
Choking is an event that leads to airway obstruction, which results in the body's oxygen supply being dangerously low, a condition called hypoxia. If there is too little oxygen in the body, the brain is particularly affected as the neural tissue suffers. Here, we discuss the relationship between choking incidents and possible reasons behind the resulting chronic brain injury. We intend to emphasize the results of a pilot study conducted to examine the cognitive and neurological functions of the hypoxic outcome of choking. In this study, we focus on the mechanics of oxygen supply deprivation, the vulnerability of the brain, and sensitivity to time, explaining the need for a precise understanding of the nature and the timing of intervention. These ideas help construct the severe long-term outcomes of such events and serve as an example for the research-critical discussion. Further, this discussion acts as a stepping stone for improving methods of medical response and precautionary measures directed to prevent hypoxic brain damage after choking.
What happens to the brain during a choking incident?

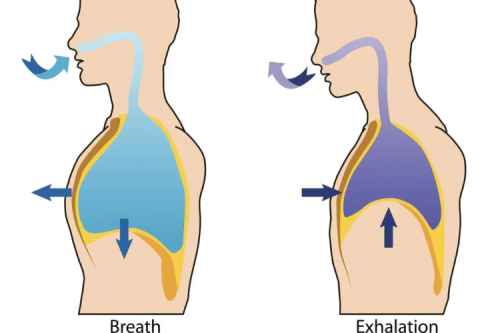
Obstructions to the airway during choking restrict the incoming airflow to the lungs and, subsequently, the bloodstream. This frequent occurrence of choking hamstrings the supply of oxygenated blood to the brain, which immediately leads to hypoxia and insufficient levels of oxygen in the brain. To bypass and remediate this life-threatening condition, practitioners can perform the Heimlich maneuver, which, along with back slaps, can efficiently free up the blocked airway, guaranteeing the brain's well-being. Triaging this situation within four to six minutes will prevent the brain from succumbing to irreversible damage by using a controlled shortage of oxygen to shut down the metabolism of the brain cells. Regarding different brain regions, the oxygen shortage threshold differs and usually spans from four to six minutes when the center of the brain starts giving up. Taking drastic measures such as CPR can switch the flow of oxygen into the body and guarantee that the person is not thrown into the clutches of dominating neurological damage.
How does choking affect the oxygen supply to the brain?
The moment an individual chokes, there is a blockage to the trachea, which does not allow the person to inhale freely. Without the ability to intake air, the person cannot bring oxygen deep enough into the lungs and, consequently, into the bloodstream. The longer this block remains, the more complex the situation will become. Within a short timeframe, the person will experience severe consequences where a single tissue oxygen remains, triggering the state of the brain cells that depend on the constant supply of energy and oxygen. Choking needs to be dealt with immediately to guarantee that proper blood flow, oxygen-rich, is delivered to the brain; otherwise, the brain will begin to enter zombie mode, where the only way to escape will be to destroy them. Of course, suppose the block to the trachea stems from a foreign object. In that case, dislodging that specific object will yield the opposite effect, blocking the supply of oxygen to the brain and partially eliminating the possibility of brain overheating.
What are the immediate effects of strangulation on brain function?
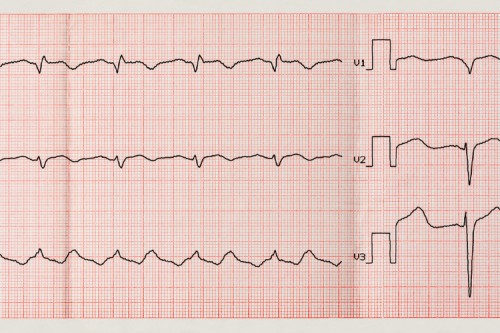
Every form of strangulation obliterates the flow of oxygenated blood to the brain, which causes hypoxia within a few seconds. The energy demands that the brain requires to function cannot be met as a result, and this deprivation results in an immediate blackout. Also, constriction on the carotid arteries leads to stimulated baroreceptors, which causes reflexive cardiac arrest or arrhythmias, making the lack of oxygen delivery much worse. Extended strangulation without any help can result in irreversible brain damage in four to five minutes as the oxygen-deprived neurons die at an accelerated rate.
