
There’s an outbreak such a grievous event that immediate measures are to be taken to avert any further damage, and the case is even more severe if the child in question is an infant. Most frequently, food, small objects, or toys are the cause behind an interrupted respiratory tract, which is dangerous, to say the least, as it can impair breathing or, worse, suffocate. In this blog, we will strive to explain the ways one can quickly identify whether an infant is choking, the triggering causes for such instances, and if there are any first-aid tips to help with such reunions. More crucially, this article intends to provide step-by-step directions to parents and aiders of the infant, which would help them during high times and place them in a better position to act without panic or erratic movements. Approaches to avoid such situations are also offered as they provide an alternate method to ensure the baby remains safe.
What are the Signs a Baby is Choking?

Here are signs that require attention. If you see a baby choking, it can make breathing extremely difficult. A wheezing or a gasping sound is a good indication of this. It may even be that no breath control sound is produced. You may also check if the infant has a practical or involuntary cough, which in either case may not help as there is a finite chance of a baby being able to cough at all. An inability to cry is another answer alongside skin conditions whereby a minor bluish hue may occur around the lips or other skin areas. Frantic movements such as flinging arms are also available. Supplementary indicators involve callousness combined with rounded eyes, followed by the baby choking the neck or chest area with their hands. Appropriate first aid measures would be rendered impossible if such conditions go undetected.
How to Recognize the Signs a Baby is Choking
The baby is in danger of choking, and a few clues give me the warning signs. The first indication to look for is not being able to hear a cry, cough, or any such sound - an airway block. Secondly, I check for physical signs like cyanosis, where the lips start turning blue or the face color changes and is flabby. Other signs include nonsensical and ineffective coughing or panic attacks with wide open eyes and arms waving. All of these signs are the starting points and are enough to tell me that to save the person, first breathing must be restored, and the crack blocking the needed air to enter must be removed.
Why an Infant May Be Choking on Small Objects
Small pieces of a toy or any household item can be an object of analysis by a baby, who tends to put every piece of object in his mouth. Right from the sensory development stage, however, the act can be hazardous if the objects are small enough to obstruct the respiratory tract. In my findings, beads, coins, and even parts of toys are the significant reasons. As per the guidelines set by CPSC, if an object is 1.75 inches or 4.4 cm, it should meet safety standards, which would fall under the choking hazards category. These parameters assist in determining whether a toy or an object is appropriate for children aged 3 years or less. There are certain food items, too, like grapes, muscats, nuts, and pieces of meat, which can easily pose a choking threat, especially when given in more significant pieces than the child can chew. Close monitoring and being mindful of the abovementioned aspects should prevent such instances.
What to Do if the Infant Cannot Breathe or Cough
Immediate action is critical when an infant cannot breathe or cough due to a foreign object obstruction. Follow these steps:
- Assess the Situation
- Check if the infant is responsive or unresponsive. If unresponsive, call for emergency medical services immediately.
- Look for physical signs of choking, such as difficulty breathing, inability to cry, or bluish discoloration (cyanosis) of the skin.
- Back Blows
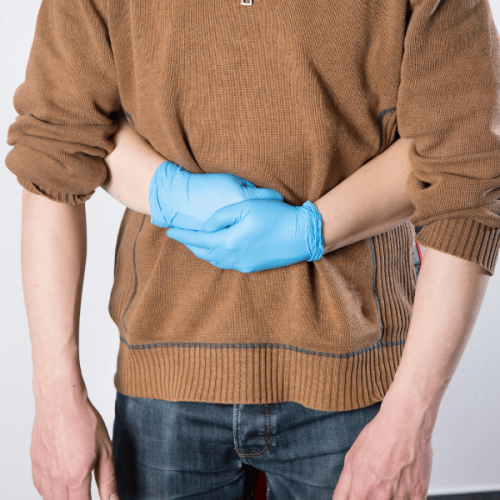
- Place the infant's face on your forearm, with the head supported and lower than the chest.
