Omitting the required intervention in case of the inability to mouth or speak might lead to qualitative consequences, which in this case are death or mortality, especially for infants. Children aged less than 1 year are in prime developmental age with physiological structure maturing, which includes coordination control of swallowing and lungs, having small size gaps for windpipes. Today’s blog narrates the basic first aid steps required during the choking of an infant, which includes targeted action to achieve higher success rates. Knowing how and why infants choke should encourage a parent or a caregiver to react appropriately in a given situation, which increases the survival rates of the infant in such dire pressures. This will offer clear guidelines on the basic infant choking first aid principles and how back blows and chest compression methods can be used in sequential order so that the caregivers take the right action at the right time.
What should you do if a choking infant cannot breathe?
How to perform back blows correctly.
It is my view that back blows to a choking infant need to be done according to the guidelines set forth. To do this, an infant is placed on an adult’s forearm with the infant’s head just under the forearm level. With one hand supervised over the infant’s head and neck, five blows are delivered with the other hand high up on the middle of the infant’s back between the two shoulders using a heel of the palm with moderate and controlled pressure; since children are relatively fragile sensitive force needs to be applied. This should be repeated as long as the infant can be seen to be making some noises while breathing or crying, thus indicating the blockage has been cleared. It is worth keeping in mind that there are a considerably significant number of different cases that allow children to breathe independently, which makes it easier for you to perform your part of the work. In such situations, it is crucial to remember that being calm and accurate is the most appropriate behavior for a given stressful situation.Steps for chest thrusts in infants
In my extensive experience and practice of several years in pediatric emergency medicine, it is evident to me that performing chest thrusts clearly assists in the removal of an infant from a choking scenario, only if it is performed as it is supposed to be. This is how it should be done: Let us go on.- Position the infant appropriately: You massage the infant’s head and keep it placed lower than the infant’s torso and recognize the ‘supine’ position as ‘the safe position.’ Note that their airway is not obstructed during this entire process.
- Identify the correct location: Just under the nip as part of the ribs above the navel, note two to three specific fingers as an important feature. This is the location where chest thrusts will be administered to that infant.
- Apply firm, controlled thrusts: Position your fingers and thumbs in between the lower and upper ribs and use them to push halfway down the ridges that the two ribs make. Because all efforts are controlled, great thought should be given as to how much force the thrusts should generate as the goal is to clear the obstruction without harming the patient so making enough force to attempt clearing the air is easy.
- Repeat the sequence: Insert 5 successive thrusts that ramp in magnitude over a 5-minute span to the affected rib area then after five thrusts give an ear to an infant’s indication or sign which could involve crying or only a little thoracic cough which could suggest the obstruction is displaced out of the airway and, hence, breathing has been restored.
- Continue until resolved: If swallowing is difficult due to the body’s size-increasing obstruction, it would be prudent to perform chest thrusts in conjunction with back blows until proper medical assistance arrives or remove the obstruction if it disappears on its own.
Signs that the airway is clear
It is my view who has experience that avocational or toxicological management is not necessary to observe whether an infant's airway is free following back blows or chest thrusts. These are the signs that are of utmost concern:- Ability to Cry or Make Noise: It can be construed that air is able to pass through the sound producing organ which was previously and somewhat still remains congested, if a child is able to make sounds or cry within the first twelve months.
- Normal Breathing Patterns: It can be construed that air is able to pass through the sound producing organ which was previously and somewhat still remains congested, if a child is able to make sounds or cry within the first twelve months.
- Coughing:If an individual is exhibiting a strong cough reflex, then it implies that some covering is loose and that the flush and clean mechanism, which serves to remove any obstruction, is functioning well.
- Improved Color: Improvement of the child’s hypoxic baseline skin color can be noted, especially the facial blanch, which was witnessed during the clutching when there was a nasogastric tube blockage.
- Calm and Resting: A normal face sometimes implies no pain, meaning that when the infant is calm, he is also breathing normally, suggesting that he is not active, thus interfering with the never-ending running system.