Can a brief choking episode cause hypoxic-ischemic brain injury?
Yes, even a short episode of choking has the potential to induce hypoxic-ischemic brain injury (HIBI) if the oxygen (hypoxia) and blood flow (ischemia) to the brain is extensive, at least for a short while. The duration of oxygen for the brain to be suffocated (deprivation) is what is most concerning. Neurons are susceptible to lacking oxygen and commence suffering damage 3 - 4 minutes after being deprived. If the choking is prolonged beyond this period, the likelihood of hypoxic-ischemic brain injury becomes heightened.
Some of these key technical parameters are:
- Oxygen saturation levels (SpO2): Neuronal damage begins ShpO’s intervention. When SpO2 descends below 90% (hypoxemia), permanence exposes the individual to 3 to 5 minutes of sustained hypoxia.
- Cerebral perfusion pressure (CPP): Directly strangling blood flow leading to choking conditions critically decreases CPP. CPP values below 60 mmHg are critical and profoundly decrease oxygen delivered to the brain tissues.
- Duration of hypoxia/ischemia: Significant neuron hypoxic damage occurs after the 4 to 5-minute mark of complete oxygen deprivation. The irreversible injury occurs soon thereafter, and measures must be enacted rapidly.
- Partial oxygen pressure in arterial blood (PaO2): PaO2 below 60 mmHg typically leads to severe hypoxia.
Choking moments that last only a few seconds tend to be less damaging to the brain in the long term. They can cause hypoxia, which could lead to irreversible changes in brain function or other complications depending on the extent of the individual’s vulnerability. HIBI can be treated or prevented by restoring immediate medical assistance and oxygen.
How can choking lead to an acquired brain injury (ABI)?
Choking can lead to an ABI primarily due to strangulation or something compressing the airway, interfering with oxygen intake. As a result, cerebral hypoxia might occur in about two to three minutes. The brain is susceptible to oxygen deprivation, and even short periods of inadequate oxygen supply can cause neuronal death. Additionally, choking for a prolonged time can result in significant amounts of HIBI, which will impact cognition and motor and sensory activities, depending on where the brain sustains damage. Providing timely intervention to restore oxygenation is crucial in preventing ABI straining from choking.
What is the relationship between oxygen deprivation and brain cell damage?
The connection between brain cell injury and oxygen deficiency is highly concerning. Nerve tissues are at risk because they depend on a continuous oxygen supply and cannot store energy sufficiently. The starvation of oxygen will render the tissues incapable of supporting standard metabolic mechanisms within a very short time. This will finally lead to a state of disorder and, ultimately, death. Even short intervals of oxygen starvation can set off an energetic failure, toxic substance accumulation, inflammation, and other events. Long-lasting deprivation usually results in massive neuronal death, and the extent of this death determines the functions of the brain that will be affected. These observations are a clear indication that the affected tissues need timely oxygen supply for preventing further damage..
How long does it take for choking to cause an ABI?
Choking does have the potential to cause Acquired Brain Injuries (ABIs), but only in some cases. Essentially, it depends on the extent of airway obstruction and the health of the individual in question. ABIs are most prevalent when all sources of oxygen are sealed off, leading to potential anoxia. There are different severities to lung hyperperfusion, some being mild, like a lapse into confusion, or some more serious, like anoxic conditions, where all brain activity ceases. Alongside deep and permanent neurological damage, the injury depends on the preexisting conditions of the person, the severity of oxygen deprivation, and how swift the medical assistance is. Efficiency can be improved by clearer currents of assistive ventilation, CPR, and other means during oxygen deprivation. The objective is to combat the bane before it can deal irreversible damage.
Are there different types of brain injuries resulting from choking?
Choking can lead to serious consequences, and with the passage of 5-10 minutes, damages that can be caused are magnanimous, harming the cells on deeper levels. The 3-5 minute mark accounts for moderate attention damages in the form of foggy vision and shallow confusion, and long-term condition is guaranteed fatal. PME is the main reason neck constriction is so damaging, as the brain experiences excess lung hyperperfusion and low blood oxygen supply.
