
Infant choking can lead to brain injury, permanent disability, or even death. It is, therefore, important for parents and caregivers to assist in saving the life of the child who has had a choking incident. In this article, parents and caregivers are educated on attempting to intervene during choking emergencies involving children of 1 year of age. The article explains the general features that may suggest the child has had a choking episode; what steps can one take to intervene when such an episode occurs? What can be done to prevent such episodes from occurring again? These are critical skills that every parent and caregiver should learn, for they affect how quickly the child can survive an emergency.
What are the signs of choking in a 1-year-old?
If a one-year-old child is choking, a few signs and symptoms may be present, including shortness of breath, ineffective coughs, and no sounds made, such as crying. The child may also be distressed by things like holding their neck or looking afraid. In addition, the infant may go through a stage where his or her skin is unusually blue and pale due to hypoxic nature, and they might even become unconscious in some extreme cases. Identifying these signs with speed enables effective response that helps the situation.
How to recognize if a child is choking
Whenever I feel a child struggling to breathe, I monitor the child's behavioral and physical symptoms. A child appearing to be choking may not be able to speak, let out a cry, or cough. Instead, they may look in a panic, trying to reach for their neck. There are other visible signs I look out for, such as cyanosis, which is a bluish tint to the skin close to the lips, or even the absence of breath, which could indicate severe stress or difficulty in breathing. In extreme cases, the child may even become unconscious. I try my best to remain composed and calm because it helps me understand the issue more clearly and work on providing help as quickly as possible.
Common choking hazards for 1-year-olds
Some common food-related objects that might constitute choking hazards for a one-year-old child are whole grapes, nuts, popcorn, hotdogs, chunks of meat or cheese, etc. These are small enough for a one-year-old child to choke on or too large for a child to swallow whole. There are also small toys, deflated balloons, marbles, and coin-button batteries, which have a considerable amount of risk associated with them.
To help limit the potential for choking, all food that can pose a danger should be cut into smaller portions that are easier to handle. Grapes and cherry tomatoes, for example, should always be cut into quarters. Furthermore, it is advisable to put all pieces of toys out of a child’s reach. Many foods should not be given to children below the age of four, particularly round or cylindrical foods, as these can be easily stuck in a child's windpipe. In support of this notion, the American Academy of Pediatrics further argues that toy parts should not be less than 1.25 inches in diameter and 2.25 inches in length. Supervising activities during meal and play times is therefore essential in averting instances of choking.
When to call for emergency help
When a child shows such symptoms, they might possess an item in their throat. In such cases, the first thing to do is connect with the emergency service immediately. If no sounds are being produced and the child is making serious attempts at coughing with light sounds coming from their throat, in such cases, they have a complete airway obstruction. If such a child goes on to lose consciousness, then the process of administrating CPR should begin as it would allow them to stay faintly alive for some time. Infants that are a year minus should be given back thumps, as the Red Cross suggests, and any child older than that can be given a combination of back hits and naval thrust. Even if the item goes out, but an injury is acquired, contacting a professional medical person is imperative.
What are the first aid steps for a choking 1-year-old?
If a 1-year-old child begins choking, immediate and precise actions are critical to clear the airway and prevent further complications. Follow these steps carefully:
- Assess the Situation
Confirm whether the child is indeed choking. Signs to watch for include an inability to cough, speak, or breathe and cyanosis (blue skin or lips). If the child is coughing forcefully, encourage them to continue coughing, as this is the most effective way to expel the object naturally. Avoid interfering unless the child’s airway becomes fully obstructed.
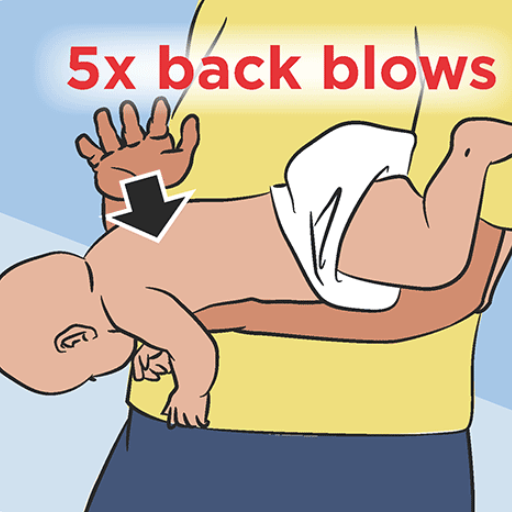
- Deliver Back Blows
Position the baby face-down along your forearm, supporting their head and neck securely with your hand. Using the heel of your other hand, deliver up to five firm back blows between the shoulder blades. Ensure the child's head is lower than their chest to utilize gravity effectively.
