
When a child is choking, there is very little time to waste with starting aid methods as they will get worse by the second. If the information and help is given in time, it has the potential to save a life. The present content highlights the knowledge and lacunae related to first aid techniques for a child who is at risk of choking. Oxygen is asphyxiated. Suffocation means removing it. First, we will help the reader grasp the information and terminology crucial for applying artificial respiration (CPR) or Heimlich maneuver. Moreover, this will be emphasized by removing all the common blunders in managing the medical event and referring to further training material. After equipping oneself with these core skills, it would be easy to understand how to tackle most of the aggressive, life-threatening situations many parents may encounter.
What are the signs and symptoms of a choking child?

When a child is choking, looking for both physical and behavioral indications is essential. Frequently, the following can serve as identifiers:
- Difficulty in Breathing: The child may inhale and exhale with considerable effort and sometimes seem agitated.
- Noisy or Quiet Crying: The child may have suffered an injury that is damaging enough to cause him/her not to speak or cry actively.
- Coughing or Gagging: The child may also cough or gag to push out whatever is blocked.
- Cyanosis: A pale skin coloration can also be caused by a deficient oxygen supply.
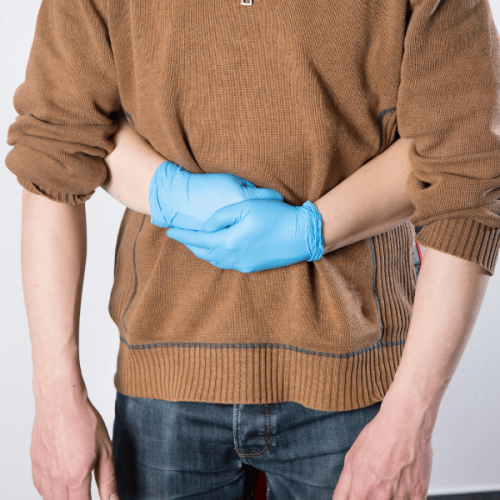
- Holding the Neck: Whenever a child is choking, attempting to speak out can cause him/her tremendous irritation. Choking is a common ailment for any child.
- Low or no Respiratory Sound: There can also be a situation where the airflow is very weak, leading to weak or no sounds at all.
If appropriate measures are not taken it can lead to unforeseeable serious issues, thus the above signs need to be attended to instantly.
How to recognize if a child can't breathe due to choking
Observe specific cues to know whether a child has difficulty breathing because they are choking. I would look for a sign of whether the child tries to talk, cry, or make any sound, indicating a complete airway obstruction. In addition, their facial expressions would give me an idea; for instance, if they have a panicky or scared look, it could be a warning. The presence of a child with this behavior, plus the child having a blue skin or blue lips (cyanosis) would be sufficient evidence to ascertain the low oxygen level. These visual and behavioral cues help me determine the situation, respond to it accordingly, and clear the obstruction in his throat without wasting time.
What are the differences between mild and severe choking?
A person’s ability to breathe is mildly choking if they cannot speak or do things requiring air intake. In mild choking, however, a person can still make sounds or, for that matter, cough forcefully. In this case, Forceful action would be an attempt by the body to shrug off the obstruction in the airways, bending a person to cough. This cough reflex automatically triggers the expulsion of foreign objects from the windpipe. The following mild signs can appear as redness on the face, but the patient doesn’t have silicosis, which makes oxygen levels sufficient.
In contrast, muscle contraction preventing the expulsion of wind from the lungs denotes severe choking. In all cases speaking, cursing, coughing, and any sound remains impossible. Choking is a mess of fear. That, along with a grasp of the throat, has become a symbol of choking. The bluish tint of skin and lips is a sign of suffocation, and it persists until the body gets adequate oxygen supply. Rescuing measures, including force to belly and back massage, are required as the Risk of passing out makes a life-threatening circumstance lasting roughly five or fewer minutes.
When should you start first aid for a choking child?
