Cardiac arrhythmias are a critical concern in emergency medicine, with ventricular tachycardia (VTach) and ventricular fibrillation (VFib) representing two of the most life-threatening conditions. While both originate in the ventricles and can lead to sudden cardiac arrest, their mechanisms, presentations, and treatments differ significantly. Understanding these differences is essential for healthcare providers to deliver prompt, effective interventions.
For the average person, VTach and VFib might seem like medical jargon, but distinguishing between them can mean the difference between life and death for clinicians. Let’s explore the pathophysiology, clinical presentation, and management strategies for these two dangerous arrhythmias.
What Is Ventricular Fibrillation (V-Fib)?
Ventricular fibrillation (V-Fib) is a severe and life-threatening heart rhythm disorder characterized by rapid and chaotic electrical signals in the lower chambers of the heart, known as the ventricles. This condition causes the ventricles to quiver or "fibrillate" instead of contracting effectively, severely disrupting blood flow to the body and vital organs.
Without immediate medical intervention, such as cardiopulmonary resuscitation (CPR) and defibrillation, V-Fib can lead to sudden cardiac arrest, which is often fatal. The condition is usually not preceded by warning signs, making it particularly dangerous. V-Fib is frequently associated with underlying heart diseases, such as coronary artery disease or heart failure, but it may also occur in individuals with no known cardiac issues.
Understanding the Heart’s Electrical System
Understanding the heart’s electrical system is essential to comprehending how V-Fib develops. The heart relies on a complex network of electrical impulses to coordinate its contractions and maintain a steady rhythm.
The Role of the Sinoatrial Node
The sinoatrial (SA) node, the heart’s natural pacemaker, is in the right atrium. It generates electrical signals that start each heartbeat. These signals prompt the atria (the upper chambers) to contract, pushing blood into the ventricles.
The Signal Pathway
The electrical impulse from the SA node travels through the atrioventricular (AV) node, which lies between the atria and ventricles. The AV node slows the signal slightly, ensuring the atria have enough time to empty blood into the ventricles before they contract. From the AV node, the signal travels along specialized fibers called the bundle of His and Purkinje fibers, causing the ventricles to contract in a coordinated manner. This process ensures effective blood pumping to the lungs and the rest of the body.
How Normal Rhythm Maintains Bodily Function
This carefully timed sequence of electrical signals and muscle contractions enables the heart to maintain its essential function of circulating oxygen-rich blood. When this electrical system operates normally, the heart beats steadily, typically 60 to 100 beats per minute in adults.
How V-Fib Disrupts Normal Heart Function
When V-Fib occurs, the orderly conduction of electrical impulses through the ventricles is replaced by erratic and disorganized signals. This disruption causes the ventricles to twitch or quiver rather than contract forcefully.
Loss of Effective Blood Circulation
Because the ventricles fail to contract coordinated, the heart cannot pump blood. This results in a sudden drop in blood pressure and cuts off blood flow to vital organs, including the brain and heart muscle. The lack of oxygenated blood can cause damage to these organs within minutes.
Risk of Sudden Cardiac Arrest
The most immediate danger of V-Fib is sudden cardiac arrest. This occurs when the heart stops pumping entirely. It’s an emergency condition that requires rapid intervention, typically with a defibrillator, to restore a normal heart rhythm. Without treatment, the chances of survival are extremely low.
Contributing Factors to V-Fib
V-Fib is often a complication of other cardiac conditions, such as a heart attack or ischemic heart disease. Scarring of the heart tissue from past heart attacks can also increase the risk. Other triggers include electrolyte imbalances, drug toxicity, or severe trauma to the chest. Despite these risk factors, primary V-Fib can also occur in individuals with no detectable heart disease, often due to inherited abnormalities in the heart's electrical pathways.
The Role of Defibrillation and Emergency Care
Defibrillation, which delivers an electrical shock to the heart, is the most effective way to stop V-Fib. The shock interrupts the chaotic electrical activity, allowing the heart to return to a normal rhythm. Without this treatment, the heart’s electrical chaos will persist, usually leading to death within minutes.
