound even more dangerous. Additionally, it shows no signs of dominance and seeks help. If oxygen is severely blocked, a prompt rush is required before everything worsens.
How to Administer Back Blows and Chest Thrusts
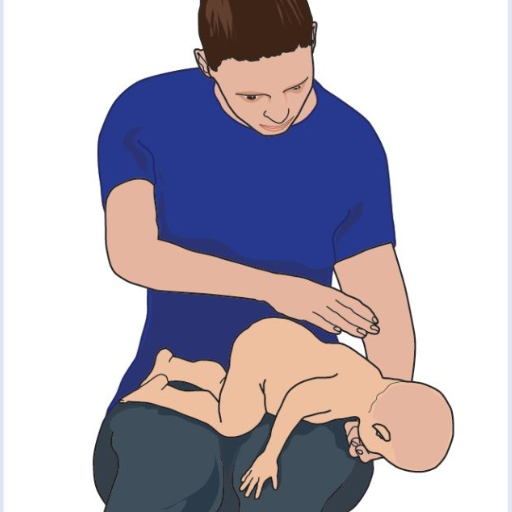
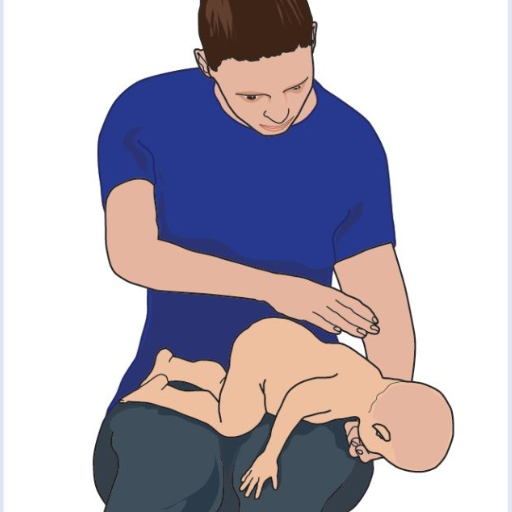
To back blow and thrust my chest, I first place the infant along my forearm while facing downwards, so I have to give support to his/her neck and head with my hand. Then, I proceed to deliver five or fewer strong back blows between the infant's shoulder blades with my other hand, using the heel of my palm, I deliver each smack and I check to see whether or not the obstruction is gone. When the blockage is still obstructing my view. I turn the infant to face me; with the infant resting on my forearm, I place two fingers at the center of the infant’s chest and a line below the nipple. After which, I strike the infant’s chest using controlled pressure five times. I continue this procedure until breathing is okay or stop altogether if the infant starts to lose consciousness. As soon as the infant loses consciousness, the first thing is going to be effective chest compression along with an expert call. Any case relating to the infant is not to be looked into lightly, as problems may be hiding underneath the surface.
Steps to Clear the Airway in a Choking Infant
- Assess the Situation
- Determine if the infant is choking by observing signs such as inability to cry, cough, or breathe or a bluish color around the lips and face. If the infant can cough forcefully, encourage them to continue coughing.
- Position the Infant
- Support the infant’s head and neck with your hand while positioning them face down on your forearm. Rest your forearm on your thigh for stability, ensuring the infant’s head is lower than their chest to utilize gravity in clearing the airway.
- Administer Back Blows
- Using the heel of your hand, deliver five firm back blows between the infant’s shoulder blades. After each back blow, check if the airway obstruction has been cleared. Do not proceed to the next step unless necessary.
- Perform Chest Thrusts
- If the back blows are ineffective, turn the infant face up while supporting the head and neck. Place two fingers at the center of the infant’s chest, just below the nipple line. Administer five quick chest thrusts, compressing the chest about 1.5 inches (4 cm) with a smooth, controlled motion.
- Alternate Interventions
- Keep alternating five back blows and five chest thrusts until the blockage is removed or the infant becomes unresponsive. Regularly check for the object’s removal during the procedure.
