
Checking the pulse during CPR is a critical step in assessing whether the heart has resumed adequate circulation. This article examines the significance of pulse checks, outlines the correct procedure for performing them, and discusses their crucial role in guiding life-saving actions during cardiac emergencies. Learn how this simple yet vital skill can make a difference in critical moments.
Understanding Cardiac Arrest
What is Cardiac Arrest?
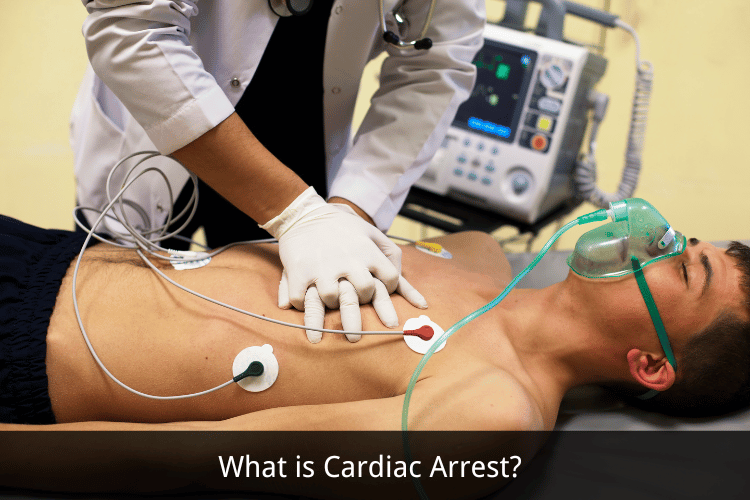 Cardiac arrest is a sudden and life-threatening condition in which the heart unexpectedly stops beating. This abrupt cessation of heart function disrupts the flow of blood to vital organs, including the brain and lungs, leading to a loss of consciousness and, if untreated, death within minutes. Unlike a heart attack, which occurs due to a blockage in the blood vessels supplying the heart, cardiac arrest is primarily an electrical problem. It is often caused by arrhythmias, such as ventricular fibrillation, in which the heart's electrical signals become chaotic, preventing it from pumping blood effectively.
Cardiac arrest can occur without warning and affects individuals of all ages, including those with no prior history of heart disease. Common risk factors include coronary artery disease, heart failure, and inherited conditions like long QT syndrome. External factors, such as drug overdose, severe trauma, or drowning, can also trigger cardiac arrest. Understanding the nature of this condition is crucial for recognizing its urgency and taking appropriate action.
Cardiac arrest is a sudden and life-threatening condition in which the heart unexpectedly stops beating. This abrupt cessation of heart function disrupts the flow of blood to vital organs, including the brain and lungs, leading to a loss of consciousness and, if untreated, death within minutes. Unlike a heart attack, which occurs due to a blockage in the blood vessels supplying the heart, cardiac arrest is primarily an electrical problem. It is often caused by arrhythmias, such as ventricular fibrillation, in which the heart's electrical signals become chaotic, preventing it from pumping blood effectively.
Cardiac arrest can occur without warning and affects individuals of all ages, including those with no prior history of heart disease. Common risk factors include coronary artery disease, heart failure, and inherited conditions like long QT syndrome. External factors, such as drug overdose, severe trauma, or drowning, can also trigger cardiac arrest. Understanding the nature of this condition is crucial for recognizing its urgency and taking appropriate action.
