Neurogenic shock and spinal shock are two distinct conditions often associated with spinal cord injuries, but they differ significantly in their causes, symptoms, and treatments. This article provides a comprehensive overview of these conditions, highlighting their key differences and the critical role of timely diagnosis and intervention in improving patient outcomes.
Understanding Neurogenic Shock
Definition and Causes of Neurogenic Shock
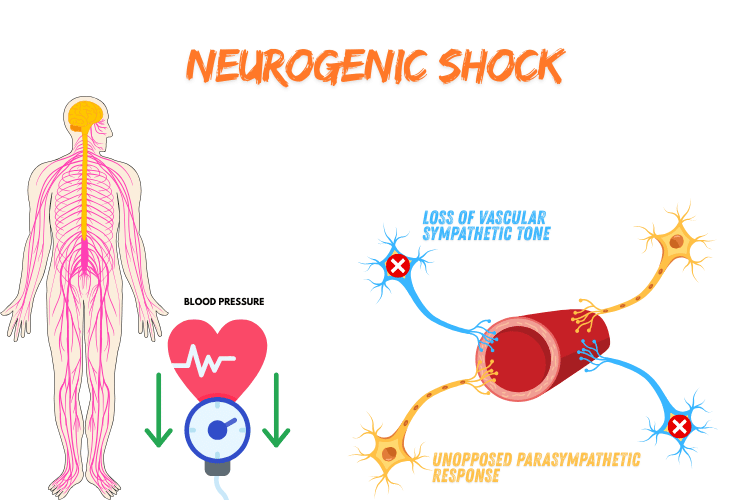
Neurogenic shock is a type of distributive shock that occurs when there is a disruption in the autonomic nervous system, resulting in a loss of vascular tone and subsequent pooling of blood throughout the body. This condition is often caused by spinal cord injuries, particularly those affecting the cervical or upper thoracic regions, which impair the sympathetic nervous system's ability to regulate blood vessel constriction. As a result, blood vessels dilate excessively, causing a significant drop in blood pressure and reduced blood flow to vital organs. Other potential causes of neurogenic shock include traumatic brain injuries, severe spinal anesthesia, or damage to the brainstem. In rare cases, conditions such as Guillain-Barré syndrome or multiple sclerosis may also lead to neurogenic shock by affecting the nervous system's ability to control vascular tone. Understanding the underlying cause is critical for effective treatment, as neurogenic shock requires targeted interventions to restore blood pressure and stabilize the patient.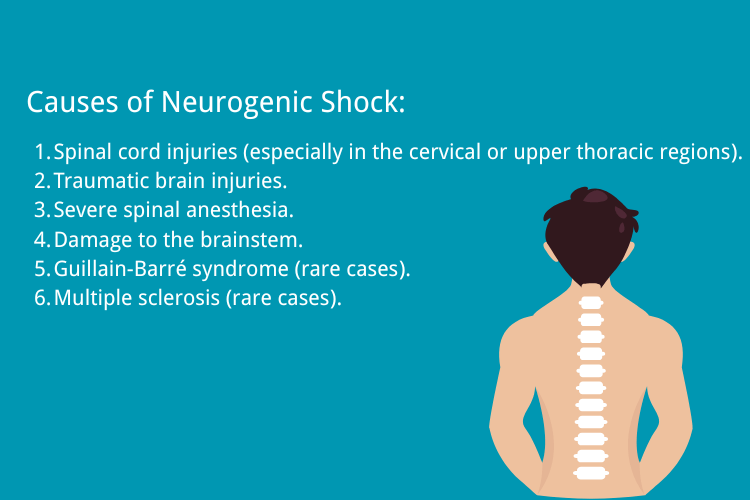
Neurogenic Shock Symptoms
The symptoms of neurogenic shock are distinct and often related to the loss of sympathetic nervous system function. One of the hallmark signs is a sudden and severe drop in blood pressure, known as hypotension, which occurs due to widespread blood vessel dilation. This is often accompanied by bradycardia, or a slower-than-normal heart rate, which is unique to neurogenic shock compared to other types of shock that typically cause tachycardia (a rapid heart rate). Other symptoms may include warm, flushed skin due to increased blood flow in the dilated vessels, as well as reduced urine output, which indicates poor perfusion to the kidneys. Individuals may also experience dizziness, fainting, or confusion as a result of decreased blood flow to the brain. In severe cases, neurogenic shock can lead to respiratory difficulties or even organ failure if not treated promptly. It is important to note that the symptoms of neurogenic shock can overlap with those of other types of shock, such as septic or hypovolemic shock. However, the presence of bradycardia and warm skin, along with a history of spinal cord or nervous system injury, can help differentiate neurogenic shock from other conditions.Diagnosing Neurogenic Shock