- Perform Chest Thrusts
If the object has not been dislodged, turn the baby face up and lay it on your forearm or a firm surface. Using two fingers, apply up to five quick chest thrusts to the lower third of the sternum. Aim to produce enough pressure to expel the object without causing injury.
- Repeat as Necessary
Alternate between back blows and chest thrusts until the object is cleared or the child becomes unresponsive. If the obstruction persists, proceed to call 911 and begin CPR if trained.
- Seek Medical Attention
Even if the object is successfully dislodged, a medical evaluation is essential to ensure no secondary injuries or complications occur from the incident.
Carefully following these steps and preparing ahead of time through training can make a critical difference in an emergency involving a choking infant.
Back Blows Technique for Infants
To execute the back blows technique, I first see that an infant is well supported by placing her face and body downwards along my forearm and making sure her head is lower than her chest. With the heel of my hand, I am performing up to five, but no more than five, firm and controlled back blows between the infant’s shoulder blades. I aim to exert sufficient force to dislodge the obstruction but not at the expense of the sensitivity of the infant’s architecture. If the object is still lodged, chest thrusts, as outlined above, are alternately applied. Safety and efficiency are the two significant concerns at every procedure stage. Treat an airway obstruction medically for all possible inflicted damage to be checked out.
Chest Thrusts for Young Children
The chest thrust technique is critical in managing an obstructed airway in young children. For young children with throats blocked, use chest thrusts first, putting the child on the back and supporting him firmly on some surface. With the child’s chest up in a downward direction, use two fingers to place yourself about a little above the child’s nipple line. Getting at least one or two fingers deep, around one to one and a half inches for those under a year and around one-third of an adult’s chest for children aged one and above, never surpassing two inches. If the hands are still deep in the chest, try for three thrusts and two rapid repetitions, and every time one thrust is deftly able to allow the child’s chest to revert to its original position, the forward motion follows right after.
The essence of these thrusts or movement towards these thrusts, for that matter, is to provide enough force to push the object away. But in case that was not successful, after continuing to alternate between the two measures, I would seek the assistance of medical services with the help of some of my colleagues. The changes occurring while ignoring the mouth can be the best details I can give to attending medical practitioners.
These safety measures in guidelines must be sufficiently understood and practiced so that one can be effective in performing this life-saving procedure. They include the recommendations from the American Heart Association or Red Cross.
How to perform infant CPR if needed
To do infant CPR, start by placing the child on a flat surface. Next, rub the child’s foot and shout. Call their name; if the child does not respond or does not breathe at all, then commence CPR.
With one hand, place the middle two fingers on the center of the nipple lines on the lower part of the chest. Then, Depress the chest around one and a half inches (or one-third the depth of the infant’s chest) at a rate of 100 and 120 times every minute. Each time in between the chest beats, allow it to rest in its `original` position.
For every 30 beats, you need to give 2 mouth-to-mouth beats. For every inhale of yours, apply your mouth onto the child’s mouth and nose while inhaling until the chest starts moving. Infants do not have a large lung volume capacity, so a bit of air is enough to move the chest. Proceed by repeating the cycle of 30 beats and two mouth-to-mouth inhalations until life signs return or until the emergency medical services arrive, but always Make sure that emergency medical services have called for help.
How do I perform back blows on a choking 1-year-old?
When attempting back blows on a choking toddler, it is mandatory to ensure that the child’s airway is blocked while the child is still conscious. In this case, the toddler should be placed head down along the length of your forearm while holding its head and neck with your palm. Your forearm should rest on your thigh for support. Now, do not forget about using your other palm heel, this time causing enduring up to 5 slaps between the toddler’s shoulder blades, then check after every hit if the point is cleared or not. If the item is not removed, attempt abdominal thrusts or call an ambulance. Whatever happens, stay awake while looking at the baby and ensure EMS is standing by.
Proper positioning for back blows
.The following procedures will help in proper positioning of the infant by back blows, especially if they are a choking 1-year-old.
- The Infant is Secured: The baby is held in an infant position, with the chest uppermost and the head on the arm, so gravity can work on loosening up the blockage.
- Head and Neck Supported: One hand supports the neck and head of the infant while the baby's chin is placed on the palm. The arms of the carrier help stabilize the rest of the body.
- Resting Position: Positioning the forearm on the thigh or the lap helps one be more stable and in control. This reduces the chances of an accidental injury during the procedure.
- Contact Points: The person giving the blows backs the head with the heel of another hand. The back blow is done at five intervals and is done centrally between the baby’s shoulder areas. All the controlled blows must compress the windpipe to help clear the blockage, if any.
Technical parameters:
- Ensure the baby’s head is lowered to approximately 15 to 30 degrees in relation to the chest.
- Back blows delivered must be strong enough to inflict no damage to ribs and backs but may be powerful enough to cause puffs of wind.
