Pulseless Electrical Activity (PEA) is a critical condition where the heart's electrical system remains active, but the heart fails to pump blood effectively. This article explores the causes, distinctions, and management of PEA, emphasizing the importance of timely intervention and understanding its reversible factors. Dive in to learn how healthcare providers address this life-threatening condition and improve patient outcomes.
Understanding Pulseless Electrical Activity (PEA)
Definition of Pulseless Electrical Activity
Pulseless Electrical Activity (PEA) is a medical condition in which the heart's electrical system continues to generate activity, but the heart muscle fails to contract effectively, resulting in no detectable pulse or blood circulation. Despite the presence of electrical signals, the heart is unable to pump blood to the body, leading to a state of cardiac arrest. PEA is not a specific disease but rather a clinical state that can result from various underlying causes, such as severe hypoxia, acidosis, or significant blood loss. PEA is considered a "non-shockable rhythm," meaning it cannot be treated with defibrillation. Instead, the focus of treatment is on identifying and addressing the root cause of the condition while providing high-quality cardiopulmonary resuscitation (CPR) to maintain blood flow to vital organs. Early recognition and intervention are critical, as PEA is often reversible if the underlying issue is promptly corrected.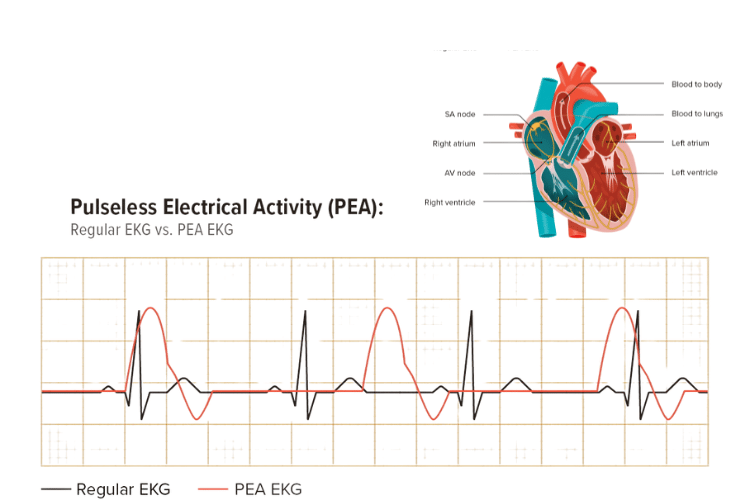
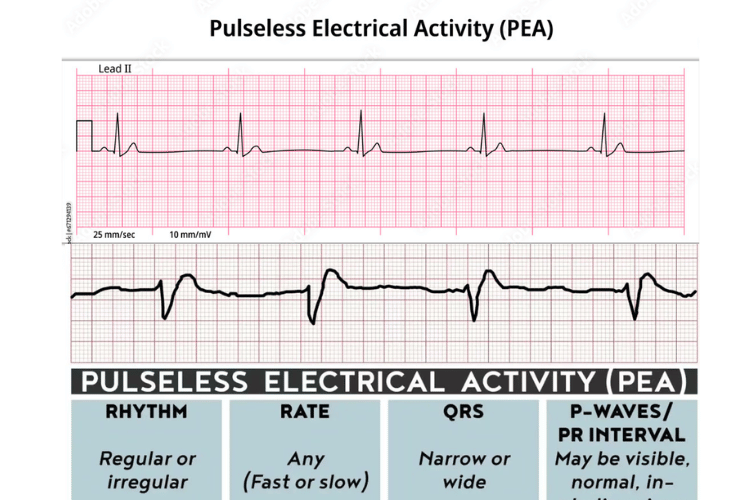
Regular EKG and PEA EKG
Distinction Between PEA and Asystole
While both PEA and asystole are forms of cardiac arrest, they differ significantly in terms of their underlying mechanisms and treatment approaches. Understanding these differences is crucial for effective management during emergencies.- Presence of Electrical Activity:
- PEA: In PEA, the heart's electrical system is active, and an organized rhythm can be observed on an electrocardiogram (ECG). However, this electrical activity does not result in effective heart contractions or a palpable pulse.