What are the signs and symptoms of brain damage from choking?
The symptoms and signs one suffers may vary when diagnosing brain damage due to suspected strangulation as it relates to the timeframe and severity of oxygen deprivation. Common indications include confusion, memory loss, or cognitive impairment, which may occur immediately after the incident. Other neurological symptoms, such as seizures or problems with balance, coordination, and other forms of movement, may also be present. Some patients also report chronic headaches, dizziness, or problems with vision. More advanced symptoms may include disturbances of consciousness, shortness of breath, and specific chronic neurological issues such as speech and movement disorders. To avoid as much damage as possible, seeking help in the early stages will be most beneficial.
How does loss of consciousness relate to the severity of brain injury?
Loss of consciousness (LOC) is a key indicator in assessing a brain injury's severity. Its duration is directly correlated with the level of injury severity, measured through specific thresholds. Brain injuries are classified as mild, moderate, or severe based on the following widely accepted parameters:
- Mild Traumatic Brain Injury (TBI): LOC lasts less than 30 minutes. These injuries may result in temporary confusion or memory loss but often have a favorable prognosis with appropriate care.
- Moderate TBI: LOC persists between 30 minutes and 24 hours. These cases often involve noticeable cognitive or physical impairments requiring medical intervention and rehabilitation.
- Severe TBI: LOC exceeds 24 hours. Severe injuries are typically associated with significant and long-term neurological deficits, warranting intensive medical treatment and ongoing support.
The Glasgow Coma Scale (GCS) is also commonly used alongside LOC duration to further evaluate and confirm injury severity. Lower GCS scores indicate more significant impairment. Accurate assessment of LOC and timely intervention are critical to improving outcomes for individuals with brain injuries.
What cognitive and psychological changes may occur after a choking-induced ABI?
Cognitive and emotional functions often alter or worsen after a choking-induced acquired brain injury (ABI). The level of change hinges on the extent and area of the brain’s physical damage caused by oxygen deprivation (hypoxia). Hard cognitive keywords that arise after such an event are lack of focus, deficits in memory—especially short-term memory—and executive dysfunction, which hampers challenges in problem-solving, decision-making, and planning. Other salient features patients suffer from include aphasia and slowed mental processing capabilities.
Due to the brain's failure to regulate emotions, irritation, mood changes, anxiety, depression, and even PTSD are profound psychological alterations. These changes rely on the extent of emotional responses, ranging from severe to mild. PTSD is more likely to be experienced if the incident of choking is deemed life-threatening. The relevant particularities suggest that hypoxic episodes occurring persistently over 4 to 5 minutes critically heighten the chances of grave brain injury. Neurological recuperation probabilities tend to drop substantially beyond this point, and the risks being taken grow rather severe. Timely neuropsychological assessment and rehabilitation approaches are of the essence in dealing with these complex problems and providing recovery assistance.
How is the Glasgow Coma Scale used to assess choking-related brain injuries?
The Glasgow Coma Scale (GCS) is a fundamental tool for estimating the gravity of injuries to the brain caused by choking episodes. It determines a patient's consciousness in three aspects: eye-opening, verbal response, and motor response. These three criteria are scored separately and summed to define the level of impairment, which may be classified as mild, moderate, or severe. A low GCS score after a choking incident suggests considerable brain hypoxia or damage exists, which aids in determining further treatment actions and prognostic steps. GCS measurement parameters should also be followed during recovery to ensure proper restoration of hypoxic damage.
What first aid measures can prevent brain damage during a choking incident?

First aid interventions are of utmost importance in averting a variety of brain damage caused by cases of choking. The initial intervention involves evaluating the victim’s choking sound for wheezing or ability to cough. If the victim’s voice is nonexistent, then emphysema is present and physically obstructing the and applying the Heimlich maneuver (forcing abdominal thrusts) to the person. For infants, perform five back slaps followed by five chest thrusts alternatively. If the person is responsive, do not attempt to talk to them and commence with CPR by giving artificial ventilation. Rescue breathing ought to be done to supply air. Timely accessibility of medical personnel for definitive treatment of the patient is vital. First Aid that is administered hypothesizes that the patient will experience minimum hypoxic damage to the brain, enabling the person to regain independent breathing without further assistance.