Ventricular fibrillation demands immediate medical attention due to its critical impact on the heart’s ability to sustain life. By understanding how the heart’s electrical system functions and how V-Fib disrupts it, we can better appreciate the importance of rapid intervention in this dangerous condition.
Symptoms of Ventricular Fibrillation: What to Watch For
Ventricular fibrillation (VF) is a life-threatening condition that requires immediate medical intervention. It disrupts the heart's normal rhythm, preventing blood from being pumped effectively to the rest of the body. Recognizing the symptoms of ventricular fibrillation can make the difference between life and death. Below, we’ll discuss the key signs to look out for in this critical cardiac emergency.
Sudden Collapse and Loss of Consciousness
One of the most striking and immediate symptoms of ventricular fibrillation is sudden collapse. This happens because VF disrupts the heart's ability to pump blood effectively, cutting off oxygen supply to the brain and other vital organs.
Loss of consciousness occurs almost instantaneously following the collapse. The body cannot maintain alertness or muscular coordination without sufficient blood flow to the brain. This is why someone experiencing VF often falls to the ground suddenly, even if they seemed wonderful moments before.
It’s vital to understand that this collapse is abrupt and unanticipated. Unlike fatigue or other gradual conditions, the onset of symptoms is rapid and severe. If someone you’re with collapses without warning, consider VF as a possible cause. Immediate action, such as calling emergency services and initiating CPR, could save their life.
Absence of Pulse and Breathing
During ventricular fibrillation, the heart's electrical signals become chaotic, causing it to quiver instead of beat. As a result, blood is no longer pumped effectively. This cessation of function leads to an absence of a detectable pulse.
To check for a pulse, feel for it at the neck or wrist. You won’t find one when VF is present because the heart is no longer circulating blood. Similarly, breathing stops or becomes irregular within seconds of the onset of VF due to the lack of oxygen throughout the body.
It’s important to distinguish this symptom from shallow or labored breathing caused by other conditions. With VF, there may be no respiratory activity because the heart’s failure to pump impacts oxygen delivery entirely. Recognizing the absence of pulse and effective breathing is a critical indicator that emergency measures are needed.
Unresponsiveness and Cyanosis
Unresponsiveness is another hallmark symptom of ventricular fibrillation. Because the brain is deprived of oxygen, a person in VF cannot respond to any stimulus, including verbal commands, touch, or pain. They may appear unconscious or in a coma-like state.
Another key visual sign to look out for is cyanosis, a bluish or grayish discoloration of the skin, lips, or fingernails. Cyanosis occurs because oxygen-poor blood cannot reach the tissues, resulting in the visible signs of oxygen deprivation. The progression of cyanosis can happen quickly, and its presence is a warning of critical danger.
Both unresponsiveness and cyanosis indicate the body is experiencing severe distress due to the lack of proper cardiac function. These signs require immediate action, such as calling emergency medical services and performing cardiopulmonary resuscitation (CPR) while waiting for professional help.
Recognizing these symptoms swiftly and responding urgently are essential during a ventricular fibrillation episode. Time is of the essence in such a crisis, and your actions could save a life. If you suspect ventricular fibrillation in someone, seek medical assistance immediately.
Common Causes of Ventricular Fibrillation
Ventricular fibrillation, often abbreviated as VF or V-fib, is a life-threatening condition in which the heart's ventricles quiver instead of pumping blood efficiently. This arrhythmia disrupts the heart's normal electrical impulses, halting its ability to circulate blood. Understanding the common causes of ventricular fibrillation is essential for prevention and management. Below, we break down the primary factors that often contribute to this condition.
Heart Disease and Previous Heart Attacks
Coronary Artery Disease (CAD) as a Key Trigger
Coronary artery disease is one of the most frequent underlying causes of ventricular fibrillation. CAD narrows or blocks the arteries that supply blood to the heart, which can lead to ischemia (reduced blood flow). The lack of nutrients and oxygen impairs heart tissue, creating electrical instability in the ventricles. This instability significantly increases the likelihood of abnormal heart rhythms like ventricular fibrillation.
