
Time is of the essence when a kid is choking, and knowing that this article aims to be the only resource that a parent of a 3-year-old child ever needs in case of accidental choking. It also delves into the circumstances that cause choking, its common factors in young children, and the first action that can be taken if a child is choked. In this way, it aims to provide all parents, caregivers, and guardians with what to do in such circumstances. We discuss interpreting the characteristics of the child when it is partially or wholly choked and essential first-aid measures, which involve slaps on the back and pressure around the belly as the way out to make sure the child does not die from choking. In the end, other ways to ensure no choking occurs or at least to reduce choking hazards are provided, along with when to consult a professional doctor.
What are the First Aid Steps for a Choking Child?

- Assess the Situation
Determine if the child is experiencing a partial or complete airway obstruction. If the child can cough, speak, or breathe, encourage them to continue coughing to expel the object. Do not interfere unless the obstruction worsens.
- Call for Help
If the child cannot breathe, speak, or cry, call emergency services immediately or direct someone else to call while you provide first aid.
- Administer Back Blows
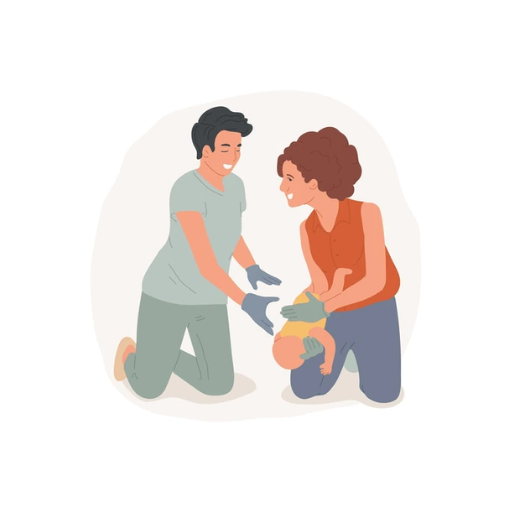
For younger children, position the child face-down over your arm or lap, supporting their head. Using the heel of your hand, deliver up to five firm back blows between the shoulder blades.
- Perform Abdominal Thrusts (Heimlich Maneuver)
For children older than 1 year, stand or kneel behind the child. Place one hand in a fist just above their navel, grasp your fist with the other hand, and give quick upward thrusts. Perform up to 5 abdominal thrusts.
- Alternate Between Back Blows and Abdominal Thrusts
If the object is not expelled, alternate five back blows with five abdominal thrusts until the airway is clear or professional help arrives.
- Perform CPR if Necessary
If the child becomes unresponsive, begin CPR, starting with chest compressions. Check for the object in the mouth before breathing, but avoid blind finger sweeps.
- Seek Medical Attention
Even if the object is expelled, the child should be evaluated by a healthcare professional to ensure no internal injuries or residual complications.
How to Identify if a Child is Choking
To determine whether a child is choking, first analyze if they can cry, cough, or speak. Children who are choking may also have signs like a hand on their throat, inability to make any sound, or strange sounds that are high-pitched while breathing. You might see that their skin is turning pale, blue, or dusky due to oxygen deprivation. If the airway is only slightly blocked, a child might be able to cough or produce some sound indicating there is some airflow. People experiencing a complete blockage will, however, be unable to breathe at all and may also show signs of hysteria. Remember that every second matters- if you notice this sign, do what you must do.
What Techniques Can Dislodge the Object?
When it comes to using evidence-based maneuvers to remove an object from a child’s airway, such maneuvers act in response to the child's age and overall physical condition. These include the following:
- Back Blows
Infants (0-12 months): The child must be put against your forearm with its head lower than its chest, and its neck and head must be completely supported. Give a maximum of five back blows between the infant’s shoulder blades with the heel of your hand.
For children over the 1-year marker, make the child bend over either from a standing or a sitting position and then, with the heel of your palm, give a maximum of five blows to the back.
- Chest Thrusts (Infants)
If back blows do not remove the obstruction, attempt thrusting. While holding the infant’s head lower than their body, pivot the infant onto their back, place two fingers just below the nipple line, and simultaneously compress the chest in the direction towards the body for almost 1.5 inches, thrice.
- Abdominal Thrusts, Better Known as the Heimlich
For children aged one and above, stand behind the child. Then, stand with your arms over the child's waist. Place a fist over the child’s belly button, then grasp your fist with the other hand. Pull in and push up five quick thrusts to the diaphragm, repeating five times in total. However, this procedure should be avoided for children under the age of one as it may lead to severe internal injuries.