If a child is choking severely (cannot cough, speak, cry, or breathe), first aid should be commenced without wasting a second. Understand the universal choking sign: clutching at the throat, cyanosis, or absence of any sound - all these indicate the person cannot inhale air and the airway is completely blocked. If the child can cough vigorously and make some noise, ask him to continue coughing, but don’t assist him. To clear up severe choking, start with back blows and abdominal thrusts as soon as possible. Do five back slaps and five chests make chest thrusts instead of abdominal thrusts on infants under one year? In case the child has stopped responding or is unconscious, start performing cardiopulmonary resuscitation (CPR) and simultaneously call an emergency officer. During these treatments, the child’s head and body are always in a comfortable position.
How do you perform the Heimlich maneuver on a choking child?

To give a one-year-old choking child Heimlich, start by standing or kneeling behind him, clasping around his waist with his arms as he bends over. One hand should be formed into a fist and placed between the ribcage and navel of the child. With the other hand, grasp your fist and push in and up against the child. If this causes a child to stop being able to breathe or the inserted object has not been pushed out at this point, then continue with each push of ‘inward’ and ‘upward’ as a child’s motion. If the child stops breathing, lay the child flat on a firm surface for CPR and make sure to contact emergency units. A child older than a year can be given this procedure, but a child younger than a year should not have this procedure done on them as this can cause them harm.
Step-by-step guide to abdominal thrusts for children
- Secure the Child’s Position: Stand or kneel behind the child while holding the center of their waist.
- Make a Fist: With one hand, make a fist; this fist will go above the belly button and below the ribcage.
- This is what I call the pivot hand: Hold your other hand around your eight; this will help keep the thrust in place.
- Come closer together: By pulling the child closer to your hand, you aim to complete the thrust, which should push the object attached to the airway away.
- Repeat or Ignore: Last Resort! Try all means while making sure that the child is still ready to try something new. Control every thrust made by the child, and if the child does give up, then clearly, every force controlling them or aiming to control them must have been too much.
- Dial Apart from Your Standard Number: Utilize CPR efficiently in an emergency scenario with the assistance of medics or first responders. Never forget that other techniques are helpful when surpassing one-year-old infants.
What to do if the Heimlich maneuver doesn't work
If the Heimlich maneuver fails, I would suggest contacting emergency services as they provide better assistance. In the meantime, place the child on a hard surface while observing if they can respond and breathe. If the child cannot answer, voluntarily perform cardiopulmonary resuscitation on him or her.
In case of choking, CPR is performed as follows: 30 chest compressions followed by a visual mouth check to see if the object can be dislodged, and then two breaths are given. For children, compress to a depth of about 5 cm at 100–120 compressions per minute. If you see something in the child’s mouth, try to grasp it with a finger; however, ensure not to insert your finger in the mouth deeper as it could send the object more profoundly into the child’s throat. Breathe into the child’s mouth two times, but do not attempt to supply both breaths simultaneously. If, after a few cycles, the child is still unconscious, don’t give up; control the chest area, thrust, and pump the child until the object is removed or help arrives. Children younger than one year do not perform abdominal thrusts or chest compressions. They are replaced with deep back slaps.
What are the choking first aid techniques for infants and toddlers?

The recommended approach indicates that the infant should be put face down on one’s forearm while the other hand holds the infant. Five back slaps should be directed between the infant's shoulder blades, employing the palm's root. In case the choke is still intact, the infant user is turned such that she is facing upwards and then using two fingers in between her nipple and her jaw, pushing sharply and thrusting the bottom half of his hand at the middle of the infant’s chest. Keep alternating between the two procedures until the obstruction is displaced or the infant begins to breathe.
The procedure is now put into use for a toddler that is more than a year old, the abdominal thrusts (Heimlich maneuver) are performed by standing behind the child and encircling the child’s stomach area with both hands one of which is closed into a fist which is placed above the navel. A child can be asked to undergo a couple of quick inward and upward thrusts till the airway is apparent. In case the child does not respond, then CPR is commenced alongside looking in the child’s mouth for any object that might be in there. Compression of the waist continues until there is a clear airway, which means that CPR has to be used, which, at times, could be unsuccessful.