Scarring from Previous Heart Attacks
A previous heart attack leaves scar tissue on the heart, which can interfere with the smooth conduction of electrical signals. Scarred heart tissue is less flexible and has difficulty responding to the impulses needed for a coordinated heartbeat. This disruption creates a fertile ground for VF to develop. It’s worth noting that VF is a common cause of death within the first hours after a myocardial infarction.
Cardiomyopathies and Other Structural Issues
Certain types of heart disease, such as dilated or hypertrophic cardiomyopathy, can also lead to VF. These conditions alter the structure or functionality of the heart muscle, reducing its ability to maintain a stable rhythm. Patients with these diseases are at an increased risk, as their hearts are more prone to erratic electrical activity.
Electrolyte Imbalances and Their Role
Electrolytes like potassium, sodium, calcium, and magnesium are crucial for the heart's electrical activity. These minerals help regulate how electrical impulses travel through the heart's cells. Imbalances in these electrolytes can lead to hazardous complications, including ventricular fibrillation.
Potassium Imbalances
Hypokalemia (low potassium) and hyperkalemia (high potassium) are two conditions that alter normal heart rhythm. Low potassium weakens the cells’ ability to conduct electrical impulses, increasing susceptibility to arrhythmias. High potassium, on the other hand, can prevent the heart from depolarizing properly, leading to potentially fatal rhythm disturbances.
Magnesium Deficiency
Magnesium works closely with potassium to support the heart’s electrical system. A magnesium deficiency can exacerbate the effect of low potassium and disrupt the electrical conduction within the heart, making ventricular fibrillation more likely.
Sodium and Calcium Fluctuations
Sodium and calcium play a role in the heart’s action potentials, the electrical impulses that cause the heart to beat. Imbalances in these minerals can disturb the precise sequence of depolarization and repolarization in the ventricles, making the heart vulnerable to erratic rhythms, including VF.
Intense Physical Activity and Stress Triggers
Extreme Exercise and Cardiac Strain
Engaging in intense physical activity can sometimes trigger ventricular fibrillation, particularly in people with underlying heart conditions. During heavy exercise, the demand for oxygen-rich blood spikes. If the cardiovascular system is unable to effectively meet this demand, the resulting stress can lead to ischemia and provoke VF. Competitive athletes with undiagnosed heart conditions are especially at risk.
Emotional Stress and Adrenaline Surges
Sudden emotional trauma or stress can also lead to a condition known as stress-induced cardiomyopathy, or “broken heart syndrome.” This temporary weakening of the heart muscle can mimic a heart attack and increase the risk of arrhythmias. The surge of stress hormones like adrenaline can trigger electrical instability in the ventricles, potentially leading to VF.
Preexisting Conditions Amplify Risk
For individuals with arrhythmia disorders or heart disease, physical and emotional stress can act as a catalyst for ventricular fibrillation. The combination of external triggers and internal vulnerabilities makes managing stress and sustained physical activity a key preventive measure for those at risk.
Ventricular fibrillation is a serious condition with several common causes, ranging from heart disease to electrolyte imbalances and physical or emotional stress. By understanding these triggers in detail, patients and healthcare providers can work together to implement preventative strategies and reduce the risk of this often-fatal arrhythmia. Early intervention, healthy lifestyle choices, and close medical supervision for at-risk individuals are essential in combating the dangers associated with ventricular fibrillation.
Diagnosing Ventricular Fibrillation: Tools and Techniques
Ventricular fibrillation (V-Fib) is a life-threatening cardiac arrhythmia that requires immediate attention. Effective diagnosis plays a critical role in timely treatment and improving patient outcomes. Here, we’ll look at the primary tools and techniques used to diagnose V-Fib, focusing on electrocardiograms, automated external defibrillators, and physical examination.
The Role of Electrocardiograms (ECG) in Diagnosis
Electrocardiograms (ECGs) are the gold standard for diagnosing ventricular fibrillation. This non-invasive tool records the heart's electrical activity, providing a visual representation clinicians can use to identify abnormalities.
The ECG shows distinct wave patterns in a normal heart rhythm, including P waves, QRS complexes, and T waves. However, in V-Fib, this organized pattern disappears. Instead, the ECG displays rapid, chaotic, and irregular electrical signals, reflecting the erratic contractions of the ventricles. These irregularities can help healthcare providers confirm the condition within moments.