Steps for chest thrusts in infants
From my experiences of years in practicing and teaching pediatric emergency medicine, it stands to reason that performing chest thrusts must obviously assist in the removal of the infant from a choking scenario and it has to be done correctly. Here is how to proceed:- Position the infant appropriately: First, place the infant on your leg in a supine position with its head lower than its torso relative to the chest and hold its head with one hand in such a way that the airway is not obstructed.
- Identify the correct location: Find the nipple line and touch the lower ribs just below the nipple with two or three fingers; this will be the location where you will perform chest thrusts.
- Apply firm, controlled thrusts: Apply pressure with your index fingers down two thrusts of about 1.5 inches. It is located in between the downer ribs and upper ribs. The only important factor is that the thrusts are adequately firm, controlled enough, and to the extent that the aim of pushing the obstruction out of the airway is achieved but are not sufficiently strong enough to cause a physical injury.
- Repeat the sequence: Forcefully push them back into the ribs and give the affected rib cage 5 thrusts enduring a minute interval after every five then after five thrusts listen for the infant’s sign which more likely include a cry, cough, or both, that indicates that the obstruction has been removed from their airway.
- Continue until resolved: If a person is unable to eject the size increasing obstruction, then it is safer to combine chest thrusts and back blows until medical assistance arrives or otherwise look for and remove the obstructing object if it is easier to do so.
Signs that the airway is clear
A knowledgeable practitioner such as myself has to argue against the need to use avocational or toxicological management in order to determine the signs indicating the patency of an infant's airway post-back slaps or chest thrusts. Instead, look for these reassuring signs during the examination to rule out neck or throat obstruction in the infant:- Ability to Cry or Make Noise: There’s Congestion - Due to compression of the vocal organ, cry or sound is regarded as the first-year age milestone, which indicates the capability of the air to pass through the
sound speechorgan, in any case, disintegration of the organ structure has not occurred to some extent. - Normal Breathing Patterns: Possibility of Obstruction in the Airway - If a baby looks like he is trying to breathe without any conflict or struggling, wheezing, or gasping, then there are fair chances that the airway is actually patent.
- Coughing: A voluntary cough shows some form of looseness and indicates that some covering may still be present while the cleansing system remains effective and in action.
- Improved Color: Try not to choke an infant. The intended color of the skin is the baseline color of the infant’s improvement, especially the glance of the face blush, which was seen during choking because of the gasper.
- Calm and Resting: Child Potential - There is no evidence of pain or any form of disorder in a child; in such a circumstance, there is a re-establishment of the connection with the breathing and fighting apparatus. Infants possess facial elements that are ensured by calm day-to-day nerves.
How to Administer First Aid for a Choking Baby
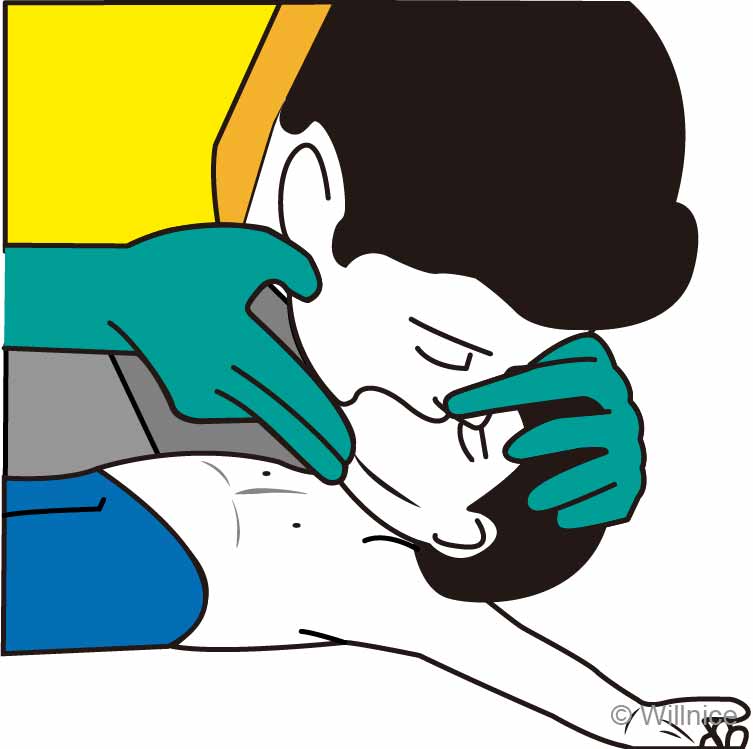
