
Choking is a dangerous situation and is life-threatening, which needs immediate action. For parents, child caregivers, and educators, learning how to take this step can be the difference between saving a life and causing a forever impact on the child and the family. In the abovementioned situation, the writer has focused on providing a proper skeleton structure for the reader to assist with choking, particularly suitable for 4-year-old kids. Readers will be given precise information on identifying the symptoms of choking, the fundamental difference between partial and complete airway obstructions, and how to deal with them . This article also explains the everyday items that might result in a child experiencing choking and how to prevent them from reducing cases. At the end of this article, the reader will be able to enhance their confidence and knowledge on how to save a life in circumstances when only a few seconds are available.
What are the signs of choking in a 4-year-old?
Any obstruction in a 4-year-old’s airway can be a serious cause of concern, especially if a child suddenly struggles with breathing, coughing, or gagging. In case of a weak airway blockage, a child may begin to make a rattling sound while breathing or coughing and may also wheeze. Still, if the blockage is complete, then the child, in some cases, would not be able to call out or scream, would struggle to breathe, and, in extreme situations, would start to turn a bit blue around their mouth and skin. Other indications include grabbing their throat and a look of panic on their face, and if the obstruction is not treated, then it can lead to the individual passing out.
Recognizing the Symptoms of Choking
When dealing with cases of choking in children, the first four things I will focus on as the child is perpendicular to me, the child being able to cough or make sounds would indicate a situation of partial airway obstruction; however, if a child is neither able to talk nor cry and can sustain breath, this means there is a situation of complete obstruction of the airway. Other critical indicators would be whether the child is holding their neck, how stressed out they are, and how pale their face looks. There are also silent indicators such as when the child tries to inhale or has a change in awareness, these signs indicate that which requires relief boundaries.
Differences Between Partial and Complete Airway Obstruction
A partial airway blockage happens when a portion of the airway is not fully closed off and still lets some air in. A cough, wheezing, or other sounds commonly heard during inhalation and exhalation may be present. Airway obstruction may be associated with strong attempts to remove the blockage, and the affected person is generally able to express the problem. It means that some ventilation can take place, but it might be through the use of abnormal or difficult breathing patterns.
In complete airway obstruction, the air breathed in cannot reach the lungs because of a blockage. There is a loss of the ability to speak, breathe, make sounds, or anything in this type of airway blockage. The person may show signs of choking, panic, worry, or develop a bluish tint to the skin or lips. If a person is not helped quickly through back blows or abdominal thrusts, or any other emergency case, he or she stands at a risk of losing consciousness and threats to life.
Technical Parameters:
- Partial Obstruction:
- Airflow: Reduced but present.
- Cough Reflex: Strong and typically productive.
- Oxygen Saturation (SpO2): It may slightly decrease but can remain above critical thresholds (the normal range is generally 95%-100%).
- Complete Obstruction:
- Airflow: Absent.
- Auditory Indicators: No coughing, wheezing, or sounds from the victim.
- Oxygen Saturation (SpO2): Rapidly drops below critical levels, potentially leading to hypoxia (<90% SpO2).
Prompt recognition of the differences and taking appropriate action is essential to prevent severe outcomes and restore the airway to functionality.
When to Intervene Immediately
I will jump into action right away when I notice signs of a total airway blockage, in this case the person is not able to cough, speak, or breathe effectively, and airflow or any sounds are absent. Any single person that seems to be in distress and holds his/her throat (the universal sign of choking) or starts losing the consciousness then I know what I need to do; and it has to be fast! Delivering back blows, performing the Heimlich cut, or even starting CPR in the case that the injured person is unconscious is of utmost importance until the qualified medical team arrives. Act fast and prevent further damage before it is too late and the person’s life is at risk due to lack of oxygen.
How to help a choking 4-year-old?
To assist a choking 4-year-old, follow these steps:
- Assess the Situation:
- If the child is coughing forcefully, encourage them to keep coughing, as this is often the most effective way to clear the airway.