One key advantage of using an ECG is its ability to distinguish V-Fib from other arrhythmias, such as ventricular tachycardia. This distinction is crucial, as treatment protocols differ based on the specific rhythm disturbance. Portable ECG monitors, often found in ambulances or emergency scenarios, allow for quick diagnosis on-site, further increasing the chances of survival during a cardiac emergency.
How AEDs Help Identify V-Fib
Automated external defibrillators (AEDs) are life-saving devices for public use during cardiac emergencies. They deliver shocks to restore a normal heart rhythm and play a vital role in diagnosing ventricular fibrillation.
When an AED is attached to a patient, its built-in algorithms analyze the heart's electrical activity to determine if a shockable rhythm, such as V-Fib, is present. If the device detects V-Fib, it audibly instructs the user to administer a shock, guiding even untrained bystanders through the process. By doing so, AEDs take on a dual role: identifying the condition and initiating treatment.
The portability and accessibility of AEDs make them indispensable in public spaces. They serve as a first line of defense in cardiac emergencies from airports to schools. Their ability to accurately recognize V-Fib in seconds ensures that treatment begins promptly, even outside of a hospital setting.
Physical Examination and Immediate Indicators
While advanced tools like ECGs and AEDs are critical in diagnosing V-Fib, physical examination remains essential, especially in scenarios where equipment may not be immediately available. Sure signs and symptoms can raise suspicion of ventricular fibrillation and prompt further diagnostic efforts.
Key signs of V-Fib include the sudden loss of consciousness, absence of a detectable pulse, and cessation of normal breathing. These symptoms indicate that the heart is no longer effectively pumping blood, leading to circulatory collapse. Other observations, such as cyanosis (a bluish tint to the skin, particularly around the lips or extremities), may also indicate severe oxygen deprivation caused by cardiac arrest.
Although these physical indicators are non-specific, their presence necessitates rapid action. First responders or bystanders trained in basic life support can initiate cardiopulmonary resuscitation (CPR) while awaiting advanced tools like AEDs or ECGs to confirm the diagnosis. This combination of immediate physical assessment and eventual use of diagnostic devices enhances the likelihood of survival.
By leveraging Electrocardiograms, AEDs, and physical examination techniques, clinicians and responders can effectively identify ventricular fibrillation and initiate lifesaving interventions without delay. Each tool uniquely plays a diagnostic role, reinforcing the need for prompt and coordinated action during cardiac emergencies.
Emergency Treatments for Ventricular Fibrillation
Ventricular fibrillation is a life-threatening cardiac emergency characterized by erratic electrical activity in the heart. This condition disrupts the heart’s ability to pump blood effectively, leading to a lack of oxygen delivery to vital organs. Immediate treatment is crucial to increase the chances of survival and prevent severe complications. Below, we outline the key emergency treatments for ventricular fibrillation, focusing on defibrillation, cardiopulmonary resuscitation (CPR), and medications to stabilize heart rhythm.
The Importance of Defibrillation
Defibrillation is the most critical intervention for ventricular fibrillation. It uses an electrical shock delivered via a defibrillator to reset the heart's electrical system and restore a normal rhythm. Without defibrillation, the chaotic electrical activity causing ventricular fibrillation cannot be corrected, usually resulting in cardiac arrest.
Timing is paramount during defibrillation. Studies show that survival rates significantly decrease with every passing minute without defibrillation. Automated External Defibrillators (AEDs) are widely available in public spaces and designed to be user-friendly. They allow bystanders to intervene before professional medical help arrives. When used promptly, these devices dramatically increase the likelihood of survival. AEDs analyze the heart rhythm to determine if a shock is necessary, ensuring proper treatment.
Performing CPR to Maintain Blood Flow
Cardiopulmonary resuscitation (CPR) is another essential step in managing ventricular fibrillation. While defibrillation addresses the root cause, CPR helps sustain life by pumping oxygenated blood to the brain, heart, and other vital organs until the heart’s rhythm is restored.