4.P proceed as Necessary
Otherwise, carry out the procedure with encouragement; however, it only includes waiting for the object to come out in reverse order. The procedure begins with putting in back blows followed by thrusting the abdominal/chest at a ratio of 5 to 5. However, after losing consciousness, perform CPR right away while still looking for the foreign object.
To avoid further unresolved complications, it is best to seek immediate professional medical attention after a sequence of performing a technique.
When to Perform Back Blows and Abdominal Thrusts
The back blows, and abdominal thrusts are used depending on how critical the choking case is. These actions can be adopted for a child who has difficulty breathing and cannot make a sound or cough. Choking can be first treated by giving the conscious child back blows that are effective when the child is not breathing well. If these measures fail, I will perform the abdominal thrusts. However, I make sure I do not perform abdominal thrusts for infants below a year. The infants are hardly one year old and need different measures for which abdominal thrusts are simplified. When these plans are being carried out, it is wise to call specialists and doctors for the following attention.
How to Help a Child Who is Choking and is Over 3 Years?

If a child more than 3 years of age is choking, follow the following steps:
- Evaluation: Check if the child can cough or talk. If there are acute signs of a blocked airway (e.g., no coughing, breathing, or speaking), quick Attention is required.
- Back Blows: Stand behind the child and back him/her up slightly. Administer not more than five hard chest thrusts at any time to the heel of the palm of one of your hands while the child is slightly bent forward.
- Abdominal Thrusts: Up to five abdominal thrusts can be administered if back blows are ineffective. Push the child towards your stomach while standing behind him/her. Clutch one of the fists just above the navel to the waist region and grasp the first one using the other hand. Hit the child's back inwards and upwards rapidly.
- Continue until required: The combination of back blows and thrusts in the abdomen should be used until the object is ejected or the child is no longer aware of the event.
Place the child on a stable, flat surface if he loses consciousness, and make sure that medical help is on its way while you start CPR. Hear, Any choking incident requires a thorough checkup after the events to eliminate any scope of later side effects.
Steps to Help a Choking Child
When there is a child who is present in front of me and has a choking hazard with the signs of a pacified cough (quiet coughing), inability of them to talk or speak, once I have formed this notion in my head I don’t bother anymore and leap into action. In the beginning, I will do a total of 5 back blows in the area between both of their shoulder blades and use my hand’s heel as a lever, during all of this if I happen not to nut out the object the funny way then I will move on to the next step. This next step will consist of me targeting the area above the belly button with my hand, going through a maximum of 5 motions in which I will quickly go inward and upwards. Once again, if the obstruction does not pass, I will repeat the steps above until it does or until the child stays unresponsive. I will also rapidly position myself for the compression and immediately state that Emergency Assistance is needed if the child does lose consciousness. After everything is over, I will have the child evaluated by the doctor to ensure no complications arise.
Performing Chest Thrusts on a Child
Chest thrusts are an effective alternative to assist a choking child, particularly in cases where abdominal thrusts may be contraindicated, such as in very small children, those who are obese, or if there is a risk of injury. To perform chest thrusts, follow these steps:
- Positioning Yourself and the Child:
- Stand or kneel behind the child, ensuring you have a steady footing and can maintain control during the process.
- Reach around the child to their chest.
- Locating the Chest Compression Area:
- Identify the lower half of the child’s sternum (breastbone), avoiding the xiphoid process (the small, pointed structure at the bottom of the sternum) and the ribs to minimize injury risk.
- Delivering Chest Thrusts:
- Place the heel of one hand on the correct spot on the sternum. If necessary, use your other hand to reinforce the first.
- Deliver up to five firm, quick thrusts directly inward toward the child’s chest, applying pressure sufficient to dislodge the object while being cautious not to cause excessive force that could cause injury.
- Repeating Steps:
- Alternate between five back blows and five chest thrusts until the foreign object is expelled or the child becomes unresponsive.
- If the Child Becomes Unresponsive:
- Lower the child gently to a firm, flat surface and immediately begin CPR.
- Ensure someone calls for emergency assistance.
- Post-Incident Evaluation:
- Once the obstruction is cleared, seek medical attention for the child to check for internal injuries or complications caused by the obstruction or the intervention.
This systematic approach underscores precision and safety, balancing the need for effective obstruction relief with minimizing potential harm to the child. Individuals trained in these techniques should only perform chest thrusts, as incorrect application can exacerbate harm.