- Deliver five firm back blows between the shoulder blades using the heel of your hand.
- Chest Thrusts
- Turn the infant face up while supporting the head and neck.
- Position two fingers in the center of the chest, slightly below the nipple line.
- Deliver five quick chest thrusts, pressing approximately 1.5 inches (4 cm) to expel the object.
- Cycle Repeatedly if Necessary
- Continue alternating between 5 back blows and five chest thrusts while checking if the object has been dislodged.
- If the infant becomes unresponsive, initiate CPR and continue until help arrives or signs of breathing return.
- Never Perform Blind Finger Sweeps
- Do not attempt to remove the object by sweeping your finger inside the infant's mouth unless the object is visible. This could push the obstruction further into the airway.
Technical Notes on Force and Measurements
- Back blows should apply a controlled yet firm force, ensuring effectiveness without causing harm.
- Chest thrusts should press at an appropriate depth of 1.5 inches (4 cm) to accommodate the smaller thoracic cavity of infants under one year old. Avoid excessive force to prevent rib fractures.
Following these steps promptly and precisely can make a lifesaving difference in a choking emergency involving an infant. Always seek medical evaluation after the incident, even if the object is removed.
How to Perform Choking First Aid on an Infant

To address choking emergencies in infants, the following steps should be carried out methodically and with precision:
- Assess the Situation
- Observe signs such as difficulty breathing, weak crying, or an inability to cough forcefully to confirm that the infant is choking.
- Perform Back Blows
- Hold the infant face-down on your forearm, supporting their head and neck. Ensure the head is lower than the chest.
- Deliver five firm back blows between the infant’s shoulder blades using the heel of your hand.
- Perform Chest Thrusts
- Turn the infant face-up on your forearm, supporting the head with your hand. Maintain a lower head position than the chest.
- Using two fingers, press the infant’s breastbone just below the nipple line. Deliver five quick chest thrusts at a depth of 1.5 inches (4 cm).
- Repeat the Cycle
- Alternately, perform five back blows and five chest thrusts until the object is expelled or the infant becomes unresponsive.
- If the Infant Becomes Unresponsive
- Begin CPR immediately with chest compressions and rescue breaths while checking for the obstructing object. Remove it only if visible. Do not perform blind sweeps.
- Seek Medical Attention
- After removing the object, consult a healthcare professional to ensure no residual injury or harm has occurred.
These steps are designed to improve airway clearance while minimizing injury risk. Always stay calm and act with careful control.
Steps to Give Back Blows for a Choking Baby
If an infant is suffocating, to give emphatic back blows proceed as follows.
- Careful, Whenever A Baby Suffocates
- Put your left arm horizontally onto your level, helping the baby so its head is lower than the chest. Ensure that your forearm is placed over the leg to provide support.
2. Performing Back Blows
- Five medium-sized blows were delivered against the middle fleshy area with interlaced fingers using the fleshy part. More definitively, each stroke must be intentional to produce the needed force that moves the back of the infants.
- Recheck And Replace As The Situation Seems The Same
- After making five contact impacts, check if the material has been expelled; if not, this chest thrust together with the other previously sketched steps, such as the progression to the final step, keeping repeating until the airway passage is removed or in case the child falls unconscious.
4. Follow all these steps to ensure the child is not in danger and promotes good recovery.
- Seek medical attention when the child becomes unremitting about any condition, moves, or coughs. As contemplated by the commander, even the child suffocating is essential to keep in mind.
This discussion promotes good ideas about how to maintain the baby when it chokes and measures to be undertaken to prevent choking from occurring in the future.
How to Administer Chest Thrusts
- Correct the Position of the Baby
- Make the baby lie with its face up on a sturdy, flat surface or lay on your back with the infant. Maintain the head and neck. Allow the head to sit in a lower position than the rest of the body to benefit from gravity.
- Find The Right Position For Thrusts
- Utilize two fingers to the center of the baby's chest, which is the area under the nipples. Avoid the area just above the lower ribs to avoid injury.