- If the Infant Becomes Unresponsive
- If the infant stops responding, call 911 or emergency services immediately. Begin CPR by performing 30 compressions at a rate of 100–120 compressions per minute and delivering two rescue breaths after each cycle. Continue until medical help arrives.
- Seek Medical Attention
- Even if the obstruction is cleared, consult a healthcare professional to ensure no injuries or additional complications resulting from choking or life-saving measures.
Signs and Symptoms of Airway Obstruction
Early identification of an airway blockage is vital for effective management. The symptoms begin to show as per the obstruction's severity, including the following.
- Partial Airway Obstruction Symptoms:
- Wheezing experienced by the patient or high-pitched sounds made during inhalation and expiration or even during recovery is termed stridor.
- Chronic cough that does not go away or may lead to gagging.
- Reduced ability to initiate people’s speaking or problems controlling their voice.
- Strain in breathing, which can be noticed if the ribs or muscles are used while breathing.
- Complete Airway Obstruction Symptoms:
- The patient cannot verbally communicate, cough, or make any audible effort to breathe.
- Breathing itself is absent, but the intention to do so is noted.
- Blue or dark colors show partial suffocation around the lips, face, and fingers.
- Once consciousness is lost due to not breathing for some time, immediate recognition and action are required to solve the problem.
Things To Look Out For:
- Respiratory Rate: During an adult’s breathing cycle, the average should equal twenty-six times each minute. Whenever the number cut-off drops or increases, intervention may be needed.
- Oxygen Saturation: When the SpO₂ is measured, and the number fails to exceed ninety metaphors, immediate steps are needed to prevent infection.
- Heartbeats: If the heart rate beats more than a hundred times in a minute, this may be the body's normal trigger to breathe more.
Combining all these signs into one approach helps air blockage cases a lot.
When Should You Call for Help During an Infant Choking Emergency?

For example, an inability to make noise combined with breathing issues or cyanosis warrants immediate assistance because this baby appears to be suffering from critical airway obstruction. Attempting back blows or chest thrusts repeatedly may work in alleviating the obstruction; however, in case the infant grows unresponsive, it is imperative to contact emergency services right away. This is because, in such situations, it is essential to take precautionary steps to stop the infant from mater a stage of hypertension,n which would increase the chances of cardiac arrest. Even while performing first aid, one has to be sure to look for any professionals who could help during the entire procedure.
Indicators That an Infant Needs Emergency Assistance
When assessing whether an infant requires emergency assistance, look for the following critical indicators:
- Respiratory Distress:
- The infant cannot cry, cough, or produce any sound, indicating a complete airway obstruction.
- Breathing appears labored, with excessive effort, which may include using accessory muscles (noticeable chest retractions or flaring of the nostrils).
- Cyanosis (bluish discoloration of the skin, especially around the lips and face) signals insufficient oxygen levels in the blood.
- Loss of Consciousness:
- The infant becomes unresponsive or exhibits a significant decrease in alertness. This could result from hypoxia due to prolonged obstruction.
- Heart Rate Abnormalities:
- A heart rate exceeding 160 beats per minute (tachycardia) may indicate severe oxygen deficiency.
- Conversely, bradycardia (heart rate dropping below 80 beats per minute in infants aged under one year) is a critical warning sign, as it often precedes cardiac arrest in respiratory emergencies.
- Gasping or Absent Breathing:
- Agonal breathing (sporadic gasps) or complete apnea (absence of breathing) points to a medical emergency requiring immediate intervention.
- Behavioral Changes:
- Sudden lethargy, extreme irritability, or a complete lack of response to stimuli may indicate oxygen deprivation, which can impact brain function.
If any of these signs are present, activate emergency medical services immediately. Simultaneously, initiate infant first aid measures, such as back blows, chest thrusts, or CPR if the infant becomes unresponsive. Continuously monitor the infant closely while awaiting professional care.