How to perform back blows and chest thrusts on babies.
To initiate chest thrusts and back blows on an infant, I would first position the infant face down over my forearm, supporting the head and neck. Then, I would take the heel of my palm and strike in between the shoulder blades five times bluntly. If the o is still lodged in the throat, I would then rotate the baby on the back and use two fingers to apply pressure on the chest five times, just below the nipple line. These sequences would be performed continuously until the airway is cleared or the baby resumes breathing independently. If the baby fails to respond, I would administer CPR and stay vigilant, looking for any o in the baby’s mouth during the intervals of every cycle of compression. Finally, even after the successful removal of the obstruction, I would make it a point that medical provisions are sought out for the baby.
When to use two-finger chest compressions for infants
When an infant who does not respond and has an absent or weak breath, I would perform two-finger compressions on their chest. This technique is portrayed as part of infant CPR. It consists of two fingers placed in the center of the chest and compressing the nipple area to a distance of approximately 1.5 inches with a frequency of 100-120 compressions in a minute. If I am alone or I have another rescuer in the Alternating appendix, I would perform a 30:2 or 15:2 ratio, respectively, until the help of medical experts is required or the baby resumes ventilation.
What to do if a toddler is choking but still conscious
In case a toddler is struggling but is still able to cough and breathe on their own, I would tell them to leave the obstruction on their own as this means the majority of the toddlers can be able to overcome the situation. However, if its not possible, then I would perform a maximum of five back pats, followed by five abdominal thrusts while employing the Heimlich maneuver. To perform a backward pat, I would make the waistband of the toddler sit a little above the navel whilst holding their hand and then strike between their shoulder blades with the heel of my hand. Similarly, to perform an abdominal thrust, I would hold them standing at the back, place a fist slightly above their navel, and then push them up in a quick upward direction. The toddler would be pushed between these methods until they pass the object, or they would not remain conscious.
Compliance issues to be concentrated on:
- To reduce the risk of injuries, keep an eye on the child and maintain comfort and balance during the techniques.
- During backward pats and abdominal thrusts, apply gentle force as the aim is to touch, not hurt.
- Remember, if toddlers cannot cough out the hindrance independently, they require medical attention instantly.
What should you do after successfully dislodging the object?

After removing the lodged object, it is essential to watch the child for signs of respiratory distress like coughing, wheezing, and shortness of breath. Check their behavior and ensure they have no breathing or swallowing problems. If any such issue is apparent, always go for a medical checkup to rule out any particular internal damage because there could have been internal injury when the obstacle was present or even while using methods to remove it. Ensure pediatric needs are handled by addressing any secondary issues in all cases.
How to check if the airway is obvious
To ascertain the patency of the airway, I first assess how well the toddler breathes without distress, including wheezing or gasping, which is an effort. I monitor if normal sounds occur when they breathe in and out, including not noticing signs that the airway is partially obstructed. Then, I evaluate whether the toddlers can cough or emit cries or normal sounds, an essential criterion for an open airway. Finally, I check the color of their skin; if it is pale or bluish tinge, there is a strong possibility that the oxygen supply is low. Otherwise, these signs don’t concern me at all.
When to seek medical attention after a choking incident
Choking incidents are critical moments that require immediate medical assistance. The occurrence of recognizable symptoms such as the following must be stated below:
- Breathing Difficulty: A child who struggles to breathe due to wheezing, high tones, or gaps should be evaluated by the doctor immediately as those indicate serious medical problems of limitations in the air passing through or damage to the windpipe.
- Constant Coughing or Gagging: The presence of foreign objects in a child's windpipe is always alarming. If the child tends to cough or gag continuously after the incident, they should be provided with professional assistance or care.