Diagnosing neurogenic shock requires a thorough evaluation of the patient’s medical history, symptoms, and physical examination findings. A key aspect of the diagnosis is identifying the underlying cause, such as a recent spinal cord injury or trauma, which provides essentialcontext for the condition. Physicians will also assess vital signs, including blood pressure, heart rate, and respiratory rate, to confirm the presence of hypotension and bradycardia. In addition to clinical evaluation, diagnostic tests are often used to rule out other potential causes of shock and confirm the diagnosis of neurogenic shock. Imaging studies, such as X-rays, CT scans, or MRIs, may be performed to identify spinal cord injuries or abnormalities in the nervous system. Blood tests can help assess organ function and detect any signs of infection or metabolic imbalances that could contribute to the patient’s condition. Advanced monitoring techniques, such as central venous pressure (CVP) measurements or arterial blood gas (ABG) analysis, may also be used to evaluate the patient’s circulatory and respiratory status. These tests provide valuable information about the severity of the shock and guide treatment decisions. Early and accurate diagnosis is essential for managing neurogenic shock effectively, as delayed treatment can lead to serious complications, including organ failure and death.Exploring Spinal Shock
Definition and Mechanisms of Spinal Shock
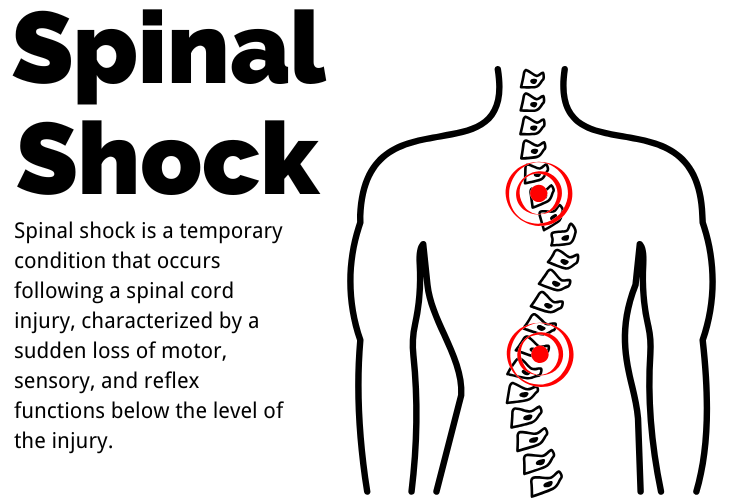 Spinal shock is a temporary condition that occurs following a spinal cord injury, characterized by a sudden loss of motor, sensory, and reflex functions below the level of the injury. This condition is not caused by physical damage to the spinal cord itself but rather by a disruption in the communication between the brain and the spinal cord. The loss of reflexes and muscle tone is due to the spinal cord entering a state of "shock," where it temporarily ceases to function properly.
The mechanisms behind spinal shock involve the interruption of neural pathways that control reflexes and voluntary movements. This disruption leads to flaccid paralysis, where muscles lose their tone and become limp, as well as areflexia, the absence of reflexes. Over time, the spinal cord may begin to recover, and reflexes can return, often in a hyperactive state. The duration of spinal shock varies, lasting from a few hours to several weeks, depending on the severity of the injury and the individual’s response to treatment.
Spinal shock is a temporary condition that occurs following a spinal cord injury, characterized by a sudden loss of motor, sensory, and reflex functions below the level of the injury. This condition is not caused by physical damage to the spinal cord itself but rather by a disruption in the communication between the brain and the spinal cord. The loss of reflexes and muscle tone is due to the spinal cord entering a state of "shock," where it temporarily ceases to function properly.
The mechanisms behind spinal shock involve the interruption of neural pathways that control reflexes and voluntary movements. This disruption leads to flaccid paralysis, where muscles lose their tone and become limp, as well as areflexia, the absence of reflexes. Over time, the spinal cord may begin to recover, and reflexes can return, often in a hyperactive state. The duration of spinal shock varies, lasting from a few hours to several weeks, depending on the severity of the injury and the individual’s response to treatment.