Guidelines from the American Red Cross and American Heart Association
I suggest always following clear, evidence-based guidelines developed by the American Red Cross and the American Heart Association when dealing with infant respiratory emergencies; first, Whenever possible, ensure the infant’s airway is open by assuring head tilt while always keeping the neck in the supported position. In case of a lack of airway, commence the breathing maneuver immediately. Place two fingers in the center of the chest directly at nipple level, and start compressions at a speed of 100-120 times per minute, pushing two to three centimeters downwards. After every thirty compressions, recheck the breathing of the infant and, if necessary, give the infant two simulated87 ventilatory movements, but in an ot true sea seduction in order over narrowsairwaysnostrillingauges contains nasopharynges sorsofthetandst.
The boy’s dynamics must “be checked empirically” every two minutes, and chest compression must continue until medical practitioners arrive or the boy breathes naturally again. The way depths, through the mouth or the nose, will be a one-time activity and do not include an individual's regular breathing system. One should never make the mistake of avoiding notification of the Emergency Number as soon as the incident is noticed. These technical instructions remain up to accepted standards, offering the best chances of living through critical situations.
How to Perform CPR if the Infant Becomes Unresponsive?

If an infant becomes unresponsive, it is essential to act promptly and composedly. Start by assessing the surroundings to ensure they are safe. Proceed to check the infant's responsiveness by gently tapping the child and calling his/her name. In cases where the infant does not respond or make any sounds, report the case or hand the responsibility to someone close to you and get them to report it.
Attach the infant to a firm surface and begin CPR. To the best of one's ability, remove obstacles from the airway by slightly tilting the head back and lifting the chin. For 10 seconds or less, try to assess if the patient is breathing. If the patient or infant does not respond to breathing for more than gasps, perform two gentle rescue breaths. This can be done quickly by forming a seal around the infant’s mouth and nose and ensuring chest rise occurs.
As an advancement, place two fingers at the middle of the patient’s chest (infant in this case) across the nipple line and begin to compress the chest. Focus majorly on the depth of around 1.5 inches (4 cm) 30 times or until you can get a fast and steady rate between 100 to 120 compressions, and do not forget to alternate. If the patient still has trouble recovering, do not stop until an emergency responder arrives. Always ensure practices are current with organizations such as the AHA or Red Cross concerning specific approaches.
Steps to Begin CPR on a Choking Infant
- Assess the situation—First, I would establish whether or not the infant in question is unresponsive and choking. If the infant cannot cough, cry, or breathe, I would promptly take action to remove the obstruction.
- Call for help—My first step would be to notify the relevant authorities or to request that anyone nearby make that call while I prepare for assistance.
- Alternate back slaps and chest thrusts - I would assist the infant in the following way: Try holding the infant face down across your forearm while securing the infant’s head. Then, administer five back slaps across the shoulder blades using your palm. If the aforementioned does not work, this process is to be undergone until the emergency staff rescues a patient from having his or her airway clogged. Furthermore, with the child on his or her back, I would move the two fingers in place below the nipple line to the center of the infant’s chest and deliver as many as five chest thrusts. This clearing method includes ‘back slaps’ during which five attempts to clear the upper body are made before proceeding to do the same with five thrusts.
- Begin CPR if unresponsive - It is equally important to note that only once paramedics have arrived can one begin to administer compressions and thrusts without worrying about the infant choking again. In the case where an infant does choke and turns unresponsive, one can place the child on a hard surface and initiate CPR while notifying emergency personnel. CPR methods of recovery involve giving two breaths followed by thirty compressions, during which time one could try to rule out instances of the ailment getting cured.
- Eliminate any apparent barriers—In the course of mouth-to-mouth resuscitation, I try to determine whether an object exists in the airway. If so, I try to remove it from the person’s mouth using gentle finger movements, but only when the object can be sighted.
How to Hold the Infant Correctly During CPR
While doing CPR on an infant, I try to remember to perform it correctly to be of help. I lay the infant on its back, on a firm and level surface, placing the mandible slightly forward to clear the airway but not too far to strain the neck. Another pair of fingers is placed on the nipple line, and gentle pressure is applied to the chest to deliver compressions. The rate of compressions is between 100 and 120, and the average depth is 1.5 inches. If I wish to give out some breath for the infant, I press my mouth thoroughly around the nose and mouth of the baby and blow a little air into the mouth. I also pay great attention to the baby's responses and breathing and alter what I do depending on what I find.