- Skin Discoloration: Blueish substances around the face, lips, or even parts of the body are a clear indication of oxygen supply disruption, and they must be controlled or reported as soon as possible.
- Loss of Consciousness: Tension increases when children start losing consciousness during or after the choking episode, so call for specialized medical professionals without wasting any time.
- Unusual Behavior: If a child suddenly becomes overactive or less active than normal after a choking incident, there is a possibility of oxygen supply disruption during the incident.
- Trouble in Swallowing: Not being able to swallow food or experiencing severe pain after coughing requires immediate assistance or guarantee because the sensation suggests choking.
Technical Parameters to Monitor:
- Respiration Rate: Toddlers typically take 20-30 breaths every minute; any major change in that range warrants an expert opinion.
- Oxygen Saturation Levels (SpO2): SpO2 levels should ideally be between 95% and 100%. Measurements less than 92% should raise concerns, as it is considered low.
- Pulse Rate: The average normal range of heartbeats per minute in children is around 80 to 130 while at rest. If these rates are higher or lower than expected, they would signal stress or a lack of oxygen.
As a general rule of thumb, for any instance of choking that has not entirely rectified itself or when the child is found to be in bad shape after the episode hell, it is likely for you to seek a medical consult.
What follow-up care is needed for a child who has choked?
If your child has had a respiratory incident, it is essential to watch them closely for any lasting signs of discomfort. Look out for such complaints as a persistent cough, some wheezing or difficulty breathing, swallowing, or the signs of an obstructed airway, as these may indicate that the airways are irritated or some obstruction may be left. It is better to be safe than sorry, and even if your child looks okay at first, call in for a check-up at a doctor’s clinic to rule out the possibility of any other complications, e.g., aspiration pneumonia. On such occasions, the physician might just carry out a thorough physical examination or order some imaging, like a chest X-ray, to verify that the child’s airway and lungs are free from obstruction. Whenever there is such a vacuum, the evaluation of the patient should be given overriding urgency, more so when the child presents with stubborn signs that just won’t go away or when they start getting worse.
How can you prevent choking hazards in children?

To reduce choking hazards for children, it is crucial to always keep an eye on them while they eat and snack. Foods should be cut into small, easy-to-swallow pieces, such as cutting grapes or cherry tomatoes in half. Try not to provide children with foods like hard nuts, large pieces of meat, sticky popcorn, or anything else that large chunks of them have to chew, especially for younger children. Ensure that toys and items in the house do not contain small parts that can get stuck in the airway. Always use age-appropriate feeding methods and toy guides, and teach the child to eat slowly and chew properly. Most importantly, everyone would feel more secure if they learned some first aid and how to help someone choke, for example, by learning how to do the Heimlich maneuver.
What are everyday objects that cause choking in children?
Kids are good at putting anything and everything into their mouths. This includes small toy parts, buttons, and even coins, which can be a choking hazard. Other food items such as grapes, nuts, and even popcorn could also lead to choking. To combat this, I avoid all of these mitigating factors to minimize the amount of risk present while keeping an eye on my kid during mealtime and playtime.
How to create a safe eating environment for young children
It is essential to ensure that children receive adequate adult supervision, meals are adequately prepared, and the actions concerning the level of food offered to children are appropriate. Ensure children remain seated and relatively still to avoid choking on the food provided. A high chair fastened with a safety belt should do well because it will restrain toddlers’s movements while letting them eat. Large pieces of food like grapes and cherry tomatoes should be sliced into smaller pieces; instead of large rounds, place hot dog pieces into small strips. Never offer these foods in large quantities. Nuts, hard candies, and sophisticated peanut butter-coated hanging segments are a few examples of these foods.
First and foremost, avoid any action that impedes the child's concentration levels while they eat. Attempting to speak, bursting into laughter, or even running around can lead to choking, which must be avoided at all costs. Always ensure that the child is provided with any bending cutlery, non-splash-consuming cups, or any age-appropriate hook or plate. Likewise, pay attention to the feeding space by removing small objects that may cause choking; this will also maintain a smooth feeding environment. Additionally, kids need to be trained on how to chew well and eat slowly so that they develop good habits early in life and there are no choking incidents.