Symptoms of Spinal Shock
The symptoms of spinal shock are primarily related to the loss of neurological function below the site of the spinal cord injury. One of the most noticeable symptoms is flaccid paralysis, where the affected muscles lose their tone and become weak or immobile. This is often accompanied by areflexia, where reflexes such as the knee-jerk or withdrawal reflex are absent. These symptoms can make it difficult for individuals to move or respond to stimuli. Another common symptom is a loss of sensation below the level of the injury. This can range from partial numbness to a complete inability to feel touch, pain, or temperature changes. Additionally, spinal shock can affect autonomic functions, leading to issues such as low blood pressure, difficulty regulating body temperature, and loss of bladder or bowel control. These autonomic disturbances are particularly concerning as they can impact overall health and quality of life. As spinal shock progresses, some individuals may experience a return of reflexes, often in an exaggerated form. This phase, known as the "reflex recovery phase," is marked by spasticity, where muscles become stiff and overactive. Understanding these symptoms is crucial for managing spinal shock and providing appropriate care during each phase of recovery.Difference Between Neurogenic and Spinal Shock
While both neurogenic shock and spinal shock are associated with spinal cord injuries, they are distinct conditions with different causes, symptoms, and mechanisms. Spinal shock is a temporary loss of reflexes, motor function, and sensation below the level of the injury, caused by the spinal cord entering a state of functional shutdown. It primarily affects the nervous system's ability to transmit signals and is characterized by flaccid paralysis and areflexia. In contrast, neurogenic shock is a type of circulatory shock that occurs due to the disruption of the autonomic nervous system, leading to a loss of vascular tone and blood pooling. This condition results in symptoms such as low blood pressure, bradycardia (slow heart rate), and warm, flushed skin. Unlike spinal shock, neurogenic shock directly impacts the cardiovascular system and requires immediate medical intervention to stabilize blood pressure and circulation. The key difference lies in their focus: spinal shock is a neurological condition affecting reflexes and motor function, while neurogenic shock is a hemodynamic condition affecting blood flow and autonomic regulation. Both conditions can occur simultaneously in individuals with severe spinal cord injuries, making it essential to differentiate between them for accurate diagnosis and treatment.Spinal Cord Injuries and Their Implications
How Spinal Cord Injuries Lead to Neurogenic Shock
Spinal cord injuries (SCIs) can have profound effects on the body, particularly when they occur in the cervical or upper thoracic regions. These injuries disrupt the communication between the brain and the autonomic nervous system, which regulates involuntary functions such as heart rate, blood pressure, and vascular tone. When this communication is impaired, the body loses its ability to maintain vascular constriction, leading to widespread blood vessel dilation. This results in a sudden drop in blood pressure, a hallmark of neurogenic shock. Neurogenic shock is most commonly associated with injuries at or above the T6 level of the spinal cord. At this level, the sympathetic nervous system, which is responsible for the "fight or flight" response, is significantly affected. Without proper sympathetic input, the parasympathetic nervous system dominates, causing bradycardia (a slow heart rate) and further compounding the drop in blood pressure. This combination of low blood pressure and reduced heart rate can severely compromise blood flow to vital organs, making neurogenic shock a life-threatening condition that requires immediate medical attention.Effects on the Autonomic Nervous System
The autonomic nervous system (ANS) is divided into the sympathetic and parasympathetic branches, both of which play critical roles in maintaining homeostasis. Spinal cord injuries, particularly those affecting the upper spinal regions, can disrupt the balance between these two branches, leading to a range of complications. The sympathetic nervous system, which controls functions like increasing heart rate and constricting blood vessels, is often impaired in SCIs. This results in unopposed parasympathetic activity, which can cause bradycardia, hypotension, and difficulty regulating body temperature. In addition to cardiovascular effects, the disruption of the ANS can impact other systems. For example, individuals with SCIs may experience issues with bladder and bowel control due to impaired autonomic regulation of the urinary and gastrointestinal systems. Thermoregulation is another common challenge, as the body may struggle to maintain a stable internal temperature in response to environmental changes. These effects highlight the critical role of the ANS in overall health and the far-reaching implications of spinal cord injuries. The severity of autonomic dysfunction depends on the level and completeness of the spinal cord injury. Higher-level injuries, such as those in the cervical region, tend to cause more pronounced autonomic disturbances, while lower-level injuries may have less severe effects. Understanding these impacts is essential for developing effective management strategies and improving the quality of life for individuals with SCIs.Managing Spinal Cord Injuries
