
In a first aid training course, everyone must learn how to save a child's life because, as we all know, seconds matter. Kids tend to get themselves into every possible mischief, and thus, they are prone to several incidents. To handle such scenarios, parents or any adults in charge should know at least the basics of infant CPR techniques and choking relief. The strategies articulated in this article represent a valuable amalgamation of advice on what to do and what to avoid when dealing with an infant in an emergency. An even more serious risk of choking could be avoided altogether. We'll detail the methods for recognizing airway obstruction: back blows, chest thrusts, and CPR. Finally, practical ways parents can better protect their babies from harm and injury will also be discussed. Is there anything more important than protecting your loved ones? I’d bet not; therefore, knowing such techniques will undoubtedly help during times of crisis.
What are the initial steps for helping a choking infant?

- Assess the Situation
Confirm that the infant is choking by observing signs such as difficulty breathing, inability to cry or cough, or bluish skin coloration. If the airway is partially obstructed and the infant is coughing strongly, encourage them to continue coughing to expel the object.
- Call for Help
If the infant cannot breathe or is unresponsive, call emergency services immediately or have someone else do so while you begin administering aid.
- Position the Infant
Lay the infant face-down along your forearm, ensuring the head is lower than the chest. Support the infant's chin and jaw with your hand, being cautious not to cover the mouth or twist the neck.
These steps provide the foundation for assisting a choking infant and should be followed immediately by back blows and chest thrusts, as outlined in detailed first-aid practices.
How to recognize signs of choking in infants
With an infant’s choking, I look for signs such as, undoubtedly, the child having trouble breathing, being unable to cry and coughing, and the skin, especially the face and lips, appearing bluish. So, if my infant suddenly becomes quiet or starts to wheeze in a high-pitched tone, then most probably the child’s airway is blocked. Moreover, I also look to ensure the child is not panicking by clutching their throat or having a concerned look on their face; therefore, I know that the steps need to be taken quickly. For such an instance, knowing such signs and recognizing them quickly enables one to assist better.
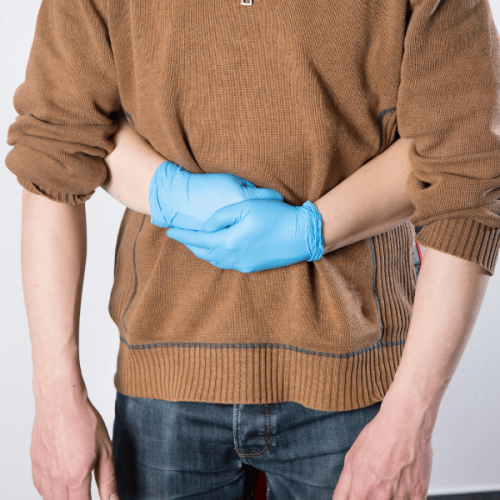
Proper positioning of the infant for choking care
To allow the correct angle to the chest thrusts and blows and at the same time reduce the likelihood of an injury, proper positioning should always be ensured when helping a choking infant. Pick the infant up in a manner where he is, for example, along your forearm, making sure that the infant’s head is lower than the infant’s chest, which allows gravity to be more practical about the issue at hand. With one of your hands, cradle the infant's jaw to support the head and neck, but your palm must not be directed towards the throat, jamming it. To give yourself some support, your forearm can be placed over your thigh, providing enough support and pressure but not causing considerable pain.
If back blows seem inefficient, the infant should be turned to a position where the infant is facing up, but the infant’s head has to remain in a lower vicinity when compared to the sternum to be effective. Your lap or forearm can still be used so that your jaw and neck, in particular, can be supported. In this way, it is possible to drive the thrusts well to the lower portion of the rib cage that will go roughly 4 centimeters deep in respective pediatric cases on aid. Every time you perform a thrust or a previously stated action in the provided pointers, always look inside the mouth after each attempt to ensure something is not still blocking the way. Keep shifting between back blows and chest thrusts until assistance or the object is freed.