Understanding Chest Compressions for an Infant
During cardiac arrest, I apply the proper technique while pushing the baby's chest in the center below the nipple line. Two fingers can achieve that. My rate of compressions is a steady 100 to 120, at least 1.5 inches deep, until the baby starts reacting. Breaths are equally critical. Oxygen can be delivered by sealing her nose and mouth and providing gentle breaths that will allow the chest to rise. I keep looking at the infants, and depending upon their reactions, breathing, movement, or the lack thereof, I would react differently, too.
What Are Common Choking Hazards for Infants and Toddlers?

Little, firm, or spherical foodstuffs, such as hot dog slices, raw vegetables, popcorn, nuts, or grapes, are hazardous to infants' and toddlers' health. Also, there are a number of inhalation risks, including buttons, small coins, balloons, and balloon pieces. Children’s food should always be appropriately cut into small pieces, and toys that are not recommended for their age should be avoided. Children should not be left unattended while eating or playing to avoid inhalation accidents.
Identifying Small Objects That Pose Risks
We must first consider small objects' size, shape, and material composition. The church organization's consumer product safety guidelines define choking objects as fitting entirely into a cylinder whose diameter is one point, twenty-five inches, and length is two point two five inches. This is seemingly the measurement depicting three the fua of a two-year-old animal. Of great concern, the board reported being low-rounded objects, like marbles or balls whose diameter is less than one andro seven eighths all-schooling ou dai, i.e., ano sak respin. Furthermore, classified objects included balloon pieces or any other plastic material that is easily breakable. These parameters, well adhered to with regular house controls, drastically reduce the risk of choking.
Preventive Measures to Avoid Choking in Infants
The child is engaged in many activities and puts many things in the mouth; thus, to avoid choking, I constantly struggle to ensure that they do not get access to small items such as toys, buttons, and coins. Furthermore, I try my level best to classify suitable toys for children regarding their age as recommended guidelines are pretty standard as significant ‘components’ are designed to inhibit swallowing; this would imply any standard about components would mean, at a minimum, all components over 1.75 inches (44.4 mm) in diameter. During family meals, I have developed the habit of slicing foods such as grapes and hot dogs into minuscule portions, less than six millimeters in any direction, as it reduces the chances of a child choking on the food. Moreover, I make it a point to avoid giving kids food items that contain popcorn, nuts, and hard candies, as all of these are known to be choking hazards for children. Trying to watch the child constantly while keeping them within safe guidelines for the environment, such as the rules set by the Consumer Product Safety Commission whenever the child is playing or eating, helps avoid infant choking. Regular touch-up maintenance of swept surfaces around the house to search for possible hidden dangers also assists in making them safer.
Why Is Infant CPR Training Essential for Parents and Caregivers?

CPR courses, in general, and Infant CPR courses, in particular, are vital for parents and carers so that they can know how to help their child in critical situations, such as when the child is choking or suffers from cardiac arrest. Conversely, infants are subjected to this danger because of their small airways and developing systems, which all require enhancement. Those trained can administer effective chest compression and rescue breath, keeping the brain alive and the body stable until the medical experts arrive. Furthermore, undertaking CPR improves the level of trust, decreases the level of anxiety, and ensures that the caregivers are always in a position to act within the most critical moments, possibly saving the life of such an infant.
Benefits of First Aid and CPR Training Services
First Aid and CPR training services provide individuals with life-saving skills and a structured response plan during medical emergencies. These services improve survival rates, reduce injury severity, and enhance recovery outcomes. Key benefits include:
- Immediate Response to Emergencies
Training equips participants with the ability to respond quickly and effectively to critical situations, such as cardiac arrest, choking, or severe bleeding, where every second counts. For example, performing proper CPR can double or even triple the chances of survival for individuals experiencing cardiac arrest, as per guidelines from the American Heart Association (AHA).
- Reduction in Health Complications
Proper application of first aid techniques, such as wound care, splinting, or applying compression, minimizes the risk of infection or long-term damage. CPR ensures the continued circulation of oxygen-rich blood to vital organs, maintaining organ function until advanced medical care is available.