 For someone who has experience in this area has observed, offering first aid support to a baby in contraction can be quite critical and tough especially for new parents or their guardians, hence I would like to state some first aid steps as first aid support. First, it important to establish whether the infant indeed needs help, in this case, a baby is not able to breathe nor cough so it is vital to understand this before giving any assistance. If the baby finds himself in such a case then start by giving strong intersects between their shoulder blades, otherwise stimulate the chest like this. To begin with, they are placed face down so that their body or stomach is directed to the vantage bar, but first, maintain a standing position that ensures both their head and torso are parallel. Encourage the voluntary coughing reflex by doing the following: 5 powerful pushes (using the heel of your hand) are given. After five pushes, flip the baby over and push/bear down two fingers on the breastbones five times, doing the same. Continue the sequence until the baby is able to cry or breathe on their own, performing harmoniously strong taps on their back and breast bones. If the baby loses full consciousness, this is the right time that CPR should be initiated, along with calling for a doctor’s help at once.
Involvement in such emergencies needs training in these techniques, as it is more sensible than waiting to be ready when required.
For someone who has experience in this area has observed, offering first aid support to a baby in contraction can be quite critical and tough especially for new parents or their guardians, hence I would like to state some first aid steps as first aid support. First, it important to establish whether the infant indeed needs help, in this case, a baby is not able to breathe nor cough so it is vital to understand this before giving any assistance. If the baby finds himself in such a case then start by giving strong intersects between their shoulder blades, otherwise stimulate the chest like this. To begin with, they are placed face down so that their body or stomach is directed to the vantage bar, but first, maintain a standing position that ensures both their head and torso are parallel. Encourage the voluntary coughing reflex by doing the following: 5 powerful pushes (using the heel of your hand) are given. After five pushes, flip the baby over and push/bear down two fingers on the breastbones five times, doing the same. Continue the sequence until the baby is able to cry or breathe on their own, performing harmoniously strong taps on their back and breast bones. If the baby loses full consciousness, this is the right time that CPR should be initiated, along with calling for a doctor’s help at once.
Involvement in such emergencies needs training in these techniques, as it is more sensible than waiting to be ready when required.
Positioning the Infant Under 1 Year for First Aid
I am pretty sure that correctly positioning an infant below one year for first aid is among the skills that improve the effectiveness of the intervention. The infant is positioned in the prone position and placed on the forearm, with the head lower than the chest. The hand must support the infant by grasping the chin so that the body faces the thighs. Such hand position is important in avoiding obstruction over the airway and in stabilizing the back of the head for delivery of back blows. Properly positioning the infant in this safe manner ensures that back blows can be delivered while minimizing the likelihood of inflicting more injuries, which promotes the quest for accomplishing the first aid measures seamlessly and safely. Furthermore, training in such situations is also important in building assurance and being able to perform these movements effectively.Using the Heel of Your Hand for Effective Back Blows
I am well aware of how challenging it can be for some people to perform effective back blows on an infant, but if the process is made into clear steps, then it can be quite simple. In that case, here’s the correct use of the palm heel:- Positioning: The infant should be placed face down on the forearm which is in turn rotated such that the chest is higher than the head. Insert a finger under the baby’s jaw without the mouth meaning the mouth can breathe.