When to call for emergency assistance
In cases where the baby is still unresponsive, or the obstruction is not resolved after performing back slap and chest thrust techniques, seek emergency medical assistance. Similarly, if a baby’s color turns bluish, he does not cry and appears unconscious, necessitating calling emergency medical assistance. In any case, while rendering care, keep trying to clear the airway until the doctors reach, using pediatric first-aid to ensure that the baby is breathing and is responsive throughout. In addition, if you notice that the pulse is weak or if the body is limp or drooped, such a person, too, should be regarded as requiring medical attention.
How do you perform back blows on a choking infant?

When a baby chokes, back blows can be given, however before that, the baby’s head and neck should be supported first. Then, place the baby face down on your forearm using your thigh or lap to help the infant, and make sure the baby’s head is lower than their chest. Stand behind the baby and use your hand to strike the area between the infant’s shoulder blades five times. Careful not to hit too hard; remember, there’s an obstruction you’re trying to remove. One air passage is open; perform chest thrusts as required. Surrounding the process, the condition of the infant must be monitored.
Correct technique for administering five back blows.
To give five firm back contacts to a choking infant who is at risk of asphyxiation, I would recommend that their head and neck be supported gently. The infant was placed at the top of my forearm to position his head lower than his chest while my forearm rested on my thigh or lap for support. Five mighty and pinpointed blows between the infants' shoulder blades would be administered using the heel of my palm. Care would be taken not to hit targets too hard, but each contact would be driven enough to dislodge the item blocking the airway. After the completion of the five slaps on the back, my next step would be to check the baby’s mouth to see if a breath was taken and to evaluate whether or not the obstruction had been dislodged. If this was not the case, I moved on to the next step, which was applying chest thrusts while closely watching their level of unconsciousness.
Positioning the infant along your forearm for back blows
The first step would entail firmly securing the child, ensuring their face is contorted towards the ground while my elbow rests on my thigh. I would place one hand, which is very helpful, under the child’s jaws, neck, and head, ensuring that their head is below the rest of their body to exert the required force from gravity so that I can easily administer back blows to the infant. I would also ensure that the infant's body is aligned with my forearm at any gap, which would be the head control during the process. The aim is to maintain the infant’s lower head and upper chest view at around a 30-degree angle from my standpoint, even as a slight tilt from the palm or the fingers is allowed so that the infant does not suffer any additional injury and cross-contamination to the minor injury does not arise from too much force being exerted.
What to do if back blows don't dislodge the object
If removing the obstructed object with back blows is impossible, start with chest thrusts. At this point, support the head and neck and rotate the infant onto the back. The infant’s head should always be lower than the chest, and the infant should be placed so that his/her head is kept in the forearm and thigh. With the non-dominant hand, place 2 or 3 fingertips onto the lower part of the sternum, about half an inch underneath the line connecting the nipples and above the xiphoid process, which is injury-prone. Following this, a thrust should be made by pressing firmly on the chest by about 1.5 inches (4 centimeters), performing a total of five. Ensure all the compressions are executed fully and allow the chest to withdraw between each compression fully.
The diaphragm located laterally of the ribs may be of aid if appropriately positioned. The two should always be alternated until professional help arrives, the object is let out, or the baby is allowed out. If the baby is not responsive, ask for emergency services. No more than a singular back blow and a singular push should be used unless a professional can modify them. Every step required must be taken as stated to minimize any risk of injury.
What are the proper chest thrust techniques for infant choking?

When dealing with infant choking and applying chest thrusts, it is pertinent that a step-wise procedure is followed to uphold safety and deal efficiently with the infant. Chest thrusts are an excellent alternative for performing CPR on infants who are one and younger. First, place the infant on a solid surface or your lap face-up while supporting their head and neck. Next, with the help of two fingers, locate the lower half of the sternum, ensuring that the xiphoid process remains untouched and laying on the mid nipple line, then proceed to apply five quick compressions by pushing inwards around 4 cm deep with enough force whereby the upward movement achieves blockage loosening, this should result in the infant experiencing an upward movement. When the infant breathes out, do not soldier on; allow the breathing to resume tension-free thanks to the applied chest thrust. Continue doing these backward until the infant stops breathing and begins to fall unconscious; whereby when this starts to happen, briskly move the infant to CPR and report the emergency services. Bearing all this in mind, upper body thrusts must be applied with appropriate concentration and hurtness so as not to impact the overseer of the task.