3.It is now Time for the Chest Thrusts
- Insert your index and thumb into the towel's bottleneck without rolling it and twist three times. Roll it only three times and make five teats. Repeat until the entire area of the chest is covered. In such a case, repeat twice within the two-second interval. Each thrust should be distinct every time to create enough force so that the obstruction is evicted.
4. In Case of Need-Change, the Side of the Hand Used
- If your patient is still choking after five thrusts, swap head thumps with palm backward whacks of the thrusts. Repeat head thrusts with whacks until either the 2nd CPR cycle is completed or you level one head whack without more than one breath.
If there is still no resolution at the end of the cycle, always recommend emergency help. In addition, the baby should be monitored continuously and supervised on how he is doing well.
When to Use Abdominal Thrusts
Utilizo los golpes abdominales cuando una persona, en general mayor de un año, está atascada y no puede toser, hablar ni respirar como lo hace normalmente. Considero que este procedimiento es correcto solo cuando la obstrucción es muy importante y las tos no han funcionado. En el caso de mujeres embarazadas o infantes menores de un anho, uso otras técnicas en su lugar. En esta maniobra es importante to ensure the person is still awake or reasonably alert, and either standing or seated. If the person loses consciousness, I start CPR but do so while trying to gently locate and clear the obstruction.
What to Do if the Baby is Still Choking

If calling out for everything else becomes second nature and the infant still recurrently chokes, this is the ideal time to call for immediate medical help. While you’re waiting for assistance, ensure the infant is less than one and repeat the cycles of back blows and chest thrusts, giving forceful push each time. You can take tiny breaths intermittently and scan the mouth to see if there is obstruction; however, don’t perform sweeping motions or strokes as they can push the object deeper. Also, if the baby goes unconscious, start with CPR without waiting even a little and continue chest compressions and breaths, looking around to check if the object is in the respiratory tract during each exhalation, aiming for resuscitation. Finally, ensure you don’t lose sight of the big picture ,as relocating that occlusion is of utmost priority until the trained medical personnel arrives.
What to Do if the Infant Becomes Unresponsive
If the infant does not respond, take the following crucial actions:
1. Seek Emergency Help: First, make sure that emergency medical services (EMS) are called, either by yourself or someone else. If no one else is around, perform CPR for two minutes before you recite the emergency contact number ‘911’.
2 . Attempt CPR (Cardiopulmonary Resuscitation):
a.For compressions of the chest:
- Put two fingers in the middle of the chest, located just below the nipple line.
- Push the chest for about 1.5 inches (4 cm) inwards.
- The heart should be pumped 100 - 120 times a minute, but the rate of compressions should be allowed to relax the chest entirely at every repetition.
b.Delivering the Breath:
- After every set of thirty-two breaths, it should be done as a rescue breath.
- If you are using your palm and fingers to aid the child, gently place them on the neck while straightening them. Now, the mouth should be positioned so that it entirely covers the child’s mouth, and the nose should gently push the air inside for just a second—enough to make the child’s chest visible.
c.Please examine the child’s airway for obstruction:
- If you can see the object, use your fingers to clear the obstruction. But take care not to use a blind sweep.
d.Suggest Battling and Breathing:
- Repeat the process after every 30 compressions and two breaths cycle until you see the child's visible response or a professional walk into the room.
Utilizing these exact guidelines systematically and controlled improves the infant\'s chances of survival and recovery in this situation.
Steps to Take if the Infant is Coughing Forcefully
Should I witness an infant who has a cough and seems to be trying to clear some obstruction, I will let him cough since it is the body’s mechanism to shun out the object. While I do this, the infant will also be monitored very closely for any signs of increased form of distress – for instance, some degree of difficulty in breathing, bluish discoloration or cyanosis of the skin, or the child not making noises or cries which means that there has been a total obstruction of airways.