- If the child cannot cough, speak, cry, or breathe, immediate action is required.
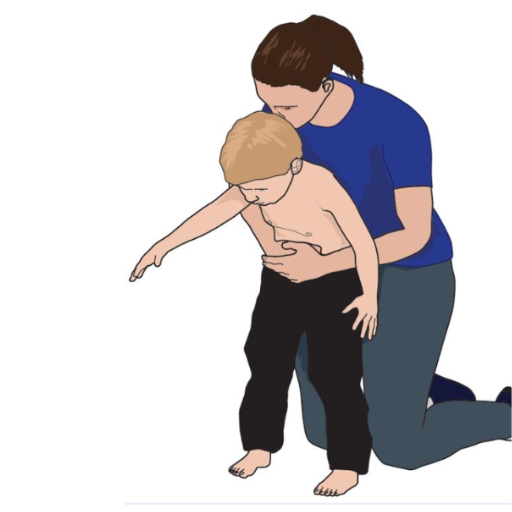
- Perform Back Blows:
- Position the child by bending them forward at the waist.
- Deliver up to 5 firm back blows between the shoulder blades using the heel of your hand.
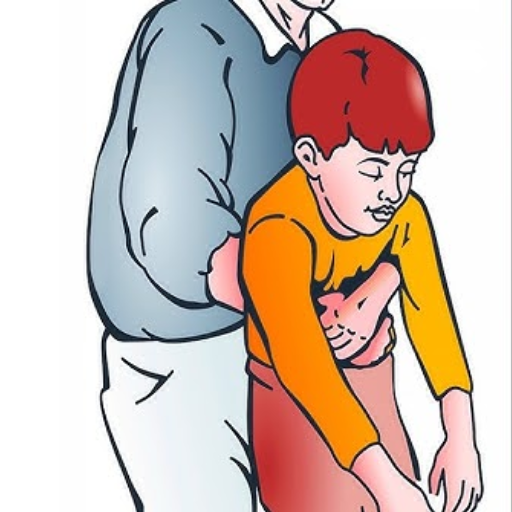
- Perform Abdominal Thrusts (Heimlich Maneuver):
- Stand behind the child, wrapping your arms around their waist.
- Make a fist and place it just above the child's navel, below the ribcage.
- Grasp your fist with your other hand and perform up to 5 quick, inward, and upward thrusts.
- Repeat if Necessary:
- Alternate between 5 back blows and five abdominal thrusts until the object is expelled or the child becomes unconscious.
- If the Child Becomes Unconscious:
- Carefully lay the child on a flat surface.
- Call emergency services immediately and begin CPR, checking the airway for visible obstructions after every 30 compressions.
Prompt action following these steps can help dislodge the obstruction and restore breathing until professional medical assistance is available. Always seek medical evaluation afterward to ensure no further complications.
Step-by-step Guide for Back Blows and Abdominal Thrusts
- Assess the Situation:
- Check if the child is choking and unable to cough, speak, or breathe. Choking victims often clutch their throats, which is a universal distress signal.
- Perform Back Blows:
- Position the child to lean forward slightly. For more minor children, support their chest with one hand.
- Use the heel of your hand to deliver five firm back blows directly between the child's shoulder blades. Each blow should be forceful enough to dislodge the obstruction.
- Perform Abdominal Thrusts:
- Stand behind the child and wrap your arms around their waist.
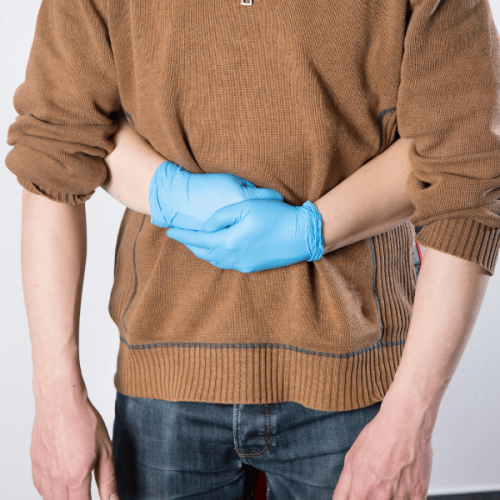
- Make a fist with one hand and position it just above the navel, below the ribcage.
