When it comes to managing heart rhythm disorders, pacemakers and defibrillators are two life-saving devices that often play a crucial role. While both are designed to address irregularities in the heart's electrical system, they serve distinct purposes. This article explores the key differences between pacemakers and defibrillators, providing insight into their distinct roles in cardiac care and their contributions to enhancing quality of life.
Understanding Pacemakers
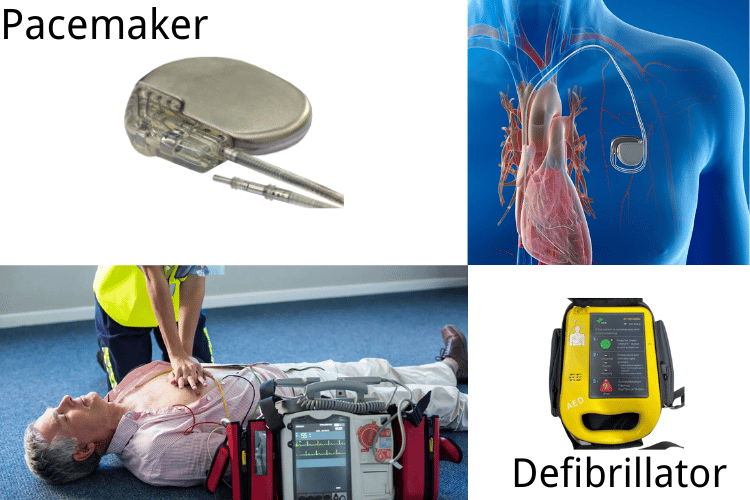
What is a Pacemaker?
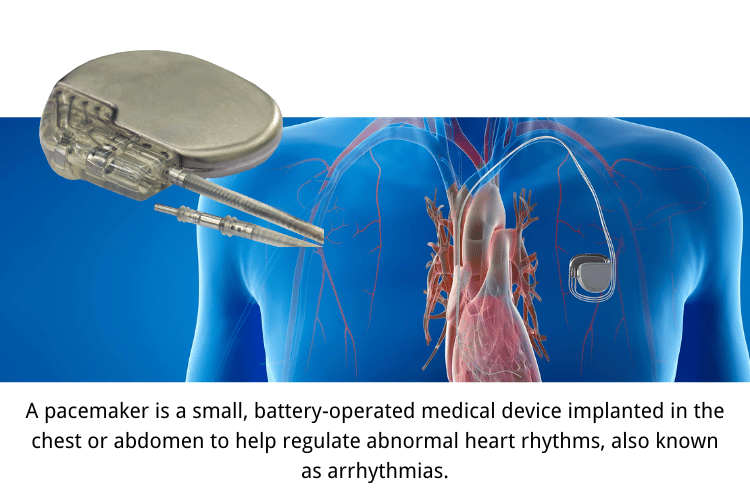 A pacemaker is a small, battery-operated medical device implanted in the chest or abdomen to help regulate abnormal heart rhythms, also known as arrhythmias. It is designed to ensure that the heart beats at a normal and consistent rate, providing the body with an adequate supply of oxygen-rich blood. Pacemakers are typically made up of two main components: a pulse generator, which houses the battery and electrical circuitry, and one or more leads (thin, insulated wires) that connect the device to the heart. These leads deliver electrical impulses to stimulate the heart muscle when it beats too slowly or irregularly.
Pacemakers are often life-saving devices for individuals with conditions that cause bradycardia (a heart rate that is too slow) or other rhythm disturbances. By maintaining a steady heartbeat, pacemakers improve overall heart function, reduce symptoms like fatigue and dizziness, and enhance the quality of life for those with cardiac issues. Modern pacemakers are highly advanced, with some models capable of adjusting heart rates based on physical activity or even transmitting data to healthcare providers for remote monitoring.
A pacemaker is a small, battery-operated medical device implanted in the chest or abdomen to help regulate abnormal heart rhythms, also known as arrhythmias. It is designed to ensure that the heart beats at a normal and consistent rate, providing the body with an adequate supply of oxygen-rich blood. Pacemakers are typically made up of two main components: a pulse generator, which houses the battery and electrical circuitry, and one or more leads (thin, insulated wires) that connect the device to the heart. These leads deliver electrical impulses to stimulate the heart muscle when it beats too slowly or irregularly.