Signs and Symptoms of Cardiac Arrest
The signs of cardiac arrest are immediate and dramatic, making it essential to act quickly. The most obvious symptom is a sudden collapse, often accompanied by a complete loss of consciousness. The individual will not respond to verbal or physical stimuli and may appear lifeless. Breathing may stop entirely or become irregular and gasping, a phenomenon known as agonal breathing, which is a critical indicator of cardiac arrest. Other symptoms include the absence of a pulse, as the heart is no longer pumping blood. In some cases, individuals may experience warning signs before cardiac arrest occurs, such as chest pain, shortness of breath, dizziness, or palpitations. However, these symptoms are not always present, and cardiac arrest can strike without any prior indication. Recognizing these signs and symptoms is vital for initiating life-saving measures, such as cardiopulmonary resuscitation (CPR) and the use of an automated external defibrillator (AED).The Importance of Immediate Response
The key to surviving cardiac arrest lies in the speed and effectiveness of the response. Every minute that passes without intervention reduces the chances of survival by approximately 10%. Immediate action, such as performing CPR and using an AED, can double or even triple the likelihood of survival. CPR helps maintain blood flow to the brain and other vital organs, while an AED delivers an electric shock to restore the heart's normal rhythm. Bystanders play a critical role in the chain of survival. Recognizing the signs of cardiac arrest and calling emergency services is the first step. While waiting for professional help to arrive, performing high-quality chest compressions and using an AED, if available, can make a life-saving difference. Public access to AEDs in workplaces, schools, and community spaces has significantly improved survival rates, but awareness and training remain essential. In addition to immediate response, post-resuscitation care in a medical facility is crucial for addressing the underlying cause of cardiac arrest and preventing recurrence. This may include advanced treatments such as therapeutic hypothermia, coronary interventions, or implantable defibrillators. By understanding the importance of rapid action and comprehensive care, individuals and communities can improve outcomes for those experiencing cardiac arrest.CPR Basics
What is CPR?
 Cardiopulmonary Resuscitation (CPR) is a life-saving emergency procedure performed when a person’s heart stops beating or they stop breathing. It is designed to maintain blood flow and oxygen delivery to vital organs, such as the brain and heart, until advanced medical care can be provided. CPR combines chest compressions, which manually pump blood through the heart, with rescue breaths, which supply oxygen to the lungs. This technique is critical in situations like cardiac arrest, drowning, or severe trauma, where immediate intervention can mean the difference between life and death.
CPR is a skill that can be learned by anyone, from healthcare professionals to laypersons. It is often taught alongside the use of automated external defibrillators (AEDs), which can restore a normal heart rhythm during cardiac arrest. While CPR does not restart the heart, it buys valuable time by keeping blood and oxygen circulating until professional help arrives.
Cardiopulmonary Resuscitation (CPR) is a life-saving emergency procedure performed when a person’s heart stops beating or they stop breathing. It is designed to maintain blood flow and oxygen delivery to vital organs, such as the brain and heart, until advanced medical care can be provided. CPR combines chest compressions, which manually pump blood through the heart, with rescue breaths, which supply oxygen to the lungs. This technique is critical in situations like cardiac arrest, drowning, or severe trauma, where immediate intervention can mean the difference between life and death.
CPR is a skill that can be learned by anyone, from healthcare professionals to laypersons. It is often taught alongside the use of automated external defibrillators (AEDs), which can restore a normal heart rhythm during cardiac arrest. While CPR does not restart the heart, it buys valuable time by keeping blood and oxygen circulating until professional help arrives.
How CPR Works in Cardiac Arrest
During cardiac arrest, the heart’s electrical system malfunctions, causing it to stop pumping blood effectively. Without blood flow, the brain and other vital organs begin to suffer damage within minutes. CPR works by mimicking the heart’s pumping action, manually circulating blood to deliver oxygen and nutrients to the body. Chest compressions create pressure that forces blood out of the heart and into the arteries, while rescue breaths replenish oxygen levels in the lungs. The effectiveness of CPR depends on the quality of chest compressions. Compressions should be performed at a rate of 100 to 120 per minute and at a depth of at least 2 inches for adults. Proper technique ensures that enough blood is circulated to sustain organ function. When combined with the use of an AED, which delivers an electric shock to restore the heart’s rhythm, CPR significantly increases the chances of survival. Even in cases where an AED is not immediately available, high-quality CPR can double or triple the likelihood of a positive outcome.Steps to Perform CPR
Performing CPR correctly is essential for maximizing its effectiveness. The following steps outline the basic procedure for administering CPR to an unresponsive individual:- Check for Responsiveness and Call for Help: Tap the person on the shoulder and shout to see if they respond. If there is no response, call emergency services immediately or ask someone else to do so. If an AED is available, retrieve it or have someone bring it to the scene.