- Asystole: Asystole, often referred to as "flatline," is characterized by the complete absence of electrical activity in the heart. The ECG shows a flat or nearly flat line, indicating no rhythm or electrical signals.
- Treatment Options:
- PEA: Since PEA is a non-shockable rhythm, defibrillation is not effective. Treatment focuses on high-quality CPR, administering medications like epinephrine, and identifying and treating reversible causes (e.g., hypoxia, hypovolemia, or tension pneumothorax).
- Asystole: Like PEA, asystole is also non-shockable. The primary interventions include CPR, epinephrine administration, and addressing potential reversible factors. However, the prognosis for asystole is generally poorer compared to PEA.
- Prognosis:
- PEA: The prognosis for PEA depends on the underlying cause and how quickly it is identified and treated. Reversible causes, such as electrolyte imbalances or cardiac tamponade, can improve outcomes if addressed promptly.
- Asystole: Asystole often indicates a more severe and prolonged cardiac arrest, with a lower likelihood of successful resuscitation.
Electrical Activity in Cardiac Arrest
Cardiac arrest is a condition in which the heart suddenly stops pumping blood, leading to a loss of circulation and oxygen delivery to the body. Electrical activity plays a central role in cardiac arrest, as it determines the type of rhythm present and guides treatment decisions. There are two main categories of rhythms in cardiac arrest: shockable and non-shockable.- Shockable Rhythms:
- These include ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT). In these cases, the heart's electrical activity is chaotic or excessively rapid, preventing effective contractions. Defibrillation is the primary treatment to reset the heart's electrical system and restore a normal rhythm.
- Non-Shockable Rhythms:
- These include PEA and asystole. In PEA, the electrical activity appears organized, but the heart muscle fails to contract. In asystole, there is no electrical activity at all. For both rhythms, defibrillation is not effective, and treatment focuses on CPR, medications, and addressing reversible causes.
Causes of Pulseless Electrical Activity (PEA)
Common Etiologies of PEA
Pulseless Electrical Activity (PEA) is not a standalone condition but rather a clinical state that arises from various underlying causes. It occurs when the heart's electrical system is active, but the mechanical function of the heart is impaired, resulting in no effective blood circulation. The most common etiologies of PEA include conditions that disrupt the heart's ability to pump blood effectively or compromise the body's overall physiology.- Hypovolemia: Severe blood or fluid loss reduces the volume available for the heart to pump, leading to inadequate circulation despite electrical activity. This is a frequent cause of PEA in trauma or dehydration cases.
- Hypoxia: A lack of oxygen in the blood can impair the heart muscle's ability to contract, resulting in PEA. This is often seen in respiratory failure or airway obstruction.
- Acidosis: Metabolic or respiratory acidosis, where the blood becomes too acidic, can interfere with the heart's function and lead to PEA.
- Cardiac Tamponade: Fluid accumulation in the pericardial sac compresses the heart, preventing it from filling and pumping effectively.
- Tension Pneumothorax: A collapsed lung with increased pressure in the chest cavity can compress the heart and major blood vessels, leading to circulatory failure.
- Massive Pulmonary Embolism: A large blood clot in the lungs can obstruct blood flow, causing PEA.
- Hyperkalemia or Hypokalemia: Abnormal potassium levels can disrupt the heart's electrical activity and mechanical function.
- Hypothermia: Extremely low body temperatures can slow the heart's activity and lead to PEA.
- Drug Overdose or Toxicity: Certain medications or toxins, such as beta-blockers, calcium channel blockers, or opioids, can depress cardiac function and result in PEA.
Risk Factors for Adult In-Hospital Cardiac Arrest
In-hospital cardiac arrests, including those presenting as PEA, are often associated with specific risk factors that predispose patients to this critical condition. Understanding these risk factors can help healthcare providers identify at-risk individuals and implement preventive measures.- Severe Illness or Organ Failure: Patients with advanced heart failure, respiratory failure, or multi-organ dysfunction are at higher risk of developing PEA due to the strain on their cardiovascular system.
- Sepsis: Severe infections can lead to systemic inflammation, acidosis, and hypoperfusion, all of which increase the likelihood of PEA.
- Post-Surgical Complications: Patients recovering from major surgeries, particularly cardiac or thoracic procedures, may experience complications like tamponade or embolism that can result in PEA.