How to perform five chest thrusts on an infant
- Position the Infant
- Lay the infant face-up on a firm surface, or place them on your lap.
- Ensure the infant’s head and neck are fully supported to prevent injury.
- Hand Placement
- Locate the lower half of the sternum, just below an imaginary line connecting the nipples.
- Avoid pressing on the xiphoid process (the end of the sternum) to prevent damage.
- Apply Chest Thrusts
- Use two fingers to deliver five quick compressions.
- Compress the chest approximately 1.5 inches (4 cm) deep.
- Technique
- Apply the force in an upward motion to help dislodge the blockage.
- Allow the chest to recoil between each thrust to maintain effectiveness fully.
- Monitor and Repeat
- Closely observe the infant for signs of improvement or distress.
- Repeat the cycle of 5 chest thrusts and five back blows, alternating as needed.
- Emergency Action if Needed
- If the infant's condition does not improve, initiate CPR immediately.
- Activate emergency services without delay.
Accurate execution of these steps is critical to ensuring the infant's safety and recovery. Always prioritize proper technique and act decisively in time-sensitive situations.
Correct Hand Placement for Infant Chest Thrusts
Proper hand placement is essential when performing chest thrusts on an infant to ensure effectiveness and minimize the risk of injury. Follow these guidelines for accurate technique:
- Identify the Correct Location
- Locate the lower half of the infant's sternum, approximately one finger-width below an imaginary line drawn between the infant's nipples.
- Avoid placing your fingers on the xiphoid process or the ribcage to prevent potential injury to internal organs.
- Position Your Fingers
- Use two fingers, typically the index and middle fingers, to perform the chest compressions.
- To maintain proper mechanics, ensure the fingers are positioned vertically on the sternum and apply force perpendicularly to the chest.
- Depth and Force Parameters
- Compress the chest to a depth of approximately 1.5 inches (4 cm).
- Apply smooth, controlled force to generate sufficient pressure without causing harm.
- Allow Recoil
- Between compressions, ensure the chest fully recoils to allow the heart to refill with blood and maintain the effectiveness of circulatory support.
Precise and controlled finger placement is critical for effective chest thrusts while preventing injury. Individuals trained in infant first aid are recommended to practice and adhere to these technical parameters frequently.
Alternating between back blows and chest thrusts
In cases of airway blockage in an infant, switching chest thrusts and back blows appears to be one of the best strategies. I preface it by giving the baby five smooth back blows, using the base of my palm in a massaging way, directed to the space between the baby’s shoulders. I ensure that the back is supported and the baby’s head slumps down to let the back work properly. After this, I place the baby on her back, and with the second two fingers, which are positioned in the lower part of the breast bone, I perform five chest thrusts in a suitable environment. With slightly increased pressure, each thrust compresses the sternum at a rate of 5 cm (2 in) in round motion until the desired depth of 4 cm has been reached. This procedure is continued, and the number of back proxies and chest thrusts interchange until the blockage clears or advanced medical help is available. I also look for very faint signs of improvement, like the baby is grieving, coughing, or even trying to clean her nose with each throat during this phase. The ability to master the transfixing technique and the rhythm of force application are the two determinants of success in avoiding injury.
When should you start infant CPR during a choking episode?

To commence with, infant CPR should be carried out only in case of a choking episode where gasping has not been present in minimal amounts but is accompanied by an infant who has lost consciousness and is not breathing. Is it acceptable to assume American Parents do not require a medical professional to call for assistance? Things will be rational. Proceed first with starting American Parent CPR, first doing compressions. Wait for the address to circulate oxygen for further assistance. Voilà! All the steps are completed rather effortlessly.
Signs that an infant has become unresponsive
I care for kids and observe their reactions whenever a noise is made, or someone tries to touch the baby or call their name. I realize there is an issue if they are unresponsive to any of this. There are specific indications for this, such as lack of movement or breathing irregularities like gasping or temporarily stopping breath altogether. I also notice their skin color, as it can turn greyish white from the pale it was before around the fingernails and lips. These are quite a few indications that show a child may require immediate attention, such as CPR.