- Assess Breathing and Pulse: Check if the person is breathing normally by looking for chest movement and listening for breath sounds. Simultaneously, check for a pulse at the neck or wrist. If there is no pulse or the person is not breathing, begin CPR immediately.
- Perform Chest Compressions: Place the heel of one hand on the center of the person’s chest, just below the breastbone. Place your other hand on top and interlock your fingers. Push hard and fast, compressing the chest at least 2 inches deep at a rate of 100 to 120 compressions per minute. Allow the chest to fully recoil between compressions.
- Provide Rescue Breaths: After 30 compressions, open the person’s airway by tilting their head back and lifting their chin. Pinch their nose shut, seal your mouth over theirs, and give two slow breaths, each lasting about one second. Ensure the chest rises with each breath. If you are untrained or uncomfortable giving rescue breaths, continue with hands-only CPR.
- Use an AED if Available: Turn on the AED and follow its voice prompts. Attach the electrode pads to the person’s bare chest as instructed. The AED will analyze the heart’s rhythm and advise whether a shock is needed. If a shock is advised, ensure no one is touching the person and press the shock button. Resume CPR immediately after the shock.
- Continue Until Help Arrives: Keep performing cycles of 30 compressions and 2 breaths, or hands-only compressions if preferred, until emergency medical personnel take over or the person shows signs of recovery, such as breathing or movement.
Checking the Pulse
What is a Pulse Check?
 A pulse check is a simple yet critical step in assessing a person’s circulatory status. It involves feeling for the rhythmic throbbing of blood as it flows through the arteries, which is caused by the heart’s contractions. Checking the pulse helps determine whether the heart is effectively pumping blood and can provide valuable information about a person’s overall health. In emergency situations, such as cardiac arrest, a pulse check is used to confirm whether the heart has stopped beating, guiding the decision to begin cardiopulmonary resuscitation (CPR).
The pulse can also indicate the strength and rhythm of the heartbeat. A strong, regular pulse suggests normal heart function, while an irregular or weak pulse may signal underlying issues, such as arrhythmias or shock. In non-emergency settings, monitoring the pulse can help track fitness levels, detect stress, or identify potential health concerns. Knowing how to perform a proper pulse check is an essential skill for both medical professionals and laypersons.
A pulse check is a simple yet critical step in assessing a person’s circulatory status. It involves feeling for the rhythmic throbbing of blood as it flows through the arteries, which is caused by the heart’s contractions. Checking the pulse helps determine whether the heart is effectively pumping blood and can provide valuable information about a person’s overall health. In emergency situations, such as cardiac arrest, a pulse check is used to confirm whether the heart has stopped beating, guiding the decision to begin cardiopulmonary resuscitation (CPR).
The pulse can also indicate the strength and rhythm of the heartbeat. A strong, regular pulse suggests normal heart function, while an irregular or weak pulse may signal underlying issues, such as arrhythmias or shock. In non-emergency settings, monitoring the pulse can help track fitness levels, detect stress, or identify potential health concerns. Knowing how to perform a proper pulse check is an essential skill for both medical professionals and laypersons.
How to Check the Carotid Pulse
The carotid pulse, located in the neck, is one of the most reliable sites for assessing circulation, especially in emergencies. The carotid arteries are large blood vessels that supply oxygen-rich blood to the brain, making their pulse easy to detect even when blood flow is reduced. Here’s how to check the carotid pulse:- Position the Person: Ensure the individual is lying flat on their back. This position makes it easier to access the neck and reduces the risk of fainting if the person is conscious but weak.
- Locate the Carotid Artery: Place two fingers—preferably the index and middle fingers—on one side of the neck, just below the jawline and to the side of the windpipe. Avoid using your thumb, as it has its own pulse that can interfere with accurate detection.