- Electrolyte Imbalances: Hospitalized patients, especially those on diuretics or receiving intravenous fluids, are prone to imbalances in potassium, calcium, or magnesium, which can disrupt cardiac function.
- Respiratory Compromise: Conditions like acute respiratory distress syndrome (ARDS), airway obstruction, or prolonged mechanical ventilation can lead to hypoxia and subsequent PEA.
- Medication Effects: High doses of sedatives, anesthetics, or cardiovascular drugs can depress the heart's function and contribute to PEA.
- Advanced Age: Older adults are more likely to have underlying chronic conditions and reduced physiological reserves, making them more susceptible to cardiac arrest.
Identifying Reversible Causes of PEA
The key to managing PEA lies in identifying and treating its reversible causes, often referred to as the "H’s and T’s." These are common, treatable conditions that can lead to PEA if not addressed promptly. Here’s a breakdown of these causes:The H’s:
- Hypovolemia: Treat with rapid fluid resuscitation or blood transfusion to restore circulating volume.
- Hypoxia: Ensure adequate oxygenation through airway management and ventilation.
- Hydrogen Ion (Acidosis): Correct metabolic acidosis with sodium bicarbonate and address the underlying cause.
- Hyperkalemia or Hypokalemia: Administer calcium, insulin, or glucose for hyperkalemia, and replace potassium for hypokalemia.
- Hypothermia: Gradually rewarm the patient using external or internal warming techniques.
The T’s:
- Tension Pneumothorax: Perform needle decompression or chest tube placement to relieve pressure.
- Tamponade (Cardiac): Conduct pericardiocentesis to remove fluid from the pericardial sac.
- Toxins: Administer specific antidotes or supportive care for drug overdoses or poisoning.
- Thrombosis (Pulmonary or Coronary): Treat pulmonary embolism with thrombolytics or coronary thrombosis with percutaneous coronary intervention (PCI).
- Trauma: Address traumatic injuries, such as internal bleeding or chest trauma, with surgical intervention or other appropriate measures.
Management of Pulseless Electrical Activity (PEA)
Initial Assessment and Immediate Actions
The management of Pulseless Electrical Activity (PEA) begins with a rapid and systematic assessment to identify the underlying cause and initiate life-saving interventions. Time is critical, as PEA represents a state of cardiac arrest where the heart's electrical activity is present, but there is no effective blood circulation. The first step is to confirm the absence of a pulse despite the presence of an organized rhythm on the electrocardiogram (ECG). This ensures that the condition is indeed PEA and not another form of cardiac arrest. Once PEA is identified, high-quality cardiopulmonary resuscitation (CPR) must be initiated immediately. CPR ensures that oxygenated blood continues to flow to vital organs, particularly the brain and heart, while the underlying cause is being addressed. Chest compressions should be performed at a rate of 100–120 compressions per minute, with minimal interruptions. Simultaneously, the airway should be secured, and ventilation provided using a bag-valve mask or advanced airway device to maintain oxygenation. During this initial phase, it is also essential to establish intravenous (IV) or intraosseous (IO) access to administer medications. Epinephrine is the drug of choice and should be given every 3–5 minutes to improve coronary and cerebral perfusion. While these immediate actions are underway, the healthcare team should begin evaluating potential reversible causes of PEA, often referred to as the "H’s and T’s," to guide further treatment.Advanced Cardiac Life Support (ACLS) Protocols
The Advanced Cardiac Life Support (ACLS) guidelines provide a structured approach to managing PEA and other forms of cardiac arrest. These protocols emphasize the importance of high-quality CPR, timely administration of medications, and the identification of reversible causes. Here are the key components of ACLS management for PEA:- High-Quality CPR:
- Ensure chest compressions are deep (at least 2 inches) and at the correct rate (100–120 per minute).
- Minimize interruptions in compressions to maintain consistent blood flow.
- Rotate rescuers every 2 minutes to prevent fatigue and maintain compression quality.
- Airway and Ventilation:
- Secure the airway using a bag-valve mask or advanced airway device, such as an endotracheal tube.
- Provide ventilation at a rate of 1 breath every 6 seconds (10 breaths per minute) to avoid hyperventilation, which can reduce cardiac output.