Proper CPR involves performing chest compressions at a depth of approximately 2 inches and a rate of 100 to 120 compressions per minute. High-quality compressions are vital to maintain adequate circulation. Incorporating two breaths after every 30 compressions is recommended if someone is trained in rescue breathing. However, hands-only CPR is effective when a bystander is untrained or unable to provide rescue breaths. CPR should be continuous and vigorous until a defibrillator is used or emergency medical services (EMS) arrive.
Medications for Stabilizing Heart Rhythm
Medications often play a crucial role alongside defibrillation and CPR to stabilize the heart rhythm following ventricular fibrillation. Healthcare professionals commonly administer antiarrhythmic drugs to help restore electrical stability in the heart.
1. Epinephrine: Administered as part of advanced cardiac life support (ACLS) protocols, epinephrine improves blood flow during resuscitation. It may enhance the efficacy of defibrillation by making the heart more responsive to electrical shocks.
2. Amiodarone or Lidocaine: These antiarrhythmic medications are frequently used after initial defibrillation attempts. They reduce the heart's irritability and prevent recurrent ventricular fibrillation episodes, improving the chances of successful resuscitation.
3. Magnesium Sulfate: This may be used if the ventricular fibrillation is linked to a specific condition, such as torsades de pointes, a polymorphic ventricular tachycardia. Magnesium helps address the underlying cause and stabilizes the rhythm.
All medications are administered under strict medical supervision and based on established protocols, ensuring the safest and most effective outcomes for individuals experiencing ventricular fibrillation.
By combining timely defibrillation, effective CPR, and appropriate medication, medical professionals and bystanders can significantly improve the chances of survival for someone experiencing ventricular fibrillation. Quick action and coordinated efforts are the foundation of successful treatment in these critical scenarios.
Long-Term Management and Prevention of V-Fib
Ventricular fibrillation (V-Fib) is a life-threatening condition that causes irregular and chaotic electrical activity in the heart. It disrupts normal blood flow and, if not treated immediately, can result in cardiac arrest. While emergency treatments like defibrillation are critical in saving lives, long-term management and prevention are just as important for individuals at risk. This involves lifestyle changes, medical devices, and regular monitoring to reduce recurrence and improve quality of life.
Lifestyle Changes to Reduce Risk
Heart-Healthy Diet
Adopting a heart-healthy diet is one of the most effective ways to lower the risk of V-Fib. A diet rich in fruits, vegetables, whole grains, and lean proteins helps maintain optimal heart function. Reducing sodium, sugar, and unhealthy fats can lower blood pressure, cholesterol, and the risk of heart disease, all contributing factors to arrhythmias like V-Fib.
Regular Exercise
Engaging in consistent, moderate physical activity strengthens the heart and improves circulation. Activities like walking, swimming, and cycling increase cardiovascular endurance, helping to regulate the heart’s rhythm. However, a healthcare provider should guide individuals recovering from a cardiac event or those with heart conditions to ensure exercise is safe and effective.
Quitting Smoking and Limiting Alcohol
Smoking significantly increases the risk of heart disease due to its effect on blood pressure and oxygen transport. Quitting smoking can dramatically improve heart health and reduce the likelihood of arrhythmias. Similarly, limiting alcohol consumption is crucial, as excessive drinking can lead to irregular heart rhythms and weaken the heart’s ability to function correctly.
Managing Stress
Chronic stress can trigger abnormal heart rhythms and worsen existing heart conditions. Stress management techniques such as deep breathing, meditation, or therapy can help control stress levels and support overall heart health.
The Role of Implantable Cardioverter-Defibrillators (ICDs)
An implantable cardioverter-defibrillator (ICD) is a small device that is critical in managing V-Fib for patients at high risk of recurrence. These devices are implanted under the skin and continuously monitor the heart’s rhythm.
How ICDs Work
When the device detects an abnormal rhythm indicative of fibrillation, it delivers an electrical shock to reset the heart’s rhythm. This immediate intervention can be life-saving in preventing sudden cardiac death and reducing the impact of repeated V-Fib episodes.
Who Benefits from ICDs?