- Apply Gentle Pressure: Press lightly against the neck until you feel a rhythmic throbbing. Be cautious not to press too hard, as excessive pressure can restrict blood flow or cause discomfort. If you don’t feel a pulse on one side, try the other side of the neck.
- Count the Beats: Once you locate the pulse, count the beats for 15 seconds and multiply by four to calculate the heart rate in beats per minute (BPM). A normal resting heart rate for adults ranges from 60 to 100 BPM, but this can vary based on factors like age, fitness level, and health conditions.
Checking for a Pulse in Other Areas
In addition to the carotid artery, there are several other locations where a pulse can be checked, depending on the situation and the individual’s condition. These include:- Radial Pulse (Wrist): The radial pulse is located on the thumb side of the wrist, just below the base of the thumb. It is commonly used in non-emergency settings to monitor heart rate and circulation. To check the radial pulse, place two fingers on the wrist and press gently until you feel the beats.
- Brachial Pulse (Arm): The brachial pulse is found on the inside of the upper arm, near the elbow. It is often used for infants or young children, as their smaller size makes other pulse points harder to detect. To locate the brachial pulse, press two fingers along the inside of the arm, between the biceps and triceps.
- Femoral Pulse (Groin): The femoral pulse is located in the groin area, where the femoral artery passes close to the skin. This pulse is typically checked in cases of severe trauma or shock, as it provides a strong indication of central circulation. To find the femoral pulse, press firmly in the crease where the thigh meets the pelvis.
- Dorsalis Pedis and Posterior Tibial Pulses (Feet): These pulses are located on the top of the foot (dorsalis pedis) and behind the ankle (posterior tibial). They are often used to assess circulation in the lower extremities, particularly in individuals with diabetes or peripheral artery disease.
First Responders' Role
Who are First Responders?
 First responders are individuals who are among the first to arrive and provide assistance during emergencies, such as accidents, natural disasters, or medical crises. This group typically includes paramedics, firefighters, police officers, and emergency medical technicians (EMTs). Their primary role is to stabilize the situation, provide immediate care, and ensure the safety of those involved until more specialized medical or rescue teams arrive. In some cases, first responders may also include trained volunteers or community members who step in to assist during critical moments.
These professionals are equipped to handle a wide range of emergencies, from administering life-saving interventions like CPR and defibrillation to managing hazardous environments. Their quick actions can significantly improve outcomes, especially in time-sensitive situations like cardiac arrest or severe trauma. First responders are not only trained to address physical injuries but also to provide emotional support to victims and their families, helping to reduce panic and maintain order during chaotic events.
First responders are individuals who are among the first to arrive and provide assistance during emergencies, such as accidents, natural disasters, or medical crises. This group typically includes paramedics, firefighters, police officers, and emergency medical technicians (EMTs). Their primary role is to stabilize the situation, provide immediate care, and ensure the safety of those involved until more specialized medical or rescue teams arrive. In some cases, first responders may also include trained volunteers or community members who step in to assist during critical moments.
These professionals are equipped to handle a wide range of emergencies, from administering life-saving interventions like CPR and defibrillation to managing hazardous environments. Their quick actions can significantly improve outcomes, especially in time-sensitive situations like cardiac arrest or severe trauma. First responders are not only trained to address physical injuries but also to provide emotional support to victims and their families, helping to reduce panic and maintain order during chaotic events.