Always check after every blow with a back fist to see if ANOTHER OBJECT HAS COME OUT. Change to chest thrusts and call for further medical help if the obstruction continues to remain after five blows.
Technique for delivering effective back blows.
Effective back blows require that the head of the infant be at least at a 15 and 30-degree angle in relation to the chest. When trying to remove a foreign object from an infant, the focus number of the blows between the shoulder blades is two. The blows aim to attempt to tell the object that it should not be where it is without playing too rough. After delivering these two controlled blows, I check whether the obstruction has been cleared. If these blows do not provide relief, chest thrusts can be performed in dire combat situations.
When to switch to chest thrusts
If within five attempts to perform a back blow, it’s not successful, combining with the Five Thrusts rule, I begin with twisting the chest, the thumbs, and the fingers together to create enough force while aiming above the navel and below the nipple. It is also important to note that the infant should remain in the English position where the infant's head is also on one side, promising a lower angle than the vertebrae. To be effective, all of these methods should be time-adequate; otherwise, it will lead to delayed oxygen intake, which can cause permanent damage.
What should I do if back blows don't work?
In case back blows do not help, the performance of chest thrusts can be performed right away, which is stated in the emergency procedures. In this case, the baby can be placed on its back while its head is positioned lower than its chest while the throat is compressed using either two or three fingers at the region below the nipples. At the same time, I will ensure that if the obstruction remains, further order care is available by calling an ambulance. Continue changing between blows and chest thrusts until the object emerges or a doctor treats the individual.
Transitioning to chest thrusts
- Infant Positioning
- Lay the infant face up on a firm, flat surface or your lap.
- Ensure the infant's head is lower than the chest to utilize gravity to remove objects.
- Hand Placement
- Use two or three fingers to locate the correct compression point, just below the nipple line on the breastbone.
- Ensure accurate finger placement to avoid compressing the ribs or other fragile areas.
- Chest Compression Parameters
- Deliver compressions with a depth of approximately 1.5 inches (4 cm).
- Perform compressions at a steady rhythm, allowing the chest to return to its normal position between thrusts.
- Emergency Protocol
- Continue alternating between five back blows and five chest thrusts if the obstruction is not expelled.
- While awaiting professional medical assistance, monitor the infant carefully for changes, such as unresponsiveness or signs of oxygen deprivation.
Adhering to these steps and maintaining the recommended parameters can optimize the chances of clearing the airway while minimizing injury risk.
How to perform chest thrusts on a 1-year-old
When giving chest thrusts to a one-year-old, the first step I would take is t to place the child on their back, lying down on a hard surface such as my lap or the ground. I would then pinpoint the part three inches below the breast line as the intervention area. Using two fingers appears ideal while performing these thrusts as I do not exert much pressure, only enough to reach the desired force. The thrusts must provide a reasonable thrusting force and must not be blocked from bursting outward in between the chest compressions. If the Einhorn’s airways do not open, I would give five effective thrusts between five back blows while checking if the child has regained motion or normal breathing. This procedure is part of diverse health guidelines for the kid to ensure safety and effectiveness.
Alternating between back blows and chest thrusts
As I alternate between back blows and chest thrusts, I would ensure that every action is performed effectively to maximize the chances of dislodging the obstruction. I would then begin the primary management technique by appealing to the back of the child’s chest, this time using only five powerful swipes between the child’s scapulae using the palm as the kid is placed face down on my arm and making sure that their head is lower than their chest. In this technique, After five back blows to the child’s chest, the child would be turned to his back and placed on firm support before performing five chest thrusts, as previously explained. This pattern, along with the back blows, would be acknowledged and carried out until the child has shown any possibility of the obstruction being cleared, and in such occasions, the child’s response and breathing would be the main factors to look for. Where no result is achieved, I would repeat the cycle until I get a physician's help.
When should I call 911 or emergency services?
Always try to seek out emergency services or dial 911 when the child appears to worsen, doesn’t respond, or stops breathing. In these times, do not hesitate to give the needed back slaps and chest pumps. If the child isn’t improving, then start CPR. Until the paramedics arrive, make sure you clear the child’s airway and, if need be, ensure they are still breathing.
Signs that indicate immediate medical attention is needed
In this case, the child is in an emergency, and there’s no mouth-to-mouth resuscitation in this context, as I told you. Rescue breathing is unnecessary, back blows and chest thrusts will be used instead. The only thing I would like to do in this case is to clear the airway of any obstructions. Call emergency services immediately once the child stops wheezing and struggling and has ranged their motions to a minimum. The fact that there is no effort to inhale towards the mouth would serve as a ‘red flag’ for me. Resuscitation would be the term I would prefer to use. To describe that in more detail, Continue doing routine standard procedures and push for the flow of desperation.