Pacemakers are often life-saving devices for individuals with conditions that cause bradycardia (a heart rate that is too slow) or other rhythm disturbances. By maintaining a steady heartbeat, pacemakers improve overall heart function, reduce symptoms like fatigue and dizziness, and enhance the quality of life for those with cardiac issues. Modern pacemakers are highly advanced, with some models capable of adjusting heart rates based on physical activity or even transmitting data to healthcare providers for remote monitoring.
How Pacemakers Work
Pacemakers function by sending small electrical impulses to the heart muscle to prompt it to contract and produce a heartbeat. The device continuously monitors the heart's natural rhythm and activates only when it detects an irregularity. For example, if the heart rate drops below a pre-set threshold, the pacemaker will deliver an electrical signal to restore a normal rhythm. This process is seamless and typically goes unnoticed by the individual. The leads of the pacemaker are strategically placed in specific chambers of the heart, depending on the type of arrhythmia being treated. For instance, in cases of bradycardia, the leads may be positioned in the right atrium or right ventricle to stimulate these areas. Some pacemakers, known as dual-chamber devices, can coordinate the activity of both the atria and ventricles to mimic the heart's natural rhythm more closely. Additionally, advanced pacemakers, such as biventricular devices, are used in patients with heart failure to synchronize the contractions of the left and right ventricles, improving the heart's pumping efficiency. Modern pacemakers are also equipped with features like rate responsiveness, which adjusts the pacing rate based on the individual's activity level. For example, during exercise, the pacemaker increases the heart rate to meet the body's higher demand for oxygen. Healthcare professionals program these devices to suit the specific needs of each patient, ensuring optimal performance and safety.Indications for Getting a Pacemaker
Pacemakers are recommended for individuals with certain heart conditions that affect the heart's ability to maintain a normal rhythm. Some of the most common indications for pacemaker implantation include:- Bradycardia: A slow heart rate, typically below 60 beats per minute, can cause symptoms like fatigue, dizziness, fainting, and shortness of breath. Pacemakers help regulate the heart rate, ensuring it stays within a healthy range.
- Heart Block: This condition occurs when the electrical signals that control the heartbeat are delayed or blocked as they travel through the heart. Depending on the severity, a pacemaker may be needed to bypass the blockage and restore normal electrical conduction.
- Atrial Fibrillation with Slow Ventricular Response: In some cases of atrial fibrillation, the heart's ventricles may beat too slowly, leading to inadequate blood circulation. A pacemaker can help maintain an appropriate ventricular rate.
- Heart Failure: Patients with heart failure and reduced ejection fraction may benefit from a biventricular pacemaker, which improves the coordination of the heart's pumping action and enhances overall cardiac function.
- Syncope (Fainting): Unexplained fainting episodes caused by irregular heart rhythms may warrant the use of a pacemaker to prevent future occurrences.
- Congenital Heart Conditions: Some individuals are born with structural or electrical abnormalities in the heart that necessitate the use of a pacemaker to maintain a stable rhythm.
- Post-Surgical Complications: Certain heart surgeries, such as valve replacements, can disrupt the heart's electrical system, necessitating the use of a pacemaker.
- Medication-Induced Arrhythmias: Some medications used to treat other conditions can cause an excessively slow heart rate. A pacemaker may be implanted to counteract this side effect while allowing the patient to continue necessary treatments.
Understanding Defibrillators
What is a Defibrillator?