Last, but not least, all caregivers must be taught the Heimlich maneuver or giving back taps in a child choking incident, which amplifies their understanding of the situation exponentially and, more so, could save a life. Out of the in-depth guidelines defined, comprehension of how to pick up a child off their high chair, how to keep them safe at a table, and other fine details surely come as a high-value bonus as they decrease the chances of lack of comfort during eating, promoting a better experience for younger children.
What age-appropriate foods can help prevent choking risks?
To reduce the risk of choking, I aim to give my child foods that are soft, small, and easy enough to chew or swallow. If the kid is aged four and below, I steer clear of any foods which can be classified as hard, round or sticky, this means that I avoided giving them foods like, whole grapes, raw vegetables, nuts, popcorn and chunks of meat or cheese. Instead, I would ideally prefer alternatives like pureed vegetables and fruit, blended mashed potatoes, or even small pieces of steamed vegetables. As for older children, the food still has to be cut into smaller and more manageable pieces.
Safe food handling also involves the following additional parameters:
- Ensure that cubed food is no more than half an inch in size
- Boil more challenging food pieces to the extent fingers can easily mash them
- Elongate grapes and cherry tomatoes to prevent choking
- Make sure that peanut butter is spread more thinly.
All of these measures have the approval of pediatricians to aid in the reduction of choking hazards.
References
Choking Abdominal thrusts Respiratory tractFrequently Asked Questions (FAQ)
Q: What are the signs of choking in a child?
A: The signs of choking in a child include difficulty breathing, inability to speak or cry, making high-pitched noises, turning blue around the lips, and grabbing at the throat. It's crucial to recognize these signs quickly to provide immediate assistance.Q: How can I save a child from choking?
A: To save a child from choking, follow these steps: 1) Give five sharp back blows between the shoulder blades with the heel of your hand. 2) If this doesn't work, give five abdominal thrusts (also known as the Heimlich maneuver). 3) Alternate between five back blows and five abdominal thrusts until the object comes out or the child becomes unconscious.Q: What is the correct way to perform abdominal thrusts on a choking child?
A: To perform abdominal thrusts, stand behind the child and wrap your arms around their waist. Make a fist with one hand and place it just above the child's navel. Grasp your fist with your other hand and give quick, upward thrusts into the abdomen. This action could push the object out and clear the airway.Q: What should I do if a baby is choking?
A: For a choking baby under one year old, the American Red Cross recommends: 1) Place the baby face down on your forearm, supporting their head. 2) Give five back blows between the shoulder blades. 3) If unsuccessful, turn the baby face up and give five chest thrusts. 4) Continue alternating between back blows and chest thrusts until the object comes out or the baby becomes unresponsive.Q: How can I prevent choking emergencies in children?
A: To prevent choking emergencies, cut food into small pieces, supervise mealtimes, avoid giving young children hard candies or nuts, keep small objects like marbles and balloons out of reach, and teach children to chew their food thoroughly. Always be aware of potential choking hazards in your child's environment.Q: What should I do if the choking child becomes unconscious?
A: If a choking child becomes unconscious, immediately start CPR. Call emergency services if you haven't already done so. Continue CPR until help arrives or the child begins breathing on their own. If you see the object in the child's mouth during CPR, carefully remove it, but don't perform blind finger sweeps, as this could push the object further into the airway.Q: Where can I learn more about first aid for choking and other emergencies?
A: You can learn more about first aid for choking and other emergencies by taking a course offered by organizations like the Red Cross or St John Ambulance. These courses provide hands-on training and up-to-date information on life-saving techniques for various situations, including choking emergencies in babies and young children.













 Login with Google
Login with Google Login with Facebook
Login with Facebook