How effective is the Heimlich maneuver in preventing hypoxic brain injury?
The immobilization method of airway obstructions is the most used technique for preventing hypoxic brain injuries and is done with a lot of efficiency. It has been established that 86 percent to 97 percent of airborne material gets successfully removed depending on the obstruction's type and location. This method of dislodging obstruction works by suctioning through a stoma (neck opening) and applying a firm tracheostomy tube to rip off any remaining secretions. It works best when the obstacle is removed; otherwise, delays occur, lowering hetero blockage sufficiency. The practical aim and quick reaction remove oxygen deprivation from the brain, which is the most crucial requirement in averting obstructions to the airway. It is critical to its functioning without treatment, and four minutes of apnea may result in severe damage. A thorough understanding is required to master the Heimlich maneuver to enable quick relief during airway obstruction emergencies.
What steps should be taken to restore oxygen flow to the brain quickly?
When there is an airway obstruction, it is my utmost priority to restore oxygen flow to the brain as quickly as possible. First, I would analyze the situation to determine how serious it is. If someone is choking and gasping for air, I will execute the Heimlich maneuver immediately, using the appropriate technique to generate enough force to remove the obstruction. I would then perform CPR (cardiopulmonary resuscitation), chest compressions, and rescue breaths until medical personnel arrive while simultaneously making sure the emergency services are being contacted right away. I understand the importance of mitigating CPR focus to rescue breaths so the professional staff can take over and focus on oxygenation. It is vital to be familiar with life-saving skills to execute them appropriately.
How are choking-induced brain injuries diagnosed and treated?

Choking-related brain injuries are recognized with a mix of clinical assessment and imaging techniques. Doctors evaluate the patient’s history: how long did the patient choke, and what were the oxygen deficiency symptoms and neurological disturbances such as confusion, fainting, and weakness? MRI and CT scans are performed to assess the extent of damage to specific brain structures or to determine the presence of hypoxic injuries. The treatment strategy should focus on restoring regular oxygen supply and achieving the minimum possible long-term damage. In most cases, patients receive oxygen, diuretics, and, as a last resort, rehabilitation therapy to treat secondary or severe injuries. Everything possible must be done to prevent permanent injury from these conditions, so swift medical attention is necessary.
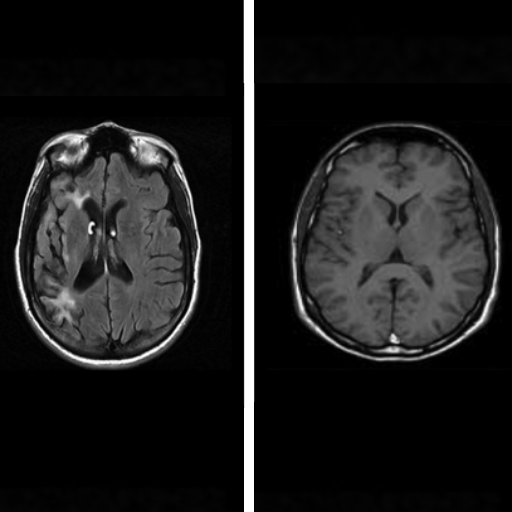
What role does MRI play in assessing brain damage from choking?
MRI is beneficial in evaluating the damage done to the brain by a choking episode. MRI identifies structures in the brain, differentiating between various forms of damage done due to hypoxia or ischemia (the two types of brain damage that occur during a choking episode). MRI offers much finer detail than other imaging options, like CT scans, and detects acceptable changes inside the brain tissue. One such specialized form of MRI scans is diffusion-weighted imaging or DWI. Diffusion-weighted imaging (DWI) is essential in assessing the scope and position of damage to the brain due to lack of oxygen since it is best suited to visualize acute ischemic injuries. These medications enable the practitioner to concentrate on the precise area of concern and achieve higher recovery rates.
What rehabilitation options are available for those with ABI after choking?