- Medication Administration:
- Administer epinephrine (1 mg IV/IO) every 3–5 minutes during resuscitation.
- Avoid defibrillation, as PEA is a non-shockable rhythm.
- Identify and Treat Reversible Causes:
- Systematically evaluate the "H’s and T’s" (e.g., hypovolemia, hypoxia, tension pneumothorax, tamponade, toxins) to address the root cause of PEA.
- Use diagnostic tools like ultrasound, blood gas analysis, or chest X-rays to confirm suspected causes.
- Team Coordination:
- Effective communication and role delegation among the resuscitation team are critical for ensuring that all aspects of care are addressed promptly.
Post-Resuscitation Care Strategies
Once ROSC is achieved, the focus shifts to post-resuscitation care to stabilize the patient, prevent further complications, and optimize long-term outcomes. This phase is critical, as patients who survive PEA are often at risk of recurrent cardiac arrest, organ dysfunction, and neurological impairment. Post-resuscitation care involves a multidisciplinary approach that addresses hemodynamic stability, oxygenation, and neurological recovery.- Hemodynamic Support:
- Monitor blood pressure and cardiac output closely, and use vasopressors or inotropes as needed to maintain adequate perfusion.
- Correct any underlying issues, such as fluid deficits or electrolyte imbalances, to stabilize the cardiovascular system.
- Oxygenation and Ventilation:
- Ensure the patient is adequately oxygenated, with a target oxygen saturation of 94–98%.
- Avoid hyperoxia, as excessive oxygen levels can lead to oxidative stress and worsen outcomes.
- If the patient remains intubated, adjust ventilation settings to maintain normal carbon dioxide levels and prevent respiratory acidosis or alkalosis.
- Neurological Monitoring and Care:
- Assess the patient’s neurological status using tools like the Glasgow Coma Scale (GCS).
- Consider targeted temperature management (TTM) for comatose patients to reduce the risk of brain injury. TTM involves maintaining the patient’s body temperature between 32–36°C for 24–48 hours.
- Diagnostic Evaluation:
- Perform a thorough evaluation to identify the cause of the cardiac arrest and guide further treatment. This may include imaging studies, blood tests, and cardiac catheterization if a coronary event is suspected.
- Long-Term Planning:
- Develop a comprehensive care plan that includes follow-up with cardiology, rehabilitation services, and lifestyle modifications to reduce the risk of future cardiac events.
- Educate the patient and their family about the importance of medication adherence, dietary changes, and regular medical check-ups.
PEA and Asystole: Clinical Implications
Outcomes for Patients with PEA
Pulseless Electrical Activity (PEA) is a critical condition that represents a form of cardiac arrest where the heart's electrical system is active, but there is no effective mechanical contraction or blood circulation. The outcomes for patients with PEA largely depend on the underlying cause, the timeliness of intervention, and the quality of resuscitation efforts. Unlike shockable rhythms such as ventricular fibrillation, PEA is considered a non-shockable rhythm, meaning defibrillation is not effective. Instead, treatment focuses on high-quality cardiopulmonary resuscitation (CPR), administration of medications like epinephrine, and identifying reversible causes. Patients with PEA often have better survival rates compared to those with asystole, as PEA is more likely to result from reversible conditions such as hypovolemia, hypoxia, or electrolyte imbalances. However, the prognosis remains guarded, as the condition indicates severe physiological compromise. Early recognition and treatment of the underlying cause are critical to improving outcomes. For example, rapid fluid resuscitation in cases of hypovolemia or immediate needle decompression for tension pneumothorax can significantly increase the chances of survival. Despite these efforts, many patients with PEA do not achieve return of spontaneous circulation (ROSC), and those who do may face challenges such as neurological impairment or organ dysfunction.Comparative Survival Rates: PEA vs. Asystole
When comparing survival rates between PEA and asystole, PEA generally has a more favorable prognosis, though both conditions are associated with high mortality. Asystole, often referred to as "flatline," represents the complete absence of electrical activity in the heart and is considered the most severe form of cardiac arrest. In contrast, PEA involves organized electrical activity without effective mechanical function, which may indicate a potentially reversible cause.- Initial Survival Rates:
- Patients with PEA are more likely to achieve ROSC during resuscitation compared to those with asystole. This is because PEA often results from treatable conditions, such as cardiac tamponade or severe hypoxia, which can be addressed during resuscitation efforts.