ICDs are typically recommended for individuals with a history of V-Fib, sustained ventricular tachycardia, or weakened heart muscles caused by conditions like cardiomyopathy. They are also used in patients who are at high risk due to genetic disorders like long QT syndrome or Brugada syndrome.
Living with an ICD
Although an ICD is vital for high-risk patients, it does require some adjustments. Patients may need to avoid proximity to strong magnetic fields, inform airport security personnel, and limit certain high-impact activities. Regular check-ups are essential to ensure the device functions correctly and the leads remain securely in place.
Regular Check-Ups and Monitoring
Long-term management of V-Fib involves consistent follow-up care with healthcare professionals.
Tracking Progress
Regular appointments allow physicians to monitor heart health, evaluate treatment plans, and adjust medications as necessary. This ongoing care is critical to managing conditions that can cause V-Fib, such as coronary artery disease, heart failure, or electrolyte imbalances.
Diagnostic Tests
Follow-up visits often include diagnostic tests, such as electrocardiograms (EKGs), stress tests, or blood work, to detect any changes in heart function. Advanced imaging like echocardiograms or MRIs may also be performed to evaluate the heart’s structure and assess the severity of any underlying conditions.
Medication Review
Patients with a history of V-Fib may be prescribed medications like antiarrhythmics or beta-blockers to help control abnormal rhythms and prevent episodes. Regular reviews ensure that dosages remain appropriate and identify potential side effects or interactions.
Empowering Patients
Education plays a significant role during routine check-ups. Understanding the warning signs of arrhythmias, medication adherence, and lifestyle modifications can empower patients to take charge of their heart health. Collaborative care involving cardiologists, primary care physicians, and sometimes electrophysiologists ensures comprehensive management strategies are in place.
By adopting lifestyle modifications, utilizing medical advancements like ICDs, and maintaining regular medical follow-ups, individuals can significantly lower their risk of V-Fib and enhance their long-term wellbeing. These proactive measures help prevent life-threatening episodes and promote a better quality of life.
Ventricular Fibrillation vs. Ventricular Tachycardia: Key Differences
| Feature | Ventricular Tachycardia (VTach) | Ventricular Fibrillation (VFib) |
|---|---|---|
| Definition | Fast but organized rhythm originating in the ventricles. | Chaotic, disorganized electrical activity in the ventricles. |
| Heart Rhythm | Rapid and regular. | Erratic and irregular. |
| Pulse | Often present but may be weak or irregular. | No detectable pulse. |
| Symptoms | Palpitations, chest pain, dizziness, fainting. | Sudden collapse, no pulse, no breathing, unresponsiveness. |
| Risk Level | High; can progress to VFib if untreated. | Very high; immediate life-threatening emergency. |
| Treatment | Medications, cardioversion, or ICD for long-term control. | Immediate defibrillation and CPR. |
| Outcome Without Treatment | Can lead to VFib or cardiac arrest. | Rapid death due to lack of circulation. |
Comparing Symptoms and Risk Levels
Ventricular fibrillation (VF) and ventricular tachycardia (VT) are both severe heart rhythm disorders originating in the ventricles, but they differ significantly in their symptoms, risks, and potential outcomes.
Symptoms of Ventricular Fibrillation (VF)
Ventricular fibrillation is an erratic and disorganized electrical activity in the ventricles, leading to the heart's inability to pump blood effectively. Symptoms of VF often come on suddenly and can include:
- Loss of consciousness - This is usually the first noticeable sign since the heart stops pumping blood to the brain.
- No pulse - The chaotic rhythm makes it impossible to sustain a heartbeat.
- Sudden collapse - Cardiac arrest occurs immediately, making the situation life-threatening.
- Seizures - These may occur as the brain is deprived of oxygen.
VF is a medical emergency that leads to death if not treated immediately. It often occurs without warning, though it sometimes follows a history of heart disease.
Symptoms of Ventricular Tachycardia (VT)
Ventricular tachycardia is characterized by a fast but organized heart rhythm originating in the ventricles. Symptoms can range widely depending on the heart's ability to maintain pumping during these episodes. Common symptoms include:
- Palpitations - A noticeable and often uncomfortable awareness of a rapid heartbeat.