- Hand Placement: The mid-section area of the wrist, which is about an inch away from the wrist joint, is used to deliver back blows. This is the firm area. This part delivers a solid rock with such an impact that the object can be easily taken off.
- Blow Delivery: While delivering five back blows to the eight-between the shoulder blades babies back dont be using excessive force as it can create more harm. Remember all these actions like movements and blows you are about to deliver as in a b direction this will help.
- Observation: Each time the impact is delivered, check whether the patient is still able to breath and whether he/she is conscious as this way you are well unaware of the problem that has occurred and you are able to assist in future problems that occur.
- Alternation: After delivering five backshots and seeing no cut-try-out chest force. The throat must be cleared, so continue hitting the between the shoulder blades until the fingertip comes out of the kid's mouth.
When to Call Emergency Medical Services
in an infant choking episode, when an infant might require to be given assistance to the extent of an emergency being called, it is important to know from a patient’s point of view. So, here are the circumstances where one might want to make a call for help:- Loss of Consciousness: In case there is loss of consciousness in the infant, it is essential to call for EMS without any delay. Loss of consciousness signifies lack of oxygen due to obstruction and this requires urgent medical care.
- Ineffective First Aid Procedure: If five back blows and five chest thrusts have been ineffective in removing the obstruction and the baby is not able to breathe or cry properly, that itself is a reason to call emergency services.
- Blue Lips or Pale Skin: These are clinical signs that the infant is not getting sufficient oxygen. If these signs are seen with difficulty in breathing then EMS must be called instantly.
- Breathing Difficulties Persist: Should the infant begin to breathe but in a labored or irregular fashion, or if such symptoms reoccur, it is reasonable to request medical assistance in order to confirm that their airways are unobstructed.
- Parental Instincts: Use your own judgment. In case, at any stage, the parents are able to see that the infant is in discomfort, which appears to be beyond the control of the parents, or the condition is deteriorating, it is advisable to call for emergency services.
Why is CPR important for a choking baby?
 Based on my experience,baby cannot be overemphasized, as this is perhaps the only emergency technique available to use when other methods have failed. Through CPR, perfusion of well-oxygenated blood to vital structures, especially the frame of the brain, is preserved, giving a chance to the body while an ambulatory service is on its course. CPR is learned as a systemic approach that consists of doing heart massage and sending a set number of breaths into the mouth of the parturient female whenever there is a suspension of the infant’s heart beat or breathing until the airway is vegetated or until there is satisfactory medical help, in such a delicate and critical situation where every second counts, this technique could potentially be the first step to sustaining life.
Based on my experience,baby cannot be overemphasized, as this is perhaps the only emergency technique available to use when other methods have failed. Through CPR, perfusion of well-oxygenated blood to vital structures, especially the frame of the brain, is preserved, giving a chance to the body while an ambulatory service is on its course. CPR is learned as a systemic approach that consists of doing heart massage and sending a set number of breaths into the mouth of the parturient female whenever there is a suspension of the infant’s heart beat or breathing until the airway is vegetated or until there is satisfactory medical help, in such a delicate and critical situation where every second counts, this technique could potentially be the first step to sustaining life.
When to Start Infant CPR
- Unconsciousness: In case of an emergency where the infant doesn’t respond and is not breathing, one shall praise the unconscious infant by gently tapping on its shoulder. This assessment shall determine the pulse of the infant.
- No Breathing or Agonal Breaths: The moment such a situation becomes unbearable in which the infant cannot either breathe or is just gasping, CPR has to be administered straight away. Gasps are irregular and denote that the heart has stopped beating.
- Choking Incident with Unarousable Infant: In a scenario where an infant chokes and then after back blows and chest thrusts the infant becomes unconscious, consuming its breath, the air in the windpipe needs to be removed by pressing it and blowing air in a fast manner. The above-mentioned actions are referred to as CPR.