- Grasp your fist with the other hand and perform up to 5 quick, inward, and upward thrusts to apply pressure to the diaphragm and force the object out.
- Repeat the Steps if Necessary:
- Alternate between 5 back blows and five abdominal thrusts until the obstruction is expelled or the child becomes unconscious. Be cautious not to apply excessive force that could cause injury.
- Monitor and Act if Unconsciousness Occurs:
- If the child becomes unresponsive, place them on a flat surface, activate emergency services, and begin CPR immediately.
- Check the airway after every 30 chest compressions, removing visible obstructions if found.
Technical Parameters to Ensure Effectiveness:
- Force of Blows: Back blows must be firm but controlled to avoid injuring the child. Force should focus between the scapulae.
- Hand Positioning for Thrusts: The fist must be placed above the navel but below the xiphoid process to avoid rib or internal organ damage.
- Thrust Angle: Abdominal thrusts should be directed inward and upward to maximize diaphragm pressure effectively.
- Response Time: Immediate execution of these steps is crucial to prevent hypoxia within the first few minutes.
Following these steps with precision can significantly improve the chances of clearing the airway and preventing further complications.
Adapting Techniques for a Child's Size and Age
When dealing with airway obstruction in children, the approach must be tailored to their size and developmental stage to ensure safety and efficacy. Here are the key adaptations:
- Infants (under 1 year):
- Back Blows:
-
- Place the infant's face on your forearm, supporting their head and neck.
- Apply five sharp back blows between the shoulder blades using the heel of your hand.
- Technical Parameters:
- Use minimal force appropriate for the infant’s size to prevent injury to fragile bones or soft tissues.
- Chest Thrusts:
- Turn the infant face up, keeping their head lower than the torso.
- Place two fingers just below the nipple line on the sternum and deliver five quick, firm chest thrusts.
- Technical Parameters:
- Thrusts should compress the chest by approximately 1.5 inches (or one-third of the chest depth).
- Children (1 year and older):
- Back Blows:
- Position the child leaning forward, supporting their chest with one hand.
- Deliver five strong back blows between the scapulae.
- Technical Parameters:
- Use enough force to dislodge the object but avoid overexertion that could cause spinal or internal injury.
- Abdominal Thrusts:
- Stand or kneel behind the child and wrap your arms around their waist.
- Make a fist and place it above the navel and below the ribcage, then perform five upward and inward thrusts.
- Technical Parameters:
- Generate sufficient pressure without exceeding the force needed based on the child’s size. Avoid thrust angles that could cause undue strain or harm.
- Older or Larger Children:
- Techniques mirror those for adults but should still be adjusted for the child’s weight and stature.
- Take care to gauge force delivery and thrust depth to avoid complications such as fractures or organ damage.
Adapting these techniques with precision ensures effective intervention while minimizing risks of injury related to a child's physical characteristics.
What should I do if the choking child becomes unresponsive?
If a child chokes and becomes unresponsive, the first thing you need to do is look for emergency services or have someone else look for lifeguards while you begin CPR. Get the child on a firm surface and start performing chest compression while centering both your palms on his chest. After every 30 chest… compressions, check if there is anything in the mouth, and if there is, remove it. Give them two rescue breaths after opening the air passage by slightly tilting the head. There is an unbroken cycle of this until the emergency help comes or the child’s brain waves become recognizable.
Transitioning from Choking First Aid to CPR
Assuming the child has already become unresponsive, I would leave the child on a flat surface while starting chest compressions and putting a call through to 911 or asking someone around to do so. With hands placed at the center of the child’s chest, I would then carry out 30 compressions consistent in depth and rhythm off my chest. Teen eureka com CPR and snot revolting feeling mechanics-wise, we were six moments of understanding while holding off deep breaths. Next, I would try to perform two rescue breaths, which were supposed to be gentle for this child. I will keep repeating this till the child can breathe or the medics arrive.