When to Call 911 for a Choking Child
In an event where a child finds it hard to breathe while simultaneously being unable to panic or speak, a necessary course of action would be to call 911 immediately. Kids are prone to such situations at times. If there is a respiration pause or accumulated distress, such as the child turning blue or fainting, a sense of help is immediately required. When I find a child calling for help while waiting for the emergency response team to arrive, I contemplate whether I could provide first aid or not, having sufficient training in such matters. As a general rule, I may begin CPR if there is no pulse or discernable breathing, maintain the airway open, and persist in assistance until the object in question is removed or help arrives. With thorough practice and determination, it becomes a habit to maintain calmness and provide the operator with a clear insight into the child's condition.
What to Do if a Child is Unresponsive or Still Choking?

Choking situations can leave a child in a very critical state. If that is the case, position the child on a solid surface while dialing 911. Right after that, CPR can start. This is done by 30 firm pushes on the chest, forming the first side of the compressions. The second part deals with head lifting and attempts to clear the airway through rescue breaths. After removing air, one can remove any blockage only if it is visible after the compressions. It is vital not to use a ‘blind finger.’ Until the child can breathe normally, repeat the steps mentioned above every time. If the child in question is conscious, further actions involve back blows and chest thrusts. Now, what’s important to remember is that all of this is done calmly, as anxiousness affects the level of efficacy. Through proper measures, risk will always be minimized.
Administering CPR to a Child
When providing CPR to a child, the first step involves ensuring that the child is lying on a firm, flat surface and checking whether anyone has contacted emergency services. The response to this query, in all probability, is optimistic. After that, I would place the heel of one hand, locate it in the middle of the child’s chest, and then provide 30 compressions about 2 inches deep while doing it at a rate of about 100-120 every minute. Afterward, I would lift their chin by tilting their head slightly to open their airway and then give two rescue breathing, ensuring their chest rises. Based on their parliamentary structure, I would maintain a rhythm of 30 breaths and two compressions, with the singular aim of exhalation after each cycle. Still, only if obstructions were visible would I remove it. The cycle gets repeated until the child is complete or till medical professionals arrive. Follow the above steps, stay calm, and be ready to make all processes seamless.
How to Shout for Help and Alert Others
Making a loud commotion while making sure that others understand the help request and everybody recognizes the dangers is one of the easiest ways to make sure that the required help is received in the first place. You should always start by examining the nature of the emergency and then try to improve it without worsening the existing circumstances. I would advise that you try to scream “Help! Emergency!” or scream out the name of the person would help you to emphasize that singular person, indeed there is no shortage of people who would do anything to shout out someone’s name. If the circumstances require making the calls to take a second or third, do so to garner some attention.
The first customer that can be called if an emergency happens is still the cell phone, especially calling 911. Providing information in such a situation includes details such as the specific location, the emergency type, the victim's proneness in the location, and the significant details for such circumstances. If the emergency sites are surrounded by rugged sites, textual alternatives or other apps made for these occasions could help.
Emergency signals could come in handy in technical environments or even rural areas. Rescue whistle signals and visual emergency signals, which include using brightly colored objects, do the same thing, and three whistle signals are the norm. If an emergency occurs on the sea or even far away from civilization, emergency flares or mirrors could also prove helpful, which is no question why they exist in the first place. It would only make sense for those rescuers to have emergency procedures that vary from context to context.
Handling a Child Who Becomes Unresponsive
If I am presented with an unresponsive child, the first thing I would do is check the surroundings so that the child and I are both safe. Once that is done, I gently shake the child's shoulder and scream, “Are you OK? Are you able to hear me?” If that does not help, disregarding all the attempts to call the child, I would call for help or inform a bystander to do so while providing them with the location and some context of the issue, if required.
Then, I would assess the child's breathing by relaxing the head back and listening for at least 10 seconds to catch breaths while watching the chest for any movement. If there were no signs of breaths or cough-like breaths, then I would call for action in the form of CPR. For Children's CPR, I follow these technical parameters as recommended by expert guidelines.
- Compression Depth: 5 cm in most children aged 1 to 5 preferably, but it should never go beyond 6 cm.
- Compression Rate: 100 to 120 compressions in a minute.
- Compression-Breath Ratio: In a one-person rescue situation, the ratio is thirty compressive thrusts and two breaths, while in a multi-person rescue situation, it is fifteen compressive thrusts and two breaths.
- Hand Positioning and Pressure: Children of various ages vary in size. Depending on the size, one has to either place one or both of their hand(s) below the mid-portion of the sternum and apply pressure.