- No Pulse Detected (rare for laypeople): Not many people are able to find a pulse in an infant; only a few are capable of doing such a thing and that too with practice. As per the general guiding rule, not more than 10 seconds shall be spent feeling for a pulse, otherwise, it would no longer be of any use, performing CPR is recommended.
- Parent or Caregiver Instincts: As a parent or caregiver, one knows how to respond, so it would be advisable to follow gut instincts on the matter. Such a go-to approach would be ideal whenever an infant seems to be in a dire situation, so while waiting for and calling for assistance, it is recommended that CPR be started.
Correct Technique for Chest Compressions
Given the level of experience possessed with this particular area, this is how infant chest compressions can be done:- Positioning: An infant should be placed on a firm, flat surface like a table, on the ground, or on their back.
- Two-Finger Method: Two fingers (an index finger and a middle finger) should be positioned just below an imaginary line connecting the infant’s nipple and the center of the chest. This provides a precise point of contact over the infant’s lower sternum. Fingers should be perpendicular to the subject's chest so that adequate force is applied without slippage of the fingers.
- Compression Depth and Rate: Compressions of about one point five inches (4 cm) should be targeted. A rate of 100 to 120 Compressions within a single minute is adequate. The depth and rate at which the compressions are done are critical because this allows blood circulation by mimicking the heart's natural pumping action.
- Release and Allow Full Recoil: Special and precise lifting off of the sternum ought to be avoided so as to allow the chest after every compression to entirely return to its original position. The sequence of contraction and relaxation throughout the entire process should remain the same. Full recoil of the chest is necessary for the heart since it allows the chambers of the heart to be filled back with blood between the contractions.
- Rhythm and Consistency: There should be adequate timing between the compression and the timing, and further, a smaller period of time should be utilized during the gap between the compressions, and perfect pumping should be maintained. Stability in the technique also provides greater efficacy by allowing proper perfusion of major organs with blood.
How Long to Continue CPR Before Seeking Additional Help
it is important to bear in mind that a CPA should be performed until one of the events listed below occurs: the caregiver is too weak to continue; the infant breathes or moves so that you take over CPR; a defibrillator becomes available and is, CPR is of paramount importance as it ensures that vital organs such as the brain receive adequate oxygenated blood to enable them to survive until the trained group with life supporting advanced apparatus come to the victim's aid.How can Red Cross training help in choking emergencies?
 I can assert with confidence, that Red Cross training allows a person to gain the necessary skills and confidence to take control of a situation where a person’s airway has been obstructed. The training includes valuable information regarding the recognition of signs of choking, the correct means of performing back blows age sufficiently, thrusting, and CPR on infants and children. This training gives the assurance that the necessary rendering of help can be done deftly and in a coordinated manner during the emergency, ensuring that maximum airway obstruction and blood flow are maintained and the chances of the two surviving are good. What is more, Red Cross training addresses assessment of varied situations where care for children is provided, placing caregivers in a position to easily move from providing first aid to full medical treatment when needed.
I can assert with confidence, that Red Cross training allows a person to gain the necessary skills and confidence to take control of a situation where a person’s airway has been obstructed. The training includes valuable information regarding the recognition of signs of choking, the correct means of performing back blows age sufficiently, thrusting, and CPR on infants and children. This training gives the assurance that the necessary rendering of help can be done deftly and in a coordinated manner during the emergency, ensuring that maximum airway obstruction and blood flow are maintained and the chances of the two surviving are good. What is more, Red Cross training addresses assessment of varied situations where care for children is provided, placing caregivers in a position to easily move from providing first aid to full medical treatment when needed.
Benefits of Taking a First Aid Course
There’s a lot more to first aid training than just being able to save someone’s life – taking the first aid course has its benefits, and I can tell you, as an industry expert, that there are numerous of them. A case in point: Let me break them down for you:- Empowerment and Confidence: First and foremost, a first aid course provides you with a new sense of power and self-belief to deal with different unexpected occurrences. A proper course of action would then definitely cut down the panic and the second guessing that is usually common on such or similar scenarios.