- Chest pain or discomfort - Caused by the heart working harder than usual.
- Shortness of breath - Due to reduced blood flow to the lungs.
- Dizziness or lightheadedness - Resulting from a lack of proper blood circulation.
- Fainting (syncope) can occur if the VT episode compromises blood flow to the brain.
A prolonged VT episode may escalate to VF or lead to cardiac arrest, especially if left untreated.
Risk Levels for VF and VT
-
Ventricular Fibrillation Risk Factors:
- VF is particularly life-threatening because it halts all blood circulation instantly. It’s often linked to prior heart attacks, cardiomyopathy, or significant electrolyte imbalances.
- Without immediate intervention, survival rates are extremely low.
-
Ventricular Tachycardia Risk Factors:
- While less immediately fatal than VF, VT still poses substantial risks, particularly if sustained. It increases the likelihood of progressing to VF.
- Risk factors include scarring from previous heart attacks, structural heart diseases, or genetic conditions like long QT syndrome.
Both conditions are critical, but VF generally represents a more imminent danger to life due to the complete cessation of effective cardiac activity.
Treatment Approaches for Each Condition
Treatment for Ventricular Fibrillation
Given the urgent nature of ventricular fibrillation, treatment focuses on restoring a normal heart rhythm as quickly as possible:
-
Immediate Defibrillation:
- This is the primary treatment for VF. An automated external defibrillator (AED) or manual defibrillator delivers an electric shock to the heart, halting the disorganized electrical activity and allowing the heart’s normal rhythm to resume.
-
Cardiopulmonary Resuscitation (CPR):
- Until defibrillation is available, high-quality CPR helps maintain some circulation and oxygen delivery to vital organs.
-
Medications:
- Drugs like amiodarone, lidocaine, or epinephrine may be administered after initial defibrillation attempts to stabilize the heart or improve resuscitation success.
-
Long-Term Management:
- Survivors of VF will often require an implantable cardioverter-defibrillator (ICD) to detect and correct future life-threatening arrhythmias.
- Addressing underlying causes, such as coronary artery disease or electrolyte imbalances, is crucial to prevent recurrence.
Treatment for Ventricular Tachycardia
Management of VT depends on whether it is sustained (lasting 30 seconds or more) or non-sustained, as well as the severity of symptoms:
-
Acute Management:
- Medications like amiodarone or procainamide are often used to stabilize the rhythm during an episode.
- Electrical Cardioversion is typically employed for unstable VT, where synchronized shocks can help normalize the heart rhythm.
-
Long-Term Management:
- Beta-blockers or Antiarrhythmic Drugs may be prescribed for patients prone to recurring VT episodes.
- An ICD is often recommended for patients at high risk of VT becoming life-threatening. The device can detect and treat dangerous rhythms by delivering shocks or pacing therapy.
-
Catheter Ablation:
- For patients with frequent VT that does not respond well to medication or ICD therapy, catheter ablation may be considered. This minimally invasive procedure disrupts the electrical pathways, causing the abnormal rhythm.
-
Treating Underlying Causes:
- Identifying and managing conditions like coronary artery blockages, myocardial scarring, or electrolyte disturbances are key to preventing VT recurrence.
While both conditions require advanced medical care, VF is an immediate life-or-death emergency, whereas VT often allows for more time to assess and implement treatment options. Regardless, timely intervention for both is critical to reducing mortality and improving outcomes.
Frequently Asked Questions
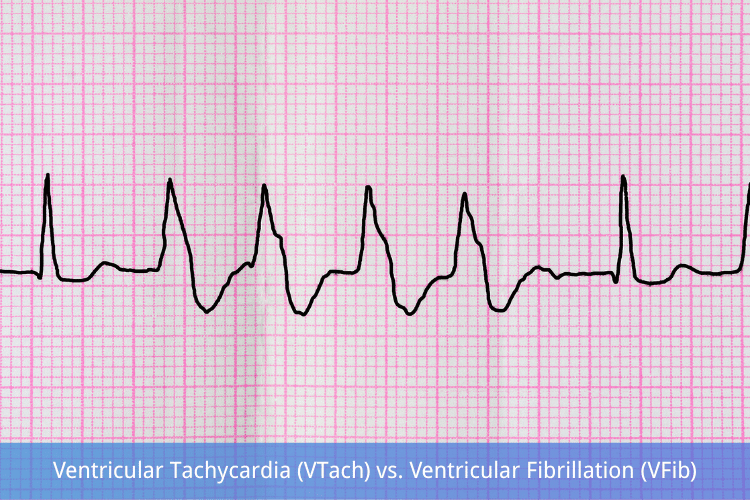
Q: What does VTach vs VFib look like on an ECG?