What to tell the emergency dispatcher
While giving some life-threatening details of the incident over the emergency phone, I would always start by saying my name and location. Then, I would provide the phone number. I would say that I was present with a child who was unable to breathe correctly, had a blue face, and was unconscious. There would be additional details, for instance, how old the child was and the assistance I tried to give, including back blows, chest thrusts, and mouth-to-mouth. If CPR were in progress, I would mention the number of strokes plus the compressing force, which I believed was reasonable. It was also about 1/3 of the area of the chest. I would also, however, be careful to do what the telephone operator asked me and not hang up until help came. I would stress out and still manage to speak without panicking and Being appropriately heard, bearing in mind that the professionals on the other side need to channel their energies effectively to maintain the health and safety of the child.
Continuing first aid while waiting for help to arrive
In a first aid situation, the very first thing I would do is assess the surrounding scene to make sure no more harm is inflicted. If the person collapses and ceases to breathe, CPR I’m going to administer while making sure that the compression’s depth reaches 5 cm but stays below 6 cm, counting 100 to 120 compressions per minute until the emergency personnel arrive; if a person is looking pale and breathes fast, an intentional direct pressure using a clean cloth on the source of bleeding mainly focus at that stage whilst aiming not to injure any parts further controls blood. However, if the individual in question has a blockage in the throat but can still talk, he or she would be advised to use the Heimlich maneuver to help force out the obstruction from the throat. In this case, I shall constantly refrain from coughing out gentle breaths, and instead, I’d be taking care of my pulse and overall breathing to keep them as easy in case of anything abrupt.
References
Choking Thorax Respiratory tractFrequently Asked Questions (FAQ)
Q: What are the first aid steps for a child who is choking?
A: The first aid steps for a choking 1-year-old child include: 1) Assess the situation quickly, 2) Give five back blows between the shoulder blades, 3) If ineffective, perform five abdominal thrusts (modified Heimlich maneuver), 4) Alternate between back blows and abdominal thrusts until the object is dislodged or the child becomes unconscious. Always call for emergency help if the situation doesn't resolve quickly.Q: How do I perform back blows on a choking 1-year-old?
A: To perform back blows on a choking 1-year-old: 1) Place the child face down on your thigh, supporting their head, 2) Give up to 5 sharp blows between the shoulder blades with the heel of your hand, 3) Check if the object has been dislodged after each blow. The American Red Cross recommends this technique as an essential first aid skill for helping a choking child.Q: What are abdominal thrusts, and how do I perform them on a 1-year-old?
A: Abdominal thrusts, also known as the Heimlich maneuver, are performed on a 1-year-old by: 1) Place the child face up on your thigh, 2) Place two fingers just above the navel, 3) Give five quick, upward thrusts, 4) Check the mouth for the object after each thrust. This technique helps dislodge objects blocking the airway.Q: When should I use a first aid app during a choking emergency?
A: A first aid app can be a valuable resource, but in an active choking emergency, focus on immediate action rather than consulting an app. Use a first aid app from organizations like the Red Cross before emergencies to learn and practice first aid skills or after the immediate crisis has passed for follow-up care information.Q: How do I know if a 1-year-old is choking or just coughing?
A: A choking 1-year-old will show signs of distress, such as an inability to cry, speak, or breathe effectively, and may have a panicked expression. They may grasp at their throat. If the child is coughing forcefully, encourage them to continue, as this may dislodge the object. First aid is performed for choking only if the cough becomes ineffective or the child cannot breathe.Q: What should I do if I can see the object in the child's mouth?
A: If you can see the object in the child's mouth and it's easy to remove, sweep it out with your finger. However, don't perform blind finger sweeps, as this may push the object further into the airway. If you cannot see the object, continue with back blows and abdominal thrusts as first aid guidelines recommend.Q: When should I call for emergency help for a choking 1-year-old?
A: You should call for emergency help immediately if: 1) The child becomes unconscious, 2) You've performed multiple cycles of back blows and abdominal thrusts without success, 3) The child's breathing becomes labored, or they turn blue. It's best to have someone else call for help while you continue first aid efforts. If you're alone, perform first aid for about 1 minute before calling for help.Q: How can I prevent choking incidents in 1-year-old children?
A: To prevent choking in 1-year-olds: 1) Cut food into small, manageable pieces; 2) Avoid giving them hard candies, nuts, whole grapes, or hot dogs; 3) Keep small objects out of reach, 4) Supervise meal times, 5) Teach them to sit while eating, 6) Encourage thorough chewing. Additionally, learning first aid skills and keeping emergency numbers handy can help you respond quickly if choking occurs.

















 Login with Google
Login with Google Login with Facebook
Login with Facebook