Importance of Calling Emergency Services
In case of a serious life attacker, you should first call emergency services, which can assist in preliminary care while waiting for the emergency responders to arrive. Emergency medical services are equipped with trained professionals and have the equipment and medications that are required to effectively manage and counteract advanced and life-threatening injuries such as cardiac arrest, choking, and severe traumas. Also, by immediately calling 911 or the local emergency number, the caller can get directions on providing first aid, such as CPR, before the paramedics arrive. The American Heart Association claims that the chances of survival for the subjects who have suffered from a cardiac attack increase significantly when the EMS is contacted at an early stage because when defibrillation and advanced care are not provided to the subject within a minute, the chances of survival decrease by 7 to 10 percent.
Le informazioni da comunicare quando si chiama il numero di emergenza sono in primo luogo: il luogo in cui si trova l’emergenza, la tipologia dell’emergenza e il stato della vittima. Sii paziente with the dispatcher and wait to answer more questions or hear the instructions. Information like the approximate age of the person in distress, their medical history, and whether or not they are awake can assist the help providers in taking further measures. The sooner and easier the help number is called, the better the results for the suffering person.
Continuing first aid efforts until help arrives
In any situation where a potential loss of life is involved, the prime concern should be to provide aid to the victim and prevent further damage to his health. Suppose the average person has to practice CPR. In that case, it is recommended to do compression at 100 and 120 times a minute for the average adult with a chest depression of between two to two point four inches while ensuring that after every depression, the threat is allowed to recover the chest, making the procedure comprehensive. While applying these Continue Compressions, the first recommendation should be chest compression at one hundred to one hundred twenty in a minute as this also ensures deeper thrusting. The recommendation by AHA for the technique is to start compressions and deep thrusts and swap sides as fatigue sets in so that the maximum number of compressions is done. Suicides can switch while other breaks regain some of their energy to provide more effective compressions. Alternatively, a clean bandage can be applied to the target while light pressures can be exerted to restrain bleeding from control. If one possesses the afflicted limb, lifting the injured limb can serve better in subduing the blood flow. The target potential is that the airway remains clear by checking the target's breath and responsiveness in close intervals. This should Dear Before, Lewer the victim's condition which indeed is enough to provide him with the chance of recovering.
Are there any special considerations for helping a choking 4-year-old?
Specific adjustments should be made in treating a choking 4-year-old due to their smaller anatomical structures and proclivity to injury. Begin by confirming choking by checking for lack of ability to speak, cry or make a high-pitched wheezing noise. If the toddler is alert, follow a routine of first five back blows, then five abdominal thrusts, also known as the Heimlich maneuver. It should be ensured that the back blows are applied with the heel of the hand between the child’s shoulder blades and that abdominal thrusts are performed just above the navel in a quick, inward, and upward motion. In case the choking child loses consciousness, lower the child to a flat surface and start doing CPR while checking the area for any physical obstruction between rescue breaths. Also, do not do blind sweeps of the mouth, as it may further push the object deeper into the airway. Push your action according to the child's size and how responsive she is until the emergency medical help arrives.
Adjusting Force and Technique for a Child's Body
When trying to help a child who is choking, the anatomical structures must be considered to ensure the appropriate amount of strength and the technique is suitable for the child’s needs. Back blows do, instead, tend to suffer when the force put into them is not measured appropriately because if it is not dislocated,d the child may end up getting injured due to the size of the child’s frame. Being in the proper sense is also very important, with the child needing to lean forward from the waist to get to the clearing of the airway faster.
Abdominal thrusts are performed by making a fist using one hand, placing it between the other hand, and pushing it in a direction toward the child’s softer abdomen. As the abdominal muscles are smoother, there is a lower chance that the child will feel excessive pressure. Also, when addressing children under the age of 4 years, be advised not directly to apply pressure on the child’s ribs and breastbone as it could quickly end up resulting in them getting fractured.