Parameters For Monitoring:
1. Effectiveness of Breathing:
- In an infant, I would like to see a normal rate of chest rise and fall of 30-60 breaths per minute.
2. Oxygenation Hampering:
- In this case, signs of oxygen deprivation can easily be noted, with the infant as lethargic or perhaps even cyanotic.
3 . Auditory Cues:
- Depending on how strong and productive a cough is would dictate if some assistance is needed.
If the infant is unable to complain of a sufficient cough or shows moderate signs of obstruction of the airway, I, for one, would consider back blows and chest thrusts as per the guidelines for infant choking.
When to Call 911 for Emergency Help
In case of these instances, never hesitate to contact 911.
Total airway obstruction:
An infant who is silent and does not breathe, cry, or cough suffers from a total blockage of the airway. This poses a significant risk to the infant's life, hence calling for immediate help.
Things that are to be noted:
- No attempt to breathe in leads to air or chest movement.
- Skin color changes to pale, bluish, or gray.
- Giddy status.
Poor respiratory movement:
When an infant breathes, stronger efforts are observed to inflate the lungs, and if that is unachievable, persistent breathing with assistance is observed.
Things that are to be noted:
- Respiratory rate is below 30 or more than 60 breaths within a minute.
- An infant becomes lethargic or insensible due to insufficient oxygen provided to the body.
Intervention measures taken are unsuccessful:
- Once the infant loses consciousness and resists all attempts of speaking or breathing, then aid must be given without further delay.
Post complications:
- If the airway is cleared with the required object still causing suffocation, persistent coughing, ultimate behavior, thin wheezing, or oxygen obstruction, immediate intervention becomes needed.
In infant choking emergencies, time is of the essence. For those without practical knowledge of basic first aid, obtaining emergency assistance is vital to facilitating immediate and effective professional assistance.
How First Aid Advice Can Help Save Lives

It is indeed a fact that First Aid instructions lay down the sequence of actions that can be done on the spot during an emergency, which increases the chances of a successful outcome. Ready and verbally directed caregivers will likely turn to techniques such as appropriate back blows and chest thrusts once they receive clear instructions. Also, indicators such as respiratory rate irregularities and apparent signs of tiredness tell us when a patient needing urgent attention should be referred to a hospital. Thus, by providing information concerning what should be done and the importance of doing these actions quickly, first aid instructions help to reduce risks and even save lives at crucial points.
Importance of First Aid Training for Parents
First aid training equips parents with the knowledge and skills necessary to respond effectively to various medical emergencies involving their children. It is particularly critical for addressing scenarios such as choking, severe allergic reactions, or injuries caused by falls. Parents trained in first aid can administer life-saving measures during the crucial moments before professional help arrives, reducing the risk of long-term harm.
Key Technical Parameters to Consider in First Aid Training for Parents:
- Recognition of Medical Emergencies
- Regular respiratory rate for children (20-30 breaths per minute for ages 1-5, 12-20 breaths per minute for ages six and older).
- Common symptoms of anaphylaxis include swelling, difficulty breathing, and hives.
- Essential Life Support (BLS) Skills
- Proper technique for infant (2 fingers) and child (1 hand) chest compressions.
- Compression depth of at least 1.5 inches for infants and 2 inches for children during CPR.
- Managing Choking
- Clear guidance on using back blows and chest thrusts for infants under one year and abdominal thrusts for older children.
- Ensuring that these actions are performed with appropriate force to avoid causing injury.
- Accident and Injury Response
- Proper wound cleaning and dressing methods to prevent infection.
- Immediate actions for suspected fractures, including immobilization techniques.
By mastering these parameters and engaging in hands-on practice, parents gain confidence in acting decisively in high-pressure situations, potentially saving their child’s life or preventing complications. First aid training should be considered an essential part of parenting preparation.