To begin, if a child needs CPR, and an Automated External Defibrillator (AED) is within reach, I would first put it on, following the ECG guidelines on how to position the module on the chest. As a reminder, pediatric pads should be utilized if the patient is under eight years old or weighs 25 kg or less. Additionally, Remember to focus on the event's timeline since the person performing CPR should maintain it until help is available or the child starts breathing or moving.
What are the Signs of Choking in Children?
The inability to talk, make sounds, or even breathe is one of the initial warning signs of choking in children. Other signs that may be observed include spastic clutching of the throat, ineffective or weak coughing, and cyanosis, which is blue tincture around the lips, face, and/or nails. Furthermore, in some moments, the child may appear to be scared, having bulging eyes, and in extreme cases, when the throat is completely blocking the airflow, the child may become unconscious. These symptoms above should be bypassed, and other measures should be taken as soon as possible.
Recognizing Blockage in a Child's Airway
When there is a situation involving the occlusion of the airway, as in this case, more ethical measures need to be taken; for instance, it is scary and alarming if I start noticing a child coughing aggressively or not talking much. I would put a gentle hand across my throat and wheeze as a means of crying, signaling to a person around me to see that I need help in getting to the hospital. Thereafter, depending upon the age of the child, I would provide help through either abdominal thrusts (for older children) or ‘chest thrusts and back blows” (for older ones). If a child becomes unresponsive, I would begin CPR immediately, one of which is artificial respiration until the help arrives.
Understanding the Signs of Choking
Choking occurs when an object wholly or partially obstructs the airway, leading to difficulty or inability to breathe. The key signs of choking include:
- Partial Airway Blockage:
- The person may cough forcefully, gag, or make high-pitched wheezing sounds, indicating some airflow is still present.
- Individuals can speak or make sounds, but breathing may be labored.
- Complete Airway Blockage:
- Lack of sound (no speaking, crying, or coughing).
- Hands often clutch at the throat (universal choking sign).
- Breathing difficulty, cyanosis (bluish skin), or loss of consciousness due to oxygen deprivation.
Technical Response Parameters:
Infants (Under 1 Year):- Begin with five back blows, applying the heel of the hand between the infant’s shoulder blades.
- Follow with five chest thrusts, pressing with two fingers on the lower half of the breastbone at a depth of about 1.5 inches (4 cm).
- Avoid abdominal thrusts to prevent injury.
- Deliver five back blows, using the heel of the hand firmly between the shoulder blades.
- Locate the navel and place a fist just above it.
- Apply quick, inward, and upward thrusts to dislodge the object.
- Repeat alternating back blows and abdominal thrusts until the object is expelled or the individual becomes unresponsive.
- Provide chest compressions at a depth of 2 inches (5 cm) for children and adults, maintaining a rate of 100–120 compressions per minute.
- Check the airway for visible obstructions between compression cycles and attempt rescue breaths if the airway is clear.
How to See the Object in a Child's Throat
To check what an object is in the child’s upper airway, I start by ensuring the child is placed such that there is enough light in the room or where he is standing to see the object. The next step involves looking into the mouth of the child, which can be done by gently leaning the child’s head back while moving their chin upwards. Steps must be taken with care so that the obstruction is not aggravated. Also, thanks to a flashlight, I could look into the child’s mouth to see if anything was lodged in the throat. If such a thing is seen, instead of trying to unblock the airway by sweeping with my fingers, I want to ensure I can quickly see the object, allowing me to retrieve it without losing the blockage position.
How to Prevent Choking in Children?

Efforts to prevent children's choking have to be accompanied by dedication and dedication, as children are not capable of being careful. Even during meals, ensure the children do not rush and that they are being supervised so that everyone can eat at his own pace. Young children should not be exposed to cut-up raw vegetables, whole grapes, hard candy, and nuts, which are dangerous. Young children are best suited to eating smaller-cut food since they’re still toddlers. Try to prevent children from swallowing little objects they should not be putting in their mouths, such as toys, coins, or buttons. Additionally, instruct the children to talk less, laugh less, and avoid any action of playing while placing food kindly in their mouths. Also, provide children with age-suited toys and limit the type of play they’re exposed to.
Tips for Avoiding Small Objects Around Children
To minimize the risk of choking due to small objects, implement the following strategies:
- Conduct Regular Inspections: Routinely check floors, play areas, and low surfaces for any loose small objects, such as coins, buttons, beads, or deflated balloons, and remove them immediately.