Rehabilitation protocols for patients with an acquired brain injury (ABI) from choking are typically directed toward improving physical, cognitive, and speech rehabilitation while enhancing life quality. These include physical training to improve motor and balance functions, occupational training to develop activities of daily living (ADLs), and speech and language therapy to improve communication and swallowing. Cognitive rehabilitation may also be needed for memory, attention, and problem-solving impairments. The particular technical details of rehabilitation usually differ with the degree and site of the brain injury. For instance, these therapies can comprise certain structured activities focusing on neuroplasticity to rehabilitate speech functions and targeted muscle strength training and sensory re-integration activities. Neurology, therapy, and rehabilitation medicine specialists must work together to create an individualized comprehensive recovery plan.
References
-
"The choking game”: self-induced hypoxia presenting as recurrent seizurelike events" - Discusses self-induced hypoxia and its neurological effects.
-
"Hypoxic-ischemic brain injury: pathophysiology, neuropathology and mechanisms" - Explores the mechanisms and outcomes of hypoxic-ischemic brain injuries.
-
"Neuropsychological and neuropathological effects of anoxic or ischemic induced brain injury" - Examines the neuropsychological impacts of anoxic or ischemic brain injuries.
Frequently Asked Questions (FAQ)
Q: Can choking cause an acquired brain injury?
A: Yes, choking can cause an acquired brain injury (ABI). When the airway is blocked, it restricts oxygen flow to the brain, potentially leading to hypoxic or ischemic brain injury. This type of injury can damage various areas of the brain, affecting cognitive function, memory, and other neurological processes.Q: What are the potential effects of brain injury from choking?
A: The effects of brain injury from choking can vary depending on the severity and duration of oxygen deprivation. Potential effects may include memory problems, impaired cognitive function, changes in behavior, difficulty with speech and language, motor skill impairment, and in severe cases, long-term disability or even death. The specific outcomes depend on which areas of the brain are affected and the extent of the damage.Q: How does choking lead to damage to the brain?
A: Choking can lead to damage to the brain by cutting off the oxygen supply. When the airway is blocked, blood flow carrying oxygen to the brain is reduced or completely stopped. This lack of oxygen, known as hypoxia or anoxia, can cause brain cells to die within minutes, resulting in a hypoxic or ischemic brain injury. The longer the brain is deprived of oxygen, the more severe the damage can be.Q: What are the long-term effects of ABI from choking?
A: The long-term effects of ABI from choking can be significant and may include persistent cognitive impairment, changes in personality, difficulty with executive functioning, ongoing memory problems, and physical disabilities. In some cases, individuals may require long-term care and support. The severity of these effects can range from mild to severe, depending on the extent of the brain injury and the effectiveness of treatment and rehabilitation.Q: How does treatment and rehabilitation for ABI from choking differ from TBI?
A: While treatment and rehabilitation for ABI from choking share some similarities with traumatic brain injury (TBI), there are key differences. ABI from choking is a non-traumatic injury, so the initial focus is on restoring oxygen supply and preventing further damage. Rehabilitation may emphasize cognitive and functional recovery more than physical trauma management. Both types of injuries may require long-term cognitive therapy, but ABI from choking might have a stronger focus on restoring functions affected by oxygen deprivation.Q: Can a preliminary study shed light on the hypoxic effects of choking?
A: Yes, a preliminary study can provide valuable insights into the hypoxic effects of choking. Such a study might use techniques like magnetic resonance imaging (MRI) to observe brain changes in individuals who have experienced choking incidents. It could help identify patterns of brain damage, assess the impact on cognitive and psychological functioning, and potentially inform treatment strategies. However, it's important to note that more comprehensive research would be needed to draw definitive conclusions.Q: How do instances of choking relate to intimate partner violence and brain injury?
A: Instances of choking in intimate partner violence can lead to acquired brain injury. When an abuser strangles or chokes their partner, it can cause hypoxic brain injury due to restricted blood flow and oxygen to the brain. This type of injury may not be immediately apparent but can have severe long-term consequences. The Brain Injury Association recognizes strangulation in domestic violence as a significant cause of ABI, highlighting the need for awareness and intervention in such cases.











 Login with Google
Login with Google Login with Facebook
Login with Facebook