How St John Ambulance and Red Cross Training Offer Support
St John Ambulance and Red Cross are two of the most significant providers that offer comprehensive first aid training, which enables a person to save a life. Some of the courses offered include CPR for infants and children, choking management, and CPR for beating injuries. Participators of these programs are shot-tailored courses that assist them in acquiring skills such as chest compressions, compression bandaging, and using splints through practical sessions. These two organizations also have a lot of resources, among them handouts, video tutorials, and lesson plans. After participating in these programs, I feel prepared to deal with urgent situations and care for my child.
Benefits of Using a First Aid App
First aid apps allow instant, portable, and adequate instructions in emergency situations over communication. The apps provide stepwise guidance to the user through the handling of cuts, burns, bleeding, choking, cardiac arrest, and more. Some apps have an offline mode that allows the user to retain essential information even when Wi-Fi is unavailable, which is especially useful in rural locations or emergencies when the connection is limited.
First aid apps are often austere in their designs since they have graphics, videos, and audio that can enhance comprehension in tense situations. Apps such as those created by the Red Cross and CEC contain features enabling users to access the app and automatically dial an emergency number or track the user’s location.
- Functional Without Internet: Provides access to vital data while offline.
- Gamified App Elements: Incorporates quizzes, tutorials, and other material to enhance comprehension.
- Geolocation and Emergency Contact Integration: Assists in adding direct dialing capability for emergency service and locating users.
- Updated regularly: The most recent recommendations, such as AHA or others, can be accessed instantly.
- Multi-Device Support: The apps are built for both iOS and Android devices, which makes them easier to use.
First aid apps reduce the workload as they augment an individual’s or a caregiver’s readiness to deal with any possible medical situation that they might encounter. Such applications function as an extension of formal first aid courses, and they are important for people willing to respond to emergencies.
What Should You Do Until Help Arrives?

- Appraise the Circumstances for Dangers: Make sure that the area in which both the first aider and the injured person are situated is out of harm's way. Only move the injured person if there are clear circumstantial threats that are urgent, such as fire or walls collapsing.
- Verify Awareness: Check whether the individual is waking and can inhale oxygen. In case the person does not respond to any of the questions being asked, start measures like CPR to revive the person if trained for such scenarios.
- Manage Bleeding: In all cases where bleeding occurs, the first aid person should use their hands or a clean cloth/bandage to apply direct pressure on the wound, which is a priority for bleeding control—also, complete the use of sterile gloves, which aids and minimizes infection risks.
- Comfort and Supervise: The injured person should receive continued assistance, such as keeping them calm, providing warmth, and getting them into comfortable positions. Their condition, such as breathing rate and heartbeat, should be monitored until a specialist arrives at the scene.
- Basic Agreement Features: If you contact an emergency service provider, heed their instructions carefully and follow the order of action provided. Moreover, ensure that you also explain the condition of the injured individual to them and provide any help you can.
So, in a way, you serve a critical function, maybe easing the situation for the worst cases until a higher source of medical care is made available. Following these procedures can ensure the situation does not worsen drastically.
How to Keep the Infant's Airway Clear
- Ensure Proper Positioning: Lay the infant on their back on a firm, flat surface such as a table or the floor. Slightly tilt their head back to open the airway, but avoid overextending the neck, as this could obstruct the airway instead. For newborns, a neutral head position is sufficient.
- Clear Visible Obstructions: Check the infant's mouth for any visible blockage, such as mucus or food. If you see an obstruction, gently remove it using your finger, but do not blindly sweep the mouth, as this could push the object further into the airway.
- Use Bulb Syringe for Fluids: If fluid (e.g., saliva or mucus) is blocking the airway, use a bulb syringe to suction the mouth and nose gently. Squeeze the bulb before insertion, place the tip into the side of the mouth or nostril (not too deep), and release the bulb to suction the obstruction.
- Perform Back Blows and Chest Thrusts for Choking:
- Position the infant face-down on your forearm, supporting their head and neck, with the head lower than the chest.
- Deliver five firm back blows between the shoulder blades using the heel of your hand.