When the child requires CPR, they will need to have chest compressions performed on them, starting with 5 cm ones, which will eventually need to be around 2 inches deep. The motion of compress and release compress repeat at a standard average of 100 to 120 times every minute. Every rise of the chest when doing CPR indicates a successful attempt to make sure the child is not over-inhaling too much air.
Observing these technical parameters reduces the possibility of causing further injury while enhancing the effectiveness of the intervention. Medical assistance should always be sought professionally anytime these measures are undertaken and even after they are undertaken.
Communicating effectively with a frightened child
In conversations with kids who are afraid, particularly younger ones, I try to keep an even tone to calm them down. To achieve this, I squat next to the child so that we are on the same eye level; this way the child can also see that I am not a threat. When explaining the issue to them, I use age-appropriate or simple expressions to get my point across quickly while avoiding factors that instill fear in the child. I aim to remain friendly and open while asking children to talk about their feelings so that their feelings are acknowledged. Lastly, I assure them they are safe and I am there to assist.
Dealing with everyday challenges in child first aid situations
While attending to commonplace matters during a first aid for a child, I do focus on remaining calm and trying to gather my thoughts such that I do not add on to the stress level of the epileptic kid or myself. When it comes down to cuts and scrapes, I start by applying basic cleanser and soap while maintaining a dry sterile dressing over the wound to stop bleeding. During choking, I follow Amrc guidelines, which require me to give five back blows and then five abdominal thrusts, but not too much force. According to NHS guidelines, I should avoid ointments or ice and submerge the area in lukewarm running water for less than half an hour if it's a burn. Using clean instruments, averting non-gentle actions, and observing sanitation by washing hands means the chances of soreness or ill health balance out.
How can I prevent choking incidents in young children?
Mealtime in young children should be supervised strictly so that no external distractions are present and all meals are eaten with patience. Food should be cut so that large pieces such as whole grapefruits, demanding candy, or even nuts are eliminated because those are the key reasons children choke. Toys to be used also must uphold proper criteria and not small parts that can be accidentally eaten and cause choking. Moreover, children need to be taught to sit up straight because that can avoid walloping or even taking and putting food in their mouths whilst talking. Most of the time, children’s movements need to be observed regularly to avoid unwanted situations. Finally, children need to be taught and educated to be careful so that choking situations can be avoided almost entirely.
Identifying Common Choking Hazards for 4-Year-Olds
Choking hazards for 4-year-olds often arise from small, complex, or improperly sized items that can easily obstruct the airway. Common food-related hazards include whole grapes, hot dogs, chunks of meat or cheese, hard candies, popcorn, nuts, and large pieces of raw fruits or vegetables. Risks for non-food items include small toy parts, deflated balloons, marbles, coins, and beads.
Recommended Safety Parameters:
- Food Size and Consistency:
- Cut food into small pieces, ideally no more significant than ½ inch (1.3 cm) in diameter.
- Avoid very hard, sticky foods or foods that are prone to forming large chunks during chewing.
- Toy Safety:
- Toys should comply with ASTM F963 standards for toy safety in the US.
- Avoid toys with detachable or small parts smaller than 1.25 inches (3.2 cm) in diameter or 2.25 inches (5.7 cm) in length.
- Supervision and Posture:
- Always supervise mealtimes and playtime, ensuring the child remains seated upright while eating.
- Teach children not to run, jump, or engage in vigorous activity while eating or handling small objects.
Implementing these measures significantly reduces the risk of choking incidents and ensures a safer environment for young children.
Teaching children about safe eating habits
As we foster our children's growth, there is one important aspect we shouldn't ignore—safe eating practices. As a precautionary measure, start by ensuring that your child knows how important it is to scrub their hands with soap for at least twenty seconds before lunch. This can be crucial in stopping the spread of fatal bacteria like Salmonella and E. coli that can stay dormant on hands or surfaces.