Transitioning from choking care to infant CPR
Immediately when switching from applying measures to relieve a child from choking to performing CPR, the first step I take is grasping the child with a firm grip and laying them down flat on my arm while my other hand blows air gently onto the child’s back. The minute I feel the need to provide infant CPR, I lay the infant on a firm, flat surface, and first check if the child is breathless. If the child is especially taking sharp, short breaths, I start infant CPR, comprising 30 flat hand compressions followed by two gentle breathing exercises. This is crucial, similarly after providing each measure of broad hand compressions or breathing on the child, I keep on a lookout for knobs that indicate the baby’s responsiveness level or if the baby was able to breathe easily or not.
Performing chest compressions on an infant
Being gentle and careful while performing chest compressions on an infant is very important. Compressions can only be effective if they are correctly performed and the risk of injury is minimized. The first step is to lay the infant on a table or the floor. Then, place the two middle fingers or the index fingers of one hand on the breastbone near the lower part of the chest and above the mid-nipple line. Ensure that your fingers are not placed on the xiphoid process, the sternum's end, to avoid injuring internal organs.
Make compressions to a distance of 1.5 inches (also 4 centimeters) or one-third the distance from the front to the back of the infant’s chest. Rest your elbow on the table or the floor for a stable contraction position, and keep your elbows locked. Then, place your thumb straight to focus on maintaining a pumping speed of 100 to 120 pumps in a single minute. When breathing, however, pull your thumb away during contractions. This specific technique a vigorous contraction can combine effective cardiac filling and blood circulation.
Coughing/ache is pressing two breaths after 30 compressions only after ensuring the head is in a neutral position with a slight chin lift. To accommodate various levels of training, breathing over chest compressions may be adjusted to 2 over 15, but this requires one more trained rescuer. Attempt to focus on performing deletions of compressions before apparent signs surface, promising consistency until oxygenation resumes or noted medical responders are visible.
Key Physical Parameters:
- Compression Depth – of Approx 4cm or extending above an inch or third of the chest depth.
- Compression Frequency – Anywhere between 100 and 120 cpm.
- Approximate Compression-to-breath ratio (1 Breath Rescuer)- 30 Compressions to every two breaths.
- Approximate Breathing over compression ratio (2 Breath Rescuer)- 15 Compressions to each two breaths.
- Allow the chest to be released entirely in between direct pressures.
Dealing with these technological parameters guarantees that the infant receives a range of interventions with the highest chance of producing a good result.
What should you do if the infant expels the object?

In case the child dies an object, instantly make sure that the child’s airway is free and he or she is breathing appropriately. Watch for natural breathing, crying, or movement of the chest. If the infant does not seem to have any breathing issues, wait for the health practitioner to arrive while keeping the infant calm and under close surveillance. If the infant shows an inadequate breathing pattern or appears to be restless, then proceed with the necessary life-saving actions, such as rescue breaths; also, call the beneficiaries of emergency services and follow their instructions.
Assessing the infant's breathing after object removal
Once the object is dislodged, I would examine the infant’s respiration by confirming the appropriate movement of the chest and listening for any clear sounds of the airway or airflow through the nostrils and mouth. I would reassure them and make sure they are comfortable and in a secure position. Subsequently, I would closely monitor them and contact medical personnel if necessary. However, if the baby does not breathe or breathes erratically, then I would provide artificial respiration and, in some cases, commence the CPR following the laid down guidelines and, at the same time, notify the emergency services.
Monitoring the infant's condition post-choking incident
A close watch is warranted following a choking incident involving the infant to ensure that no complications are remaining. In the case of the infant, observe if there is labored breathing, persistent cough, wheezing, or change in the skin color, especially pallor or cyanosis, which indicates an obstruction or airway irritation. Look for signs like abnormal movements of the chest, which may mean there is difficulty in exchanging air.
If the infant is calm and writhing normally, it can be placed comfortably, and monitoring should be continuous for the next 24 hours. Nevertheless, tiredness, refusal to eat, or drowsiness may be a sign of more serious complications, such as aspiration pneumonia with airway trauma; therefore, an examination should be carried out immediately in these instances.