Managing spinal cord injuries requires a multidisciplinary approach that addresses both the immediate and long-term needs of the individual. In the acute phase, the primary goal is to stabilize the patient and prevent further damage to the spinal cord. This often involves immobilizing the spine, administering medications such as corticosteroids to reduce inflammation, and performing surgical interventions if necessary to relieve pressure on the spinal cord or stabilize fractured vertebrae. For individuals experiencing neurogenic shock, treatment focuses on restoring blood pressure and heart rate to normal levels. This may involve the use of intravenous fluids, vasopressors to constrict blood vessels, and medications to increase heart rate. Close monitoring of vital signs and organ function is essential to ensure that the body is receiving adequate blood flow and oxygen. In the long term, rehabilitation plays a crucial role in managing the physical and psychological effects of spinal cord injuries. Physical therapy helps individuals regain as much mobility and strength as possible, while occupational therapy focuses on improving daily living skills and independence. For those with autonomic dysfunction, strategies such as bladder and bowel training, as well as temperature regulation techniques, can help manage symptoms and improve quality of life. Advances in medical technology, such as spinal cord stimulators and exoskeleton devices, offer new hope for individuals with SCIs. These innovations aim to restore some degree of function and mobility, enhancing the overall outcomes for patients. By combining medical interventions, rehabilitation, and emerging technologies, healthcare providers can address the complex challenges posed by spinal cord injuries and support individuals in leading fulfilling lives.Treatment Approaches
Treating Neurogenic Shock
The treatment of neurogenic shock focuses on stabilizing the patient’s cardiovascular system and addressing the underlying cause of the condition. Since neurogenic shock results from a loss of vascular tone and autonomic regulation, the primary goal is to restore blood pressure and ensure adequate blood flow to vital organs. This is typically achieved through a combination of fluid resuscitation and medications. Intravenous fluids are often administered to increase blood volume and improve circulation. However, because neurogenic shock is caused by vasodilation rather than fluid loss, fluids alone may not be sufficient. Vasopressors, such as norepinephrine or dopamine, are commonly used to constrict blood vessels and raise blood pressure. These medications also help counteract the effects of unopposed parasympathetic activity, which can lead to bradycardia. In cases where bradycardia is severe, atropine may be administered to increase heart rate. Additionally, oxygen therapy is often provided to ensure that tissues receive adequate oxygenation. For patients with spinal cord injuries, immobilization and surgical interventions may be necessary to prevent further damage and support recovery. Close monitoring of vital signs and organ function is essential throughout the treatment process to ensure that interventions are effective and complications are minimized.Comparative Treatment of Spinal Shock
Unlike neurogenic shock, spinal shock is a temporary condition that resolves as the spinal cord recovers from its initial state of functional shutdown. Treatment for spinal shock primarily involves supportive care and monitoring, as there are no specific interventions to directly reverse the condition. The focus is on managing symptoms and preventing complications during the recovery phase. In the acute phase of spinal shock, immobilization of the spine is critical to prevent further injury. Medications such as corticosteroids may be used to reduce inflammation and swelling around the spinal cord, although their use remains a topic of debate among medical professionals. Physical therapy and rehabilitation are introduced as soon as the patient is stable to promote recovery of motor and sensory functions. As reflexes begin to return, spasticity and hyperreflexia may develop. These symptoms can be managed with muscle relaxants or antispasticity medications, such as baclofen or tizanidine. Long-term management focuses on addressing any residual deficits, such as bladder or bowel dysfunction, and providing psychological support to help patients adapt to their condition. While spinal shock and neurogenic shock share some similarities, their treatment approaches differ significantly due to the distinct mechanisms underlying each condition.Other Shock Types: Cardiogenic and Hemorrhagic Shock
In addition to neurogenic and spinal shock, other types of shock, such as cardiogenic and hemorrhagic shock, require unique treatment strategies tailored to their specific causes. Cardiogenic shock occurs when the heart is unable to pump blood effectively, leading to inadequate circulation. This condition is often caused by a severe heart attack, arrhythmias, or heart failure. Treatment focuses on improving cardiac output and may involve medications such as inotropes to strengthen heart contractions, vasopressors to maintain blood pressure, and diuretics to reduce fluid overload. In severe cases, mechanical support devices like intra-aortic balloon pumps or ventricular assist devices may be used. Hemorrhagic shock, on the other hand, results from significant blood loss, often due to trauma, surgery, or internal bleeding. The primary goal of treatment is to stop the bleeding and restore blood volume. This is achieved through fluid resuscitation with crystalloids or colloids, as well as blood transfusions to replace lost red blood cells. Surgical interventions may be necessary to control the source of bleeding, such as repairing a ruptured blood vessel or removing damaged tissue. While all types of shock share the common feature of impaired circulation, their underlying causes and treatment approaches vary widely. Understanding these differences is crucial for providing effective care and improving outcomes for patients experiencing shock. By tailoring interventions to the specific type of shock, healthcare providers can address the root cause of the condition and support the patient’s recovery.Frequently Asked Questions
Q: What are the symptoms of neurogenic shock?