Children must also be taught the correct way to handle food, including not cross-contaminating raw and cooked meals. For example, raw meat cannot be placed in the same area as a safe-to-eat dish and must instead be stored in a cold place at a temperature below four degrees Celsius. In addition, we recommend using separate boards and utensils for when raw and baked foods are being prepared.
Children should also appreciate ensuring that poultry is fried to exactly 165°F and ground meats such as beef and pork are set to 160°F. Similarly, seafood has a temperature threshold of 145°F. T Measuring these systems can be a breeze with a thermometer in the kitchen.
Parents ought to equip their children with the skills they need to avoid consuming expired or spoiled food. Those skills include reading expiration dates and knowing how to store certain types of food, such as swiftly putting meat and dairy products in the fridge.
Last but not least, young children should learn slowly and correctly to take in only small bits of food at once, as this will help them avoid choking. Do not give unsupervised children below four years old hard foodstuffs, fruits, or sweets such as whole grapes, nuts, or hard candy.
References
Choking Thorax ChildFrequently Asked Questions (FAQ)
Q: What are the signs and symptoms of a choking child?
A: The signs of a choking child include the inability to speak, cry, or cough effectively, struggling to breathe, making high-pitched noises while trying to breathe, bluish skin color, and panic or distress. If you notice these symptoms, acting quickly is crucial, as the child can't breathe and may lose consciousness.Q: What are the first aid steps for a child who is choking?
A: The first aid steps for a choking child are: 1) Encourage coughing if the child can breathe. 2) give five back blows between the shoulder blades if coughing doesn't work. 3) If back blows fail, perform five abdominal thrusts (Heimlich maneuver). 4) Alternate between back blows and abdominal thrusts until the object is dislodged or the child becomes unresponsive. 5) If the child becomes unresponsive, start CPR and call emergency services.Q: How do you perform back blows on a choking child?
A: Position yourself to the side and slightly behind the child to perform back blows. Support their chest with one hand and lean them forward. Using the heel of your other hand, give five forceful blows between the shoulder blades. The goal is to dislodge the object and clear the airway.Q: What is the correct technique for chest thrusts on a choking child?
A: For chest thrusts on a child, stand or kneel behind them and wrap your arms around their body. Place a fist with one hand on the middle of the breastbone. Grasp your fist with the other hand and pull sharply inwards and upwards. Give five chest thrusts, checking if the object has been dislodged after each thrust.Q: When should you call 911 or emergency services for a choking child?
A: Call 911 or your local emergency number immediately if the child cannot breathe, cough, or speak or if your attempts to dislodge the object are unsuccessful. Also, call if the child loses consciousness at any point. Calling for professional help sooner rather than later in a choking emergency is better.Q: Is first aid for choking different for a 1-year-old compared to a 4-year-old?
A: Yes, first aid for choking is slightly different for infants under 1 year old. For infants, you should give five back blows followed by five chest thrusts instead of abdominal thrusts. Support the infant face down on your forearm for back blows, and place them face up on your forearm for chest thrusts. For children over 1 year, including 4-year-olds, use the standard back blows and abdominal thrusts method.Q: Can any first aid apps help in a choking emergency?
A: Yes, several first aid apps are available that provide guidance for choking emergencies. The Red Cross First Aid app is popular, offering step-by-step instructions for various emergencies, including choking. These apps can be valuable resources, but you must familiarize yourself with the procedures before an emergency occurs and not rely solely on an app in a critical situation.Q: What should you do if you can't dislodge the object and the child becomes unresponsive?
A: If the child becomes unresponsive, lay them on a firm, flat surface and begin CPR immediately. Call 911 if you haven't already. Start with 30 chest compressions followed by two rescue breaths. Before giving rescue breaths, look in the mouth for the object. If you see it, remove it, but don't blindly sweep the mouth. Continue CPR until emergency services arrive or the child starts breathing normally.















 Login with Google
Login with Google Login with Facebook
Login with Facebook