- Quick Response Time: One of the primary benefits is the ability to respond quickly and correctly during an emergency. A trained person will be able to make critical decisions and do life-saving tasks within crucial minutes, thus providing immediate attention that can go a long way in improving the situation.
- Understanding Life-Saving Techniques: The major sub-instructors of the course would include the CPR and AED and the un-witnessed choking. In such cases the likelihoods of blood and air passages to remain intact increases greatly thus increasing the chances of survival significantly.
- Expanded Awareness of Health and Safety Risks: Identifying and locating of possible dangers is vital. This not only helps in attending to the emergencies but also in averting the emergencies all together.
- Legal and Workplace Requirements: It is imperative to attend first aid training as they are normally imposed to. practically all occupations with health and safety considerations. This gives viability of employers being able to tackle dire occurrences.
- Personal Development: Improving your competencies via first aid training increases not only your capabilities but also your importance in that particular society and workplace. It promotes a safety and prevention culture.
Understanding the American Red Cross Guidelines
The guidelines of the American Red Cross are detailed with the aim of ensuring that persons are well-equipped to tackle emergencies with proficiency. As an industry expert, I’ll outline these guidelines in an easy-to-understand manner:- Assess the Situation: The first step is conducting the risk assessment of the environment so that the rescuer and the sufferer will not face the threat. Determining the risks and taking appropriate measures is a very important step in every process. For instance, if an individual loses consciousness near an active electrical wire, it is better to ascertain the threat is eliminated before attempting any kind of rescue.
- Call for Help: In all emergency situations, getting in touch with the pertinent authorities phone contact immediately contact them. It is very useful to speak directly with those who are skilled in the field, since this enables first aid and instructions to be administered whilst on the way to the place.
- Care for Life-Threatening Conditions First: Once a person has suffered injury or an illness, an attempt should be made to identify the most threatening parts first. For example, an artery which has been damaged and caused severe bleeding or in breathing obstruction cases. For the external bleeding, place pressure on the tissue around the wound, and remove foods from the mouth and provide blows to the back.
- CPR and First Aid: Basic life support steps such as CPR ( Cardiopulmonary Resuscitation ) and First Aid must be followed. The Guidelines that the Red Cross has in place are aimed at proper practice, such as depth and rate of the compressions to the chest and the time taken to do it in order to ensure sufficient blood circulation and, hence, maintain breathing. This includes AEDs (Automatic External Defibrillators) if it is available on-site.
- Monitor the Victim: Be on alert for any signs of response or breathing in the patient. If the situation changes, adjust accordingly: for instance, if the victim does not respond, initiate the procedure for performing CPR or if they begin to show signs of life.
- Stay Informed and Trained: Make a point to have periodic training for first aid and CPR in light of the fact that protocols may change depending on new research and innovations. Such practice ensures that you do not go out of touch with the most efficient skills.
Using a First Aid App for Quick Reference
I can say with absolute certainty that in some situations, a first aid app can prove to be invaluable. Here's how:- Instant Access to Information: One of the most remarkable advantages is that reliable sources are available at the click of a button. Such applications offer a comprehensive guide on how to perform first aid techniques such as CPR, how to care for a wound, and how to relieve someone suffering form choking. Availability of such a manual enables the user to recover from an emergency situation in a more timely and efficient manner.
- Interactive Features: Numerous first aid applications, including but not limited to CPR assist, sprint fx, first aid by Red Cross, et cetera, and videos and animations interactive examples help demonstrate more difficult tasks. Picture resources are important in learning a new skill or motion where time constraints to perform the motion quickly come into play.
- Regular Updates: First aid apps can always be easily improved and enhanced. This allows you to have easy access to the most advanced techniques and principles.
- Readiness Anytime, Anywhere: One is able to carry first aid knowledge, which is crucial in any situation mobile applications provide for such purposes. Disposable CPR masks, gloves, or gauze can take the formof mobile devices at work, home, or while traveling.