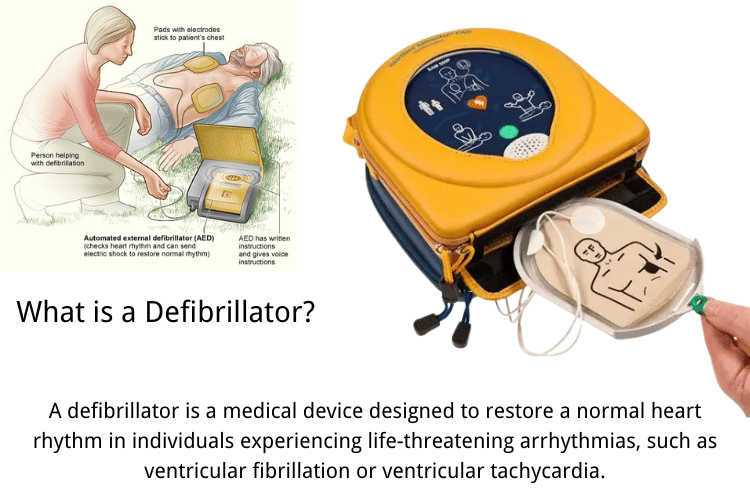 A defibrillator is a medical device designed to restore a normal heart rhythm in individuals experiencing life-threatening arrhythmias, such as ventricular fibrillation or ventricular tachycardia. These conditions disrupt the heart's ability to pump blood effectively, leading to a significant risk of cardiac arrest. Defibrillators deliver a controlled electrical shock to the heart, which helps reset its electrical system and allows it to resume a regular rhythm.
Defibrillators come in various forms, including external devices like automated external defibrillators (AEDs) and implantable devices such as implantable cardioverter defibrillators (ICDs). AEDs are commonly found in public spaces and are designed for use by laypersons during emergencies, while ICDs are surgically implanted in patients at high risk of sudden cardiac arrest. Both types of defibrillators play a critical role in saving lives by intervening during cardiac emergencies.
A defibrillator is a medical device designed to restore a normal heart rhythm in individuals experiencing life-threatening arrhythmias, such as ventricular fibrillation or ventricular tachycardia. These conditions disrupt the heart's ability to pump blood effectively, leading to a significant risk of cardiac arrest. Defibrillators deliver a controlled electrical shock to the heart, which helps reset its electrical system and allows it to resume a regular rhythm.
Defibrillators come in various forms, including external devices like automated external defibrillators (AEDs) and implantable devices such as implantable cardioverter defibrillators (ICDs). AEDs are commonly found in public spaces and are designed for use by laypersons during emergencies, while ICDs are surgically implanted in patients at high risk of sudden cardiac arrest. Both types of defibrillators play a critical role in saving lives by intervening during cardiac emergencies.
How Defibrillators Work
Defibrillators function by delivering an electrical shock to the heart to interrupt abnormal electrical activity and restore a normal rhythm. The process begins with the device detecting irregular heart rhythms through sensors or leads. Once an arrhythmia is identified, the defibrillator determines whether a shock is necessary based on the severity and type of rhythm disturbance.- Detection of Abnormal Rhythms: Implantable defibrillators, such as ICDs, continuously monitor the heart's electrical activity through leads placed in the heart. External devices like AEDs use adhesive pads to detect the heart's rhythm when applied to the chest. Both types analyze the rhythm to determine if it is life-threatening.
- Delivery of Electrical Shock: If the device identifies a dangerous arrhythmia, it delivers a high-energy shock to the heart. This shock depolarizes the heart's electrical system, effectively "resetting" it and allowing the natural pacemaker to regain control. The shock is carefully calibrated to minimize damage to the heart while maximizing the chances of restoring a normal rhythm.
- Post-Shock Monitoring: After delivering a shock, the defibrillator continues to monitor the heart to ensure the rhythm has stabilized. If the arrhythmia persists, the device may deliver additional shocks or switch to alternative therapies, such as anti-tachycardia pacing, which utilizes rapid, low-energy pulses to restore the rhythm.
Indications for Defibrillator Implant
Implantable defibrillators, such as ICDs, are recommended for individuals at high risk of sudden cardiac arrest or those with a history of life-threatening arrhythmias. The decision to implant a defibrillator is based on a thorough evaluation of the patient's medical history, heart function, and overall health. Common indications include:- Survivors of Sudden Cardiac Arrest: Patients who have experienced a cardiac arrest due to ventricular fibrillation or ventricular tachycardia are prime candidates for an ICD. The device helps prevent future episodes by intervening promptly during arrhythmias.