- Age-Appropriate Toys: Ensure all toys comply with ASTM F963-17 safety standards, especially for children under three. Avoid toys with detachable small parts, and use a small parts tester (1.25 inches/31.7 mm in diameter) to assess choking risks.
- Secure Household Items: Store items like batteries, jewelry, safety pins, and small hardware components in locked cabinets or out of reach.
- Monitor Playtime: Supervise children closely while playing to prevent them from placing objects in their mouths.
- Educate Caregivers: Inform all caregivers, including babysitters and relatives, about the potential hazards posed by small objects and the importance of vigilance.
- Use Child-Safe Storage: For small items that are frequently used by adults but dangerous for children, opt for storage solutions with locking mechanisms.
- Encourage Cleaning Habits: Teach older children to tidy up toys after play to ensure younger siblings do not access hazardous items.
These detailed measures allow for effective risk mitigation while creating a safer environment for children.
What Foods Pose a Choking Hazard?
Certain foods can be quite a choking hazard, especially for the little ones, due to their size shape, or even texture. I would particularly imagine foods like whole grapes, hot dogs, nuts, popcorn, hard candy, or even chunks of raw vegetables or meat as dangerous. Because they are somewhat round, sticky, complex, or not easy to chew, those items can quickly stop airways and be the cause of young children choking. According to a food separation guide, foods with parts measuring 1.5 centimeters in diameter or more. For children, items that crib the size of their air passages are very hazardous. Other elements like the texture of peanut butter or chewing gum that can stick to the throat also have great potential and further increase the risks. However, other risks can be eliminated or minimized by making smaller pieces of the food that could be risky or by avoiding serving them in the first place.
Supervision and First Aid Advice for Parents
Monitoring and providing first aid are imperative parental responsibilities in safeguarding children. Through instructional videos, I have learned the importance of constant surveillance, especially during risky undertakings such as swimming or using the playground to help reduce the chances of an accident. During an injury, I put more effort into maintaining a first aid kit with more supplies and learning how procedures are done in case of minor cuts, burns, choking, or even performing CPR. Moreover, I always place my phone in quiet mode to ensure that essential phone numbers, for instance, the fire brigade, police, or doctor, are stored in it. I stab the last point in stating that there are adequate resources and necessary retraining of information through proven courses. Proactive measures and preparedness are required to deal with unexpected events more efficiently.
References
Choking Child ThoraxFrequently Asked Questions (FAQ)
Q: What should I do first if my 3-year-old is choking?
A: If your 3-year-old is choking, staying calm and acting quickly is important. Start by encouraging them to cough forcefully to see if the object comes out independently. If they cannot cough or breathe, you must proceed with first aid for choking.Q: How do I perform choking first aid for a child older than 1 year?
A: For a child older than 1 year, use a combination of back blows and abdominal thrusts. Stand behind the child and make a fist with one hand. Place the thumb side of your fist against the middle of the child’s abdomen, just above the navel. Grasp your fist with your other hand and perform quick, inward and upward thrusts.Q: Can I perform back blows on a 3-year-old?
A: Yes, you can perform sharp back blows on a 3-year-old. Stand to the side or slightly behind the child, supporting their chest with one hand. Lean them forward and use the heel of your other hand to deliver up to five forceful blows between their shoulder blades.Q: What should I do if the child is still choking after back blows and abdominal thrusts?
A: If the child is still choking after performing back blows and abdominal thrusts, call 999 or local emergency services immediately and continue with first aid until help arrives or the object is dislodged.Q: How can I check if the object comes out?
A: After performing back blows or abdominal thrusts, check to see if the object comes out or if the child can breathe, cough, or speak. Suppose they cannot, continue the first aid measures.Q: Should I put my fingers in the child’s mouth to remove the object?
A: Do not put your fingers in the child’s mouth to remove the object unless you can see it clearly and easily reach it. Blindly sweeping your fingers may push the object deeper into the airway.Q: When should I get medical help after a choking incident?
A: Always seek medical help after a choking incident, even if the object emerges and the child seems fine. It’s essential to ensure that there are no complications or injuries.Q: How can I prevent my child from choking in the future?
A: To prevent choking, supervise your child during meals, cut food into small, manageable pieces, and keep small objects out of reach. Educate them about the dangers of putting objects in their mouth.Q: What resources are available to learn more about first aid for choking?
A: Organizations like the American Heart Association offer step-by-step guides and courses on first aid for choking. These resources can provide valuable information and training for handling such emergencies.














 Login with Google
Login with Google Login with Facebook
Login with Facebook