- Turn the infant over onto their back, keeping the head lower than the chest, and administer five chest thrusts by pressing with two fingers on the breastbone, just below the nipple line. Compress to a depth of about 1.5 inches (4 cm), allowing full recoil between thrusts.
- Seek Immediate Medical Assistance: Call emergency services immediately if the airway does not clear or the infant becomes unresponsive. Begin CPR if trained and continue until professional help arrives.
By following these precise steps and parameters, you can effectively assist in keeping an infant's airway clear and potentially save a life. Proper training in these techniques is highly recommended for caregivers and first responders.
What to Do if You Can See the Object Causing Blockage
If the obstruction was caused by a visible object that I can remove without forcing it deeper into the airway, I can do so cautiously. However, if the object is reachable, I would use my pinky finger, such as the infant's mouth, if necessary. I would ensure that no force is used or blind visits are made, as that can complicate the airway blockage. In the case the object is not coming out, or the choking does not subside, I will promptly contact a doctor.
How to Comfort the Infant Under 1 Year Until Help Arrives
In the first instance, while trying to attend to an infant of 1 year and below, I would try to ensure an environment that is quiet and free of sudden movements. Maintaining a gentle and calm voice while securely holding the infant is also critical, as this can bring about comfort; implementing skin-to-skin touch can also be great in such situations. If the infant is crying, I would look for the most likely reasons, such as hunger, temperature, and any discomfort, such as a wet diaper, and try to resolve such issues. To further soothe an infant, I may gently rock or sway the baby while looking at the infant’s eye. If applicable, I would wrap the infant tight enough for flexible hip movements but loose enough around the chest so that it does not feel suffocated. Also, I would closely monitor the infant's signs, such as labored breathing or discolored skin, and monitor his safety while we wait for an expert to assist.
References
Choking First aid CoughFrequently Asked Questions (FAQ)
Q: What are the first steps if an infant is choking?
A: If an infant is choking and unable to cry or make a sound, immediately call for emergency help. Begin by supporting the infant's head and neck and holding the infant's chest in your hand. Position the baby face down along your forearm, ensuring the infant's head is lower than its body.Q: How do I perform back blows on a choking infant?
A: To perform back blows, use the heel of your hand to give up to 5 quick, sharp back blows between the infant's shoulder blades. This can help dislodge any obstruction in the airway.Q: What should I do if back blows do not clear the airway?
A: If back blows do not clear the airway, turn the baby face up while supporting the infant's head and neck. Position the infant's head lower than their chest, and place two fingers in the center of the infant's chest in your hand, just below the nipple line, to give up to 5 chest thrusts.Q: When should I start baby CPR if an infant is choking?
A: If the infant becomes unconscious and is not breathing, start baby CPR immediately. Call emergency services and perform CPR, which includes chest compressions and rescue breaths, until help arrives.Q: Is the Heimlich maneuver recommended for infants?
A: The Heimlich maneuver is not recommended for infants under one year old. Instead, use back blows and chest thrusts to clear the airway.Q: How can I ensure I’m performing choking first aid correctly?
A: A training course, such as those offered by the American Red Cross, can provide hands-on experience and confidence in performing choking first aid for babies and children.Q: What should I avoid doing if my child is choking?
A: Do not try to remove the obstruction with your fingers unless you can see a piece of food or object in the infant's mouth. Blind finger sweeps can push the obstruction further down.Q: What signs indicate that an infant is choking?
A: Signs that a baby is choking include being unable to cry or make noise, weak or ineffective coughing, difficulty breathing, or turning blue around the lips.Q: Can choking occur even if the baby makes a strong cry?
A: If the baby is making a strong cry or coughing forcefully, it means the airway is only partially blocked. Encourage coughing, as it may help clear the airway without intervention.Q: Why is knowing choking first aid for infants and toddlers is important?
A: Knowing how to perform these steps can be crucial in emergency situations. They can help dislodge obstructions and potentially save a child's life before professional help arrives.






 Login with Google
Login with Google Login with Facebook
Login with Facebook