- Emergency Contacts: Many applications have options for emergency contacts integration, and some even provide the possibility to call emergency services directly from the app itself. In this manner, this feature guarantees that people can get in touch with aid as soon as an emergency situation begins to develop.
- Personalization: Some apps let users offer personalized advice through the use of specific situations. To illustrate, they might specify the case of having an attack of asthma or allergy. Making information specific to your personal needs can enhance the value of the information as well as making the time of your response shorter.
What are common choking hazards for infants?
 In the case of foods or objects that are choking hazards for children, it is essential to appreciate the fact that children have very small airways. It can even be said that even small objects like beads, coins, or buttons can be dangerous, and so can toys with detachable parts. Beyond these items, some common foods are themselves danger zones, like grapes, hot dogs, nuts, popcorn, raw veggies, etc; these are best cut into the tiniest bits or omitted entirely. Personally, in my brain, all meal and play times for infants should be properly supervised since everything can be a target for the mouth-discovering nature of the infant. As a rule, parents should be alert and avoid distractions when inspecting the child, and the child’s environment and surroundings should be free from the risk of danger.
In the case of foods or objects that are choking hazards for children, it is essential to appreciate the fact that children have very small airways. It can even be said that even small objects like beads, coins, or buttons can be dangerous, and so can toys with detachable parts. Beyond these items, some common foods are themselves danger zones, like grapes, hot dogs, nuts, popcorn, raw veggies, etc; these are best cut into the tiniest bits or omitted entirely. Personally, in my brain, all meal and play times for infants should be properly supervised since everything can be a target for the mouth-discovering nature of the infant. As a rule, parents should be alert and avoid distractions when inspecting the child, and the child’s environment and surroundings should be free from the risk of danger.
Identifying Small Objects That Can Cause Choking
Involved in this field, I would indicate first of all what small objects pose the anger of choking to infants and the relevant parameters to take into account:- Size and Shape: In the case of choking, it should be noted that any object small enough to pass through an infant’s trachea can block the airway. This factor usually applies to any component which passes the small-parts tester measuring 1.25 inches in diameter. Highly rounded objects such as marbles and balls, are particularly hazardous due to their shape.
- Material Composition: Materials made of plastics, glass, or metals are hard and thus prone to cause choking as they cannot be masticated. Such materials should not be accessible by infants.
- Detachable Parts: Toys or things that are made of small and detachable objects such as buttons on stuffed toys, building block pieces and many others have a tendency to be swallowed. Inspect toys for any signs of damage that could result in loss of fragments.
- Foods: Some foods are regarded as high-risk of choking especially for infants. This includes choking risk objects such as grapes, nuts, popcorns, and candies. Such foods should be cut into smaller pieces, crushed or totally avoided in the case of infants.
- Accessibility: Always take into account the layout of the environment as well as the ability of an infant to grab small objects. All hazards should either be out of reach or safely locked in place.
Preventive Measures to Avoid a Choking Emergency
I am able to give you practical suggestions that are relevant to the occurrence of choking emergencies. First and foremost, always make sure that the space does not have small objects which can cause harm. Always check the floor and other surfaces that can be reached for such objects as coins, buttons, or small toys that could be swallowed easily. In terms of food, do not forget to cut the food into small pieces for easier chewing or swallowing, especially those known to be choking hazards like grapes, nuts, and hot dog sausages. An adult should always be able to watch infants when they are eating as well as during play activities. Also, follow the safe toy guidelines in particular the age suitability of the toys used by infants. By being more alert and being able to act accordingly in these regards, we can create a safer environment for babies and minimize choking emergencies significantly.How to Educate Caregivers About Choking Risks
My aim is to ensure that caregivers are aware of the choking risks and how to manage these risks efficiently. Caregivers should be educated in this essential area of nursing as follows:- Awareness of Common Hazards: Start with examples of objects or foods that pose a choking hazard, e.g., round small toys, button batteries, grapes, and nuts. Explain how these items are a choking hazard in regard to their shape or size relative to an infant's airway.