The technical parameters that one has to Monitor include the following:
- Respiration Rate: For children aged below one year, this should be between thirty to sixty in a minute.
- Heart rate: From 100 to 160 beats per minute is infants' average resting heart rate.
- Oxygen saturation (SpO2): It must be between 95% and 100%, and anything less than 90 is a critical situation that necessitates immediate action.
Where there is deviation from typical values, pediatricians or the emergency services must be called for further assessment. Also, if the infant looks stable, visiting a doctor for a follow-up appointment is best to ensure no late complications develop.
When to seek medical attention after a choking episode
In case you or anybody else has choked, a medical professional should be contacted in certain situations. In such cases, I am not even sure how breathing becomes easy, but talking becomes impossible - it’s as if something was left inside the throat. Other common symptoms include persistent coughing or wheezing, so I strongly recommend contacting a medical professional if you have any questions. Furthermore, ingestion of waxy cyanosis (internal inability to breathe sharply that causes blue skin or lip color), intense strain in the area around the chest, or any slight known or unknown unconscious moment during the episode also requires medical attention. In some cases, even the complexity of aspiration pneumonia that the individual passes through must be monitored. Another distress signal to monitor is oxygen saturation levels dropping below normal (94%) - which can be measured using a pulse oximeter, or an abnormal decrease or increase in the adult's respiratory rate (less than 12 or more than 20 breathes a minute) as this can indicate a medical emergency.
References
Choking Hand Respiratory tractFrequently Asked Questions (FAQ)
Q: What are the first steps in helping a choking baby?
A: If a baby is choking, the first steps are to give up to 5 quick back blows followed by up to 5 chest thrusts. Hold the infant face down on your forearm, supporting their head, and use the heel of your hand to deliver firm back blows between the shoulder blades. If this doesn't dislodge the object, turn the baby face up and give chest thrusts using two fingers placed in the center of the chest.Q: How do I perform infant CPR if a baby becomes unresponsive?
A: If an infant becomes unresponsive, start CPR immediately. Place two fingers in the center of the chest and give 30 quick compressions, followed by 2 rescue breaths. Continue this cycle until help arrives or the infant starts breathing on its own. Proper training from organizations like the American Red Cross is crucial to performing this life-saving technique correctly.Q: What should I do if I can see the object causing the choking?
A: If you can see the object causing the choking, try to remove it only if you can easily grasp it. Never perform a blind finger sweep, as this may push the object further down the airway. If you can't easily remove the object, continue with back blows and chest thrusts until the object is dislodged or the infant becomes unconscious.Q: Are there any choking hazards I should know about for infants?
A: Yes, common choking hazards for infants include small objects like coins, buttons, small toys, and parts of larger toys. Whole grapes, hot dogs, nuts, and hard candies are also dangerous. Always supervise infants during feeding and playtime, and keep small objects out of reach.Q: How can I learn infant CPR and choking first aid?
A: You can learn infant CPR and choking first aid through certified courses offered by organizations like the American Red Cross. They provide hands-on training and practice with infant mannequins. Additionally, the Red Cross offers a first aid app that provides quick reference guides for emergencies.Q: What's the difference between helping a choking infant and an older child?
A: The main difference is in the technique and force used. For infants under one year, you use back blows and chest thrusts. You use abdominal thrusts for children over one year (Heimlich maneuver). The force used for infants is also gentler due to their smaller and more delicate bodies.Q: When should I call emergency services if a baby is choking?
A: You should call emergency services immediately if the infant becomes unresponsive, turns blue, or if you've performed multiple cycles of back blows and chest thrusts without success. If possible, have someone else call while you continue first aid efforts.Q: How can I prevent choking incidents in infants?
A: To prevent choking, always supervise infants during meals and playtime. Cut food into small, manageable pieces and avoid giving them foods that are choking hazards. Keep small objects out of reach, and regularly check toys for loose or small parts. It's also essential to create a safe environment and educate caregivers about choking risks and prevention.













 Login with Google
Login with Google Login with Facebook
Login with Facebook