- Severe Ventricular Arrhythmias: Individuals with recurrent episodes of ventricular tachycardia or fibrillation, which do not respond to medication or other treatments, may benefit from a defibrillator implant.
- Heart Failure with Reduced Ejection Fraction: Patients with heart failure and a significantly reduced ejection fraction (typically below 35%) are at increased risk of sudden cardiac arrest. An ICD can provide life-saving protection in these cases.
- Inherited Cardiac Conditions: Certain genetic disorders, such as long QT syndrome, Brugada syndrome, or hypertrophic cardiomyopathy, increase the risk of dangerous arrhythmias. A defibrillator may be implanted as a preventive measure.
- Post-Heart Attack Patients: Individuals who have suffered a heart attack and have residual damage to the heart muscle are at higher risk of arrhythmias. An ICD can help manage this risk and improve long-term outcomes.
- Cardiac Sarcoidosis or Myocarditis: Inflammatory conditions affecting the heart can lead to scarring and arrhythmias. A defibrillator may be recommended for patients with these conditions who are at risk of sudden cardiac events.
- Primary Prevention in High-Risk Groups: In some cases, defibrillators are implanted as a preventive measure in patients with no history of arrhythmias but who are deemed high-risk based on their medical profile and diagnostic tests.
Pacemakers vs. Defibrillators
The Difference Between a Pacemaker and a Defibrillator
While both pacemakers and defibrillators are medical devices designed to manage heart rhythm disorders, they serve distinct purposes and address different types of cardiac issues. Understanding their differences is crucial for determining the most suitable treatment for specific heart conditions. A pacemaker is primarily used to regulate slow or irregular heart rhythms, such as bradycardia. It works by sending small electrical impulses to the heart to maintain a steady and consistent heartbeat. Pacemakers are typically implanted in patients whose natural heart rhythm is too slow or irregular to meet the body’s needs. They are also used in cases of heart block, where the electrical signals between the heart's chambers are delayed or interrupted. On the other hand, a defibrillator, specifically an implantable cardioverter defibrillator (ICD), is designed to prevent sudden cardiac arrest caused by life-threatening arrhythmias like ventricular fibrillation or ventricular tachycardia. Unlike pacemakers, defibrillators deliver high-energy shocks to reset the heart's rhythm when it becomes dangerously fast or chaotic. ICDs also have the capability to function as pacemakers if the heart rate becomes too slow, making them versatile devices for managing complex rhythm disorders. In summary, pacemakers are used to correct slow or irregular rhythms, while defibrillators are life-saving devices that intervene during rapid or chaotic arrhythmias. Both devices play critical roles in heart rhythm management but are tailored to address different cardiac conditions.When to Choose a Pacemaker or an ICD
The decision to implant a pacemaker or an ICD depends on the specific heart condition and the patient’s overall health. Here are some scenarios to help clarify when each device is recommended:- Pacemaker Indications:
- Bradycardia: A pacemaker is ideal for patients with a slow heart rate that causes symptoms like fatigue, dizziness, or fainting.
- Heart Block: When electrical signals between the heart's chambers are delayed or blocked, a pacemaker ensures proper coordination of the heart's contractions.
- Atrial Fibrillation with Slow Ventricular Response: In some cases, a pacemaker is used to maintain an adequate heart rate in patients with atrial fibrillation.
- Post-Surgical Complications: After certain heart surgeries, a pacemaker may be needed to stabilize the heart's rhythm.
- ICD Indications:
- Survivors of Sudden Cardiac Arrest: Patients who have experienced cardiac arrest due to ventricular fibrillation or tachycardia benefit from an ICD to prevent future episodes.
- Severe Ventricular Arrhythmias: ICDs are recommended for individuals with recurrent, life-threatening arrhythmias that do not respond to medication.
- Heart Failure with Reduced Ejection Fraction: Patients with heart failure and a low ejection fraction are at high risk of sudden cardiac arrest and may require an ICD.
- Inherited Cardiac Conditions: Genetic disorders like long QT syndrome or hypertrophic cardiomyopathy often necessitate an ICD for preventive care.