A: Vtach presents as a series of wide QRS complexes that may appear regular or irregular, indicating rapid ventricular contractions. In contrast, VFib shows a chaotic, irregular waveform with no identifiable QRS complexes, resembling a quivering of the ventricles, which is life-threatening and requires immediate intervention.
Q: What are the symptoms and causes of VTach and VFib?
A: Symptoms of VTach may include palpitations, dizziness, or fainting, while VFib often leads to sudden cardiac arrest, with symptoms including loss of consciousness and absence of a heartbeat. The causes of ventricular tachycardia can include ischemic heart disease and cardiomyopathy, whereas ventricular fibrillation is often caused by myocardial infarction or severe underlying heart abnormalities.
Q: How does heart rate differ in VTach and VFib?
A: In VTach, the heart rate is typically greater than 100 beats per minute, while in VFib, it is chaotic and cannot be measured due to irregular electrical activity. Both conditions involve the lower chambers of the heart, which are critical for pumping blood effectively.
Q: What is the management and treatment for VTach and VFib?
A: The management of VTach may include medications such as antiarrhythmics and defibrillator use if the patient is unstable. For VFib, immediate defibrillation is crucial, along with advanced cardiac life support (ACLS) protocols to restore a normal rhythm and prevent cardiac arrest and death.
Q: Can you explain the difference between ventricular tachycardia and ventricular fibrillation?
A: The difference between ventricular tachycardia (VTach) and ventricular fibrillation (VFib) lies in their electrical activity patterns. Vtach is characterized by a fast but organized rhythm of the ventricles, while vfib is disorganized and chaotic, preventing the heart from effectively pumping blood.
Q: What underlying heart conditions can lead to VTach and VFib?
A: Underlying heart conditions such as coronary artery disease, cardiomyopathy, and heart failure can lead to both VTach and VFib. These conditions disrupt the normal electrical signaling of the heart, resulting in these types of arrhythmias.
Q: What should one do if symptoms are related to VTach or VFib?
A: If an individual experiences symptoms such as rapid heartbeat, chest pain, or fainting, it is crucial to seek immediate medical attention. Prompt evaluation and treatment are essential to address the potential for severe complications, including cardiac arrest.
Q: How can the risk of developing VTach or VFib be reduced?
A: Reducing the risk of developing these arrhythmias can involve managing underlying health conditions, such as controlling blood pressure and cholesterol levels, avoiding excessive alcohol and stimulant use, and engaging in regular physical activity as advised by a healthcare provider.
Q: What role does defibrillation play in treating VTach and VFib?
A: Defibrillation is a critical treatment for V-fib, as it delivers an electric shock to the heart to restore a normal rhythm. In cases of VTach, defibrillation may also be necessary if the patient is unstable or if medications are ineffective in restoring a normal heartbeat.
The Bottom Line
VTach and VFib are both life-threatening ventricular arrhythmias, but their management differs drastically. VTach may allow for a brief window of intervention with medications or cardioversion, while VFib demands immediate defibrillation to restore a perfusing rhythm. Recognizing these rhythms quickly—whether on ECG or in a pulseless patient—can save lives.
Mastering these distinctions ensures the right action at the right time for healthcare providers. For patients at risk, preventive measures like ICDs and lifestyle modifications can be the key to avoiding sudden cardiac death. In emergencies, every second counts—knowing VTach vs. VFib could make all the difference.








 Login with Google
Login with Google Login with Facebook
Login with Facebook