First Responder Training and CPR
First responders undergo rigorous training to prepare them for the diverse challenges they may face in emergency scenarios. A key component of their training is learning how to perform cardiopulmonary resuscitation (CPR) and use automated external defibrillators (AEDs). These skills are critical for managing cardiac arrest, where every second counts in preserving brain function and increasing the chances of survival. CPR training for first responders goes beyond basic techniques taught to the general public. It includes advanced methods such as team-based resuscitation, airway management, and the use of specialized equipment. For example, paramedics and EMTs are trained to use bag-valve masks for ventilation and may administer medications to support heart function. Firefighters and police officers, while not primarily medical professionals, are often trained in basic life support (BLS) to provide immediate care before paramedics arrive. In addition to CPR, first responders are trained to assess the scene of an emergency, identify potential hazards, and prioritize care based on the severity of injuries. This comprehensive training ensures that they can act decisively and effectively, even in high-pressure situations. Their ability to perform CPR and other life-saving interventions is a cornerstone of their role, making them an essential part of the emergency response system.Collaborative Efforts in Emergency Situations
Emergency situations often require a coordinated response from multiple agencies and individuals, making collaboration a vital aspect of a first responder’s role. Effective teamwork among paramedics, firefighters, police officers, and other emergency personnel ensures that resources are used efficiently and that victims receive the best possible care. For example, in a car accident, police may secure the scene and direct traffic, firefighters may extract trapped individuals, and paramedics may provide medical treatment—all working together seamlessly. Communication is a key element of this collaboration. First responders use standardized protocols and clear communication channels to share information about the situation, such as the number of victims, the severity of injuries, and any potential risks. This allows each team to focus on their specific responsibilities while maintaining a unified approach to the emergency. In addition to professional teams, first responders often work alongside bystanders or community members who may have initiated CPR or provided first aid before their arrival. Recognizing and integrating these efforts into the overall response can further improve outcomes. Public education campaigns that encourage CPR training and AED use have empowered more people to act as "immediate responders," bridging the gap until professional help arrives. By fostering collaboration and maintaining a high level of preparedness, first responders play a crucial role in managing emergencies and saving lives. Their ability to work together under challenging conditions highlights the importance of teamwork and training in the field of emergency response.First Aid Considerations
Importance of First Aid in Cardiac Events
First aid plays a critical role in managing cardiac emergencies, as it provides immediate care that can stabilize a person’s condition before professional medical help arrives. In the case of cardiac arrest, timely first aid interventions, such as cardiopulmonary resuscitation (CPR) and the use of an automated external defibrillator (AED), can significantly increase the chances of survival. These actions help maintain blood flow to vital organs, particularly the brain and heart, during the critical minutes following a cardiac event. Beyond CPR, first aid also involves assessing the individual’s condition, ensuring their airway is clear, and monitoring for signs of life, such as breathing or movement. It is equally important to create a safe environment by removing potential hazards, such as sharp objects or electrical equipment, that could pose additional risks. First aid not only addresses the immediate physical needs of the individual but also provides emotional reassurance, helping to reduce panic and maintain calmness during a high-stress situation.Performing First Aid Alongside CPR
When faced with a cardiac emergency, combining first aid techniques with CPR can enhance the effectiveness of your response. The first step is to assess the situation and determine whether the individual is unresponsive and not breathing normally. If these signs are present, begin CPR immediately while ensuring someone calls emergency services or retrieves an AED. While performing CPR, it’s important to follow proper techniques to maximize its impact. Chest compressions should be delivered at a rate of 100 to 120 per minute and at a depth of at least 2 inches for adults. If you are trained in providing rescue breaths, alternate 30 compressions with 2 breaths, ensuring the airway is open by tilting the head back and lifting the chin. If you are untrained or uncomfortable with rescue breaths, hands-only CPR is still highly effective and should be continued until help arrives. If an AED is available, it should be used as soon as possible. Turn on the device and follow its voice prompts to attach the electrode pads to the individual’s chest. The AED will analyze the heart’s rhythm and advise whether a shock is needed. If a shock is recommended, ensure no one is touching the individual before pressing the shock button. Resume CPR immediately after the shock and continue until emergency personnel take over.When to Call for Help
Knowing when to call for professional medical assistance is a vital part of first aid in cardiac emergencies. If you encounter someone who is unresponsive, not breathing, or gasping for air, call emergency services immediately. Providing the dispatcher with clear and concise information about the individual’s condition, location, and any actions already taken can help ensure a faster and more effective response. In addition to cardiac arrest, other symptoms that warrant an immediate call for help include severe chest pain, difficulty breathing, sudden weakness or numbness, and loss of consciousness. These signs may indicate a heart attack or stroke, both of which require urgent medical attention. Even if the individual regains consciousness or begins breathing on their own, it is essential to have them evaluated by healthcare professionals to address any underlying issues and prevent further complications. While waiting for emergency responders, continue providing first aid and CPR as needed. If possible, assign someone to guide the medical team to the scene or provide additional assistance, such as crowd control or retrieving necessary equipment. By acting quickly and decisively, you can make a significant difference in the outcome of a cardiac emergency.Frequently Asked Questions
Q: What is the importance of checking the pulse during CPR?