- Primary Prevention in High-Risk Patients: ICDs are sometimes implanted in patients with no history of arrhythmias but who are at high risk based on diagnostic tests and medical history.
Heart Rhythm Management: Pacemakers and Implantable Defibrillators
Both pacemakers and ICDs are integral to managing heart rhythm disorders, but their roles in treatment differ significantly. Pacemakers focus on maintaining a steady heart rate, ensuring that the heart pumps blood efficiently to meet the body’s needs. They are particularly effective for conditions that cause the heart to beat too slowly or irregularly, such as bradycardia or heart block. ICDs, however, are designed to address the opposite end of the spectrum—dangerously fast or chaotic heart rhythms that can lead to sudden cardiac arrest. By delivering a high-energy shock, ICDs reset the heart’s electrical system and restore a normal rhythm. This life-saving intervention is critical for patients with ventricular arrhythmias or those at high risk of cardiac arrest. Both devices are implanted under the skin, typically near the collarbone, and connected to the heart via leads. They are programmed by healthcare professionals to meet the specific needs of each patient, ensuring optimal performance. Modern devices are also equipped with advanced features, such as remote monitoring, which allows doctors to track the device’s performance and the patient’s heart activity in real time. In conclusion, pacemakers and defibrillators are complementary tools in the management of heart rhythm disorders. While pacemakers provide long-term support for slow or irregular rhythms, ICDs offer immediate protection against life-threatening arrhythmias. The choice between the two depends on the patient’s condition, risk factors, and overall treatment goals, with both devices playing a vital role in improving quality of life and preventing cardiac emergencies.Implantable Cardioverter Defibrillators (ICDs)
What is an Implantable Cardioverter Defibrillator?
An Implantable Cardioverter Defibrillator (ICD) is a small, life-saving medical device designed to monitor and correct dangerous heart rhythms, particularly those that can lead to sudden cardiac arrest. Unlike external defibrillators, which are used in emergencies by bystanders or medical professionals, ICDs are surgically implanted under the skin, typically near the collarbone, and provide continuous monitoring of the heart's electrical activity. ICDs are primarily used to treat ventricular arrhythmias, such as ventricular tachycardia and ventricular fibrillation, which can disrupt the heart's ability to pump blood effectively. These conditions are often life-threatening, as they can cause the heart to stop beating entirely. By delivering a controlled electrical shock, the ICD restores a normal rhythm and prevents cardiac arrest. In addition to their defibrillation capabilities, many ICDs also function as pacemakers, addressing slower heart rhythms when necessary.How ICDs Function
ICDs operate by continuously monitoring the heart's electrical signals through leads that are connected to the heart. These leads detect any irregularities in the rhythm and send the information to the device's pulse generator, which analyzes the data and determines whether intervention is needed. Here’s a breakdown of how ICDs work:- Monitoring Heart Rhythms: The ICD constantly tracks the heart's electrical activity, looking for signs of arrhythmias. It can differentiate between normal variations in heart rate, such as those caused by exercise or stress, and dangerous rhythms that require correction.
- Detecting Arrhythmias: When the ICD identifies a life-threatening arrhythmia, such as ventricular fibrillation, it quickly assesses the severity and determines the appropriate response. The device is programmed to recognize specific thresholds for intervention, ensuring it only activates when necessary.
- Delivering Therapy:
- Anti-Tachycardia Pacing (ATP): For less severe arrhythmias, the ICD may deliver a series of rapid, low-energy electrical pulses to interrupt the abnormal rhythm and restore a normal heartbeat.
- Defibrillation Shock: For more severe arrhythmias, the ICD delivers a high-energy shock to reset the heart's electrical system. This shock is often described as a sudden jolt and is powerful enough to stop chaotic electrical activity and allow the heart to resume a normal rhythm.
- Post-Therapy Monitoring: After delivering therapy, the ICD continues to monitor the heart to ensure the rhythm has stabilized. If the arrhythmia persists or recurs, the device may deliver additional shocks or adjust its pacing settings.