- Asystole, on the other hand, is typically associated with prolonged cardiac arrest or irreversible damage, making successful resuscitation less likely.
- Hospital Discharge Rates:
- While PEA has higher rates of ROSC, the percentage of patients who survive to hospital discharge remains low, often below 10–15%. This is due to the severity of the underlying conditions and the potential for multi-organ failure or neurological damage.
- Survival to discharge for asystole is even lower, often less than 5%, reflecting the poor prognosis associated with this rhythm.
- Neurological Outcomes:
- Patients who survive PEA are more likely to have favorable neurological outcomes compared to asystole survivors, particularly if the underlying cause is identified and treated promptly.
- Asystole survivors often face significant neurological impairment due to prolonged periods of inadequate blood flow to the brain.
Long-term Management after Cardiac Arrest
For patients who survive cardiac arrest, whether due to PEA or another rhythm, long-term management is essential to address the underlying cause, prevent recurrence, and optimize recovery. This phase of care involves a multidisciplinary approach that includes cardiology, neurology, and rehabilitation specialists.- Cardiac Monitoring and Treatment:
- Survivors should undergo a thorough evaluation to identify the cause of the cardiac arrest. This may include imaging studies, blood tests, and procedures like coronary angiography if a myocardial infarction is suspected.
- Depending on the findings, patients may require interventions such as coronary stenting, valve repair, or treatment for arrhythmias. Implantable devices like pacemakers or implantable cardioverter defibrillators (ICDs) may be recommended for those at risk of recurrent arrhythmias.
- Neurological Rehabilitation:
- Neurological assessment is critical for survivors, as cardiac arrest often results in hypoxic brain injury. Patients with cognitive or motor impairments may benefit from physical therapy, occupational therapy, and cognitive rehabilitation to regain function and improve quality of life.
- Targeted temperature management (TTM) during the immediate post-resuscitation phase can reduce the risk of severe brain injury and improve long-term neurological outcomes.
- Lifestyle Modifications:
- Patients are encouraged to adopt heart-healthy lifestyle changes, including a balanced diet, regular exercise, and smoking cessation. These measures can reduce the risk of future cardiac events and improve overall health.
- Stress management and mental health support are also important, as many survivors experience anxiety or depression following a cardiac arrest.
- Medication Management:
- Long-term use of medications such as beta-blockers, antiplatelet agents, or anticoagulants may be necessary to manage underlying conditions and prevent recurrence.
- Regular follow-ups with a healthcare provider are essential to monitor the effectiveness of treatment and adjust medications as needed.
- Patient and Family Education:
- Educating patients and their families about recognizing warning signs, such as chest pain or shortness of breath, can help ensure timely medical intervention in the event of a recurrence.
- Families should also be trained in basic life support (BLS) techniques, including CPR, to provide immediate assistance if needed.
Frequently Asked Questions
Q: What is pulseless electrical activity (PEA)?
A: Pulseless electrical activity (PEA) is a critical condition where the heart shows electrical activity on an electrocardiogram (ECG), but the heart muscle fails to contract effectively, resulting in no detectable pulse. PEA often occurs during cardiac arrest and requires immediate recognition and intervention for successful resuscitation.
Q: What are the common causes of pulseless electrical activity?
A: Common causes of pulseless electrical activity include:
- Hypovolemia: Severe blood or fluid loss.
- Cardiac Tamponade: Fluid buildup around the heart.
- Tension Pneumothorax: Collapsed lung causing pressure on the heart.
- Massive Pulmonary Embolism: Blood clot in the lungs.
- Metabolic Disturbances: Issues like acidosis or electrolyte imbalances. Identifying and addressing these causes promptly is essential for effective treatment and improving patient outcomes.
Q: How does pulseless electrical activity differ from ventricular fibrillation?
A: Pulseless electrical activity (PEA) differs from ventricular fibrillation (VF) in both presentation and treatment. PEA shows organized electrical activity on the ECG but no pulse, while VF appears as chaotic