A: Symptoms of neurogenic shock include a sudden drop in blood pressure (hypotension), a slow heart rate (bradycardia), and warm, flushed skin caused by widespread vasodilation. Patients may also experience reduced blood flow to vital organs, leading to confusion, dizziness, or altered mental status. Recognizing these symptoms promptly is critical, as neurogenic shock is a life-threatening condition that requires immediate medical attention.
Q: How does neurogenic shock occur?
A: Neurogenic shock occurs when a spinal cord injury disrupts the sympathetic nervous system, which is responsible for maintaining vascular tone and heart rate. This disruption leads to a loss of sympathetic control, causing blood vessels to dilate excessively (vasodilation) and resulting in low blood pressure. The reduced blood flow and oxygen delivery to vital organs necessitate swift medical intervention to stabilize the patient.
Q: What is the difference between neurogenic and spinal shock?
A: Neurogenic shock and spinal shock are distinct conditions that often occur after spinal cord injuries. Neurogenic shock refers to a cardiovascular response caused by the loss of sympathetic nervous system control, leading to hypotension, bradycardia, and vasodilation. In contrast, spinal shock is a temporary loss of motor, sensory, and reflex functions below the level of the spinal cord injury. While both conditions require immediate medical attention, their causes and treatments differ significantly.
Q: What treatments are available for neurogenic shock?
A: Treatment for neurogenic shock focuses on stabilizing blood pressure and heart rate. This often involves administering intravenous fluids to increase blood volume and using vasopressors, such as norepinephrine, to constrict blood vessels and raise blood pressure. Atropine may be used to manage bradycardia. Patients are typically treated in an intensive care setting, where close monitoring and resuscitation efforts are critical to improving outcomes.
Q: Can neurogenic shock lead to other forms of shock?
A: Yes, neurogenic shock can lead to or exacerbate other forms of shock. For example, if significant blood loss or fluid depletion occurs, it may result in hypovolemic shock. Additionally, in patients with pre-existing heart conditions, neurogenic shock can worsen cardiogenic shock. Prompt recognition and treatment of neurogenic shock are essential to prevent these complications and ensure better patient outcomes.
Q: What role does the autonomic nervous system play in neurogenic shock?
A: The autonomic nervous system, particularly the sympathetic branch, plays a crucial role in regulating blood vessel tone and heart rate. In neurogenic shock, a spinal cord injury disrupts sympathetic control, leading to widespread vasodilation, reduced vascular resistance, and hypotension. This loss of autonomic regulation significantly impairs blood flow to vital organs, making it a critical factor in the development of neurogenic shock.
Q: How does spinal cord injury contribute to neurogenic shock?
A: Spinal cord injuries contribute to neurogenic shock by damaging the nerves that control the sympathetic nervous system. This damage results in a loss of vascular tone, causing blood vessels to dilate and blood pressure to drop significantly. The impaired circulation reduces oxygen delivery to tissues and organs, making neurogenic shock a serious complication of spinal cord trauma.
Q: What is the triad associated with neurogenic shock?
A: The triad associated with neurogenic shock includes hypotension (low blood pressure), bradycardia (slow heart rate), and warm, dry skin. This combination of symptoms reflects the profound impact of spinal cord injury on the body’s ability to regulate blood flow and maintain cardiovascular stability. Recognizing this triad is key to diagnosing neurogenic shock quickly.
Q: When should someone seek immediate medical attention for neurogenic shock?
A: Immediate medical attention should be sought if an individual experiences symptoms of neurogenic shock, such as low blood pressure, slow heart rate, or warm, flushed skin, particularly following an injury or trauma that may involve the spinal cord. Early recognition and treatment are critical to preventing complications and improving the patient’s chances of recovery.
Conclusion
Understanding the differences between neurogenic shock and spinal shock is essential for effective management of spinal cord injuries. While neurogenic shock impacts the cardiovascular system, spinal shock primarily affects motor and reflex functions. Early recognition and targeted treatment can significantly improve recovery and quality of life for affected individuals.








 Login with Google
Login with Google Login with Facebook
Login with Facebook