ICD vs. Pacemaker: Key Differences
While both ICDs and pacemakers are implantable devices used to manage heart rhythm disorders, they serve distinct purposes and are designed to address different types of cardiac issues. Understanding their differences is essential for determining the appropriate treatment.- Primary Function:
- ICD: The primary role of an ICD is to prevent sudden cardiac arrest by detecting and treating life-threatening arrhythmias, such as ventricular fibrillation and ventricular tachycardia. It delivers high-energy shocks or rapid pacing to restore a normal rhythm.
- Pacemaker: A pacemaker is designed to regulate slow or irregular heart rhythms, such as bradycardia. It sends low-energy electrical impulses to maintain a steady and consistent heartbeat.
- Targeted Conditions:
- ICD: Used for patients at high risk of sudden cardiac arrest, often due to conditions like heart failure, previous cardiac arrest, or inherited arrhythmias.
- Pacemaker: Recommended for individuals with conditions that cause the heart to beat too slowly or irregularly, such as heart block or sick sinus syndrome.
- Energy Levels:
- ICD: Capable of delivering both low-energy pacing and high-energy shocks to address a wide range of arrhythmias.
- Pacemaker: Delivers only low-energy electrical impulses to correct slow or irregular rhythms.
- Monitoring and Intervention:
- ICD: Continuously monitors the heart for dangerous arrhythmias and intervenes only when necessary. It is both a monitoring and therapeutic device.
- Pacemaker: Primarily focuses on maintaining a consistent heart rate and does not deliver high-energy shocks.
- Patient Population:
- ICD: Typically implanted in patients with a history of or high risk for life-threatening arrhythmias.
- Pacemaker: Used for patients with non-life-threatening rhythm disorders that affect the heart's ability to pump blood efficiently.
- Combination Devices: Some devices, such as CRT-D (Cardiac Resynchronization Therapy with Defibrillator), combine the functions of an ICD and a pacemaker. These are often used in patients with heart failure who require both rhythm regulation and protection against sudden cardiac arrest.
Conclusion
Summary of Pacemakers and Defibrillators
Pacemakers and defibrillators are two essential medical devices that play a critical role in managing heart rhythm disorders. While both are designed to address irregularities in the heart's electrical system, their functions and applications differ significantly. Pacemakers are primarily used to regulate slow or irregular heart rhythms, ensuring the heart beats at a steady and consistent rate. They are ideal for conditions like bradycardia or heart block, where the heart's natural rhythm is too slow or disrupted. On the other hand, defibrillators, particularly implantable cardioverter defibrillators (ICDs), are life-saving devices that intervene during dangerous arrhythmias, such as ventricular fibrillation or tachycardia, by delivering high-energy shocks to restore a normal rhythm. Both devices are highly advanced, with features like remote monitoring and dual functionality in some cases, such as CRT-D devices that combine the benefits of a pacemaker and an ICD. Together, these technologies have revolutionized the treatment of cardiac conditions, improving survival rates and enhancing the quality of life for millions of patients worldwide.Making an Informed Decision
Choosing between a pacemaker and a defibrillator—or deciding to opt for a combination device—requires a thorough evaluation of the patient’s specific condition, medical history, and risk factors. This decision is typically made in consultation with a cardiologist, who will assess the heart's electrical activity through diagnostic tests like electrocardiograms (ECGs), Holter monitoring, and stress tests. Factors such as the type and severity of arrhythmia, the presence of underlying conditions like heart failure, and the patient’s overall health are all taken into account. Patients should also consider the lifestyle implications of these devices, including the need for regular follow-ups, potential restrictions on certain activities, and the psychological adjustment to living with an implanted device. Open communication with healthcare providers is crucial to understanding the benefits, risks, and long-term management of these devices. By staying informed and actively participating in the decision-making process, patients can select the most suitable treatment option for their specific needs.Future of Heart Rhythm Devices
The future of heart rhythm management is promising, with ongoing advancements in technology paving the way for more effective and patient-friendly devices. Innovations in miniaturization are making pacemakers and defibrillators smaller and less invasive, thereby reducing recovery times and improving patient comfort. Wireless and leadless pacemakers, which eliminate the need for traditional leads, are already transforming the field by reducing complications associated with lead placement. Additionally, the integration of artificial intelligence (AI) and machine learning into these devices is enhancing their ability to predict and respond to arrhythmias more accurately. AI-powered algorithms can analyze vast amounts of data from the device and the patient’s medical history to provide personalized therapy and early warnings of potential issues. Remote monitoring capabilities are also becoming increasingly sophisticated, enabling healthcare providers to track device performance and patient health in real-time, resulting in more proactive and efficient care. Furthermore, research into bioengineered solutions, such as tissue-based pacemakers, holds the potential to replace electronic devices with biological alternatives that mimic the heart's natural rhythm. These developments, along with improvements in battery life and energy efficiency, are poised to redefine the landscape of cardiac care, providing patients with safer, more effective, and less invasive options for managing heart rhythm disorders.Frequently Asked Questions
Q: What is a pacemaker?