A: Checking the pulse during cardiopulmonary resuscitation (CPR) is essential for determining whether the heart has resumed spontaneous circulation. If no pulse is detected, it indicates that the heart is not effectively pumping blood, and chest compressions should be started immediately to restore blood flow to vital organs. This step ensures that life-saving measures are applied without delay.
Q: How do I check a pulse effectively during CPR?
A: To check a pulse effectively during CPR, locate the carotid artery on the side of the neck. Use your index and middle fingers to gently palpate the area just below the jawline and to the side of the windpipe. Perform this check within 10 seconds to avoid unnecessary delays. If no pulse is felt, begin chest compressions right away.
Q: What should I do if I find a pulse during CPR?
A: If you detect a pulse during CPR, focus on monitoring the individual’s pulse and breathing. If the person remains unresponsive but has a pulse, do not perform chest compressions. Instead, provide rescue breaths at a rate of one breath every 5-6 seconds (10-12 breaths per minute) and continue basic life support (BLS) until emergency medical services arrive.
Q: How often should I check the pulse during CPR?
A: The pulse should be checked every 2 minutes while performing CPR. This interval allows you to evaluate whether spontaneous circulation has returned and ensures that chest compressions remain effective. Avoid prolonged interruptions during pulse checks to maintain the quality of CPR.
Q: What are the guidelines for checking a pulse during CPR?
A: According to the American Heart Association (AHA) guidelines, pulse checks during CPR should be quick and efficient, lasting no more than 10 seconds. If no pulse is detected within this time frame, chest compressions should be resumed immediately to avoid delays in blood circulation.
Q: Can I perform hands-only CPR without checking the pulse?
A: Yes, hands-only CPR is recommended for untrained bystanders or those unsure about checking a pulse. If the person is unresponsive and not breathing normally, it is safer to begin chest compressions immediately rather than spend time attempting to detect a pulse. Hands-only CPR can still be highly effective in maintaining blood flow.
Q: What is the role of a rescuer in checking the pulse during CPR?
A: The rescuer’s role in checking the pulse during CPR is to assess whether the heart is pumping blood effectively quickly. Based on the presence or absence of a pulse, the rescuer must decide whether to continue chest compressions, provide rescue breaths, or monitor the individual’s condition. Timely and accurate pulse checks are critical for guiding life-saving actions.
Q: What if I am uncertain about finding a pulse?
A: If you are uncertain about detecting a pulse, it is better to err on the side of caution. Begin CPR immediately if the person is unresponsive and not breathing normally. Early chest compressions can significantly improve the chances of survival, even if the pulse is difficult to detect.
Q: How do advanced life support providers check for a pulse?
A: Advanced life support (ALS) providers use manual pulse detection techniques, such as palpating the carotid or femoral arteries, to check for a pulse. They are trained to assess circulation quickly and accurately. Additionally, ALS providers may utilize advanced tools, such as cardiac monitors or ultrasound devices, to confirm the presence of a pulse and guide further interventions.
Conclusion
Pulse checks during CPR are crucial for assessing the effectiveness of resuscitation efforts and informing subsequent steps. By mastering this skill, responders can ensure timely and accurate interventions, improving the chances of survival in cardiac emergencies. With proper training and practice, anyone can make a significant contribution to saving lives when it matters most.















 Login with Google
Login with Google Login with Facebook
Login with Facebook