- Safe Environment Practices: Instruct caregivers on the need to clean the area in which infants routinely eat and play, and tips on organizing it. Stress the need to check for small objects on the floor or within reach on a regular basis, and how such simple tips can help avoid dangerous situations.
- Food Preparation Techniques: Provide practical tips on how to prepare and serve food that is unlikely to cause choking. This may comprise mashing certain foods like fruits, cutting other foods into very small pieces, and omitting certain types of foods altogether. Carrying out demonstrations may also be very useful.
- Proper Supervision: Point out the importance of constant, uninterrupted supervision during mealtimes or play. Describe how fast accidents happen, but that they can be prevented through constant supervision.
- Emergency Response Preparedness: Teach caregivers how to perform basic back blows and chest thrusts while holding infants, as well as other routine first aid procedures. Recommend that caregivers enroll in first aid courses to increase their confidence when faced with emergencies.
- Use of Age-Appropriate Toys: Emphasize the importance of choosing toys suitable for the child’s age. Indicate how to assess the potential risks, for instance, the risk of small parts coming loose.
- Frequent Engagement and Learning: Recommend that the families routinely check and assess any new information related to child safety. Caregivers are also in continuous education through different programs or the internet which provides contemporary standard procedures about children.
Reference
- MedlinePlus: Choking first aid - infant under 1 year
- American Red Cross: Infant Choking - How To Help
- Raising Children: Choking first aid for babies under 12 months
Frequently Asked Questions (FAQs)
Q: What is the first aid advice for a baby who is choking?
A: If a baby is choking, lay the infant face down along your forearm, supporting the infant's head and neck. Give five back blows between the infant's shoulder blades using the heel of your hand. If the obstruction persists, turn the infant over and give five chest thrusts by holding the infant's chest in your hand and pressing forcefully but gently on the lower half of the infant's breastbone.Q: Can you use the Heimlich maneuver on a baby who is choking?
A: The Heimlich maneuver is not recommended for infants under one year. Instead, use back blows and chest thrusts as the appropriate method for first aid for choking in infants.Q: What should I do if the baby becomes unresponsive while choking?
A: If the baby becomes unresponsive, call your local emergency number immediately. Begin infant CPR with basic life support techniques, including giving 30 chest compressions followed by two rescue breaths. Continue until professional help arrives or the infant becomes responsive.Q: Is it normal for an infant to cough forcefully when choking?
A: Yes, if the infant is coughing forcefully, it indicates that they are still able to breathe partially. Encourage them to continue coughing as it may dislodge the obstruction. However, be ready to take action with back blows and chest thrusts if necessary.Q: How do I perform five back blows on an infant?
A: To perform five back blows, hold the infant face down along your forearm, supporting their head and neck, and use the heel of your hand to deliver firm back blows between the infant's shoulder blades, aiming to dislodge the object.Q: When should I call the local emergency number if a baby is choking?
A: Call the local emergency number immediately if the baby becomes unconscious, is unable to cough or breathe forcefully, or is unable to dislodge the object with back blows and chest thrusts.Q: What are the steps if the infant becomes unconscious while choking?
A: If the infant becomes unconscious, you should call emergency services and begin CPR. Lay the infant on a flat surface and perform 30 chest compressions followed by two rescue breaths. Continue this cycle until the object is dislodged or help arrives.Q: What are some common items that pose a risk for choking in infants?
A: Common items that pose a risk for choking in infants include small toys, buttons, coins, nuts, grapes, and pieces of hard food. Always supervise infants during playtime and meal times to help save lives.Q: Can St John Ambulance provide guidance on baby first aid?
A: Yes, St John Ambulance offers comprehensive first aid advice and training, including baby first aid courses that cover choking and other emergencies.







 Login with Google
Login with Google Login with Facebook
Login with Facebook