A: A pacemaker is a small, battery-powered device implanted under the skin, typically in the chest or abdomen, to help regulate the heart's rhythm. It sends electrical impulses to the heart muscle to maintain a steady and normal heartbeat, particularly for individuals with bradycardia (a slow heart rate) or irregular heart rhythms.
Q: What is a defibrillator?
A: A defibrillator is a medical device designed to treat life-threatening arrhythmias or sudden cardiac arrest. It works by delivering an electrical shock to the heart, which helps reset the heart's rhythm and restore a normal heartbeat when necessary.
Q: How do pacemakers and defibrillators differ?
A: While both devices manage heart rhythm issues, their purposes differ. A pacemaker primarily addresses slow or irregular heartbeats by sending electrical signals to maintain a steady rhythm. A defibrillator, on the other hand, is used in critical situations, such as ventricular fibrillation, to deliver a high-energy shock and correct dangerous arrhythmias.
Q: When might someone need a pacemaker?
A: A pacemaker may be needed if someone experiences symptoms like fatigue, dizziness, or fainting due to a slow or irregular heartbeat. Conditions such as heart block or arrhythmias that disrupt the heart's electrical signals often lead to the need for a pacemaker.
Q: Can defibrillators be implanted like pacemakers?
A: Yes, implantable cardioverter defibrillators (ICDs) are implanted under the skin in a manner similar to pacemakers. These devices monitor the heart's rhythm and deliver shocks to correct life-threatening arrhythmias, making them essential for individuals at high risk of sudden cardiac arrest.
Q: What is a biventricular pacemaker?
A: A biventricular pacemaker is a specialized device used in cardiac resynchronization therapy (CRT). It paces both the right and left ventricles of the heart to improve coordination and efficiency, particularly in patients with heart failure and irregular heart rhythms.
Q: What are the benefits of an implantable defibrillator?
A: Implantable defibrillators offer life-saving benefits for individuals with a history of dangerous arrhythmias. They continuously monitor the heart's rhythm and deliver shocks when needed, preventing sudden cardiac arrest and providing reassurance for both patients and their families.
Q: How do I know if I need a defibrillator?
A: Your doctor may recommend an ICD if you have experienced life-threatening arrhythmias, have a family history of sudden cardiac arrest, or have heart conditions that increase your risk. Diagnostic tests, such as ECGs or Holter monitoring, will help determine whether a defibrillator is necessary.
Q: Can someone have both a pacemaker and a defibrillator?
A: Yes, some patients require both a pacemaker and an ICD. This combination is often used for individuals with complex heart conditions, where the pacemaker regulates slow heart rates and the defibrillator addresses life-threatening arrhythmias.
Conclusion
Pacemakers and defibrillators are essential tools in modern cardiac care, each tailored to address specific heart rhythm issues. Pacemakers focus on maintaining a steady heartbeat, while defibrillators are life-saving devices that intervene during critical arrhythmias. Understanding their differences and applications can empower patients and caregivers to make informed decisions about heart health. With advancements in technology, these devices continue to revolutionize the management of heart rhythm disorders, offering hope and improved outcomes for millions worldwide.















 Login with Google
Login with Google Login with Facebook
Login with Facebook