- Compliance with Safety Standards
Many organizations and workplaces mandate training to comply with OSHA (Occupational Safety and Health Administration) standards, ensuring employees can effectively handle workplace injuries. Certification often involves assessments to meet these regulatory requirements.
- Hands-On Practice and Confidence Building
Training sessions frequently utilize advanced equipment, such as CPR manikins, AED (Automated External Defibrillator) simulators, and real-time feedback systems. For instance, CPR compressions are typically taught at a rate of 100-120 compressions per minute at a depth of 2 inches for adults, ensuring technique accuracy during practice.
- Prevention of Escalation in Critical Situations
By mastering techniques like the Heimlich maneuver for choking or RICE (Rest, Ice, Compression, Elevation) for injuries, trained individuals can effectively stabilize a victim and prevent the condition from worsening before emergency services intervene.
- Enhanced Community and Workplace Safety
More trained individuals within a community or workplace significantly increase the collective preparedness for unexpected emergencies, creating a safer environment for everyone.
These training services save lives and foster a more profound sense of responsibility and readiness among participants, ensuring they can make critical, informed decisions under pressure.
Where to Find Infant CPR and First Aid Training Programs
While looking up Infant CPR and first aid courses and training, I suggest first looking up the American Red Cross, American Heart Association, and local health centers. Various infant specific basic CPR techniques are demonstrated through videos and classes provided by the American Red Cross. Furthermore, local branches deliver learning on pediatric first aid and CPR provided by the American Heart Association. Also, due to the prevalence of nursing mothers within the community, community health centers and hospitals hold certified training sessions for caregivers and parents that would be easy to find for most families.
References
Choking Respiratory tract ThoraxFrequently Asked Questions (FAQ)
Q: What should I do if I suspect an infant is choking?
A: If you suspect an infant is choking, immediately assess if the infant is coughing forcefully or if the infant stops breathing. If coughing, encourage it, as it's the best way to clear the airway. You should begin choking first aid if the infant stops breathing or coughing.Q: How do I perform choking first aid on an infant?
A: Choking first aid for an infant involves delivering five back blows followed by five chest thrusts. Hold the infant face-down along your forearm, supporting the infant’s head and neck with your hand. Using the heel of your free hand, give up to 5 quick, forceful back blows between the infant’s shoulder blades. Then, turn the infant face-up, with the infant's head lower than the chest, and give five chest thrusts using two fingers in the center of the infant’s chest.Q: How do I hold the infant during choking first aid?
A: Hold the infant's chest in your hand and rest the back of the infant's head on your forearm. Place the infant face-down along your forearm, resting on your thigh, ensuring the infant’s head is lower than the body.Q: What if the object does not come out after back blows and chest thrusts?
A: If the object does not come out after performing five back blows followed by five chest thrusts, repeat the sequence. Continue alternating between back blows and chest thrusts until the object is expelled or the infant becomes unconscious.Q: Can I see the object that’s causing the infant to choke?
A: Never perform a blind finger sweep. Only attempt to remove the object if you can see the object in the infant's mouth.Q: What should I do if the infant becomes unconscious?
A: If the infant becomes unconscious, call emergency services and begin CPR (cardiopulmonary resuscitation) immediately. Ensure the airway is open and begin chest compressions, followed by rescue breaths.Q: Are abdominal thrusts suitable for infants?
A: No, abdominal thrusts are not recommended for infants. Instead, use back blows and chest thrusts if the infant is choking.Q: How should I position the infant for chest thrusts?
A: Turn the infant face up, ensuring the infant’s head is lower than the chest. Use two fingers placed just below the nipple line on the infant’s chest to deliver five quick downward chest thrusts.Q: When should I stop performing back blows and chest thrusts?
A: Continue performing back blows and chest thrusts until the object is expelled, and the infant begins to breathe or cough independently, or becomes unconscious.














 Login with Google
Login with Google Login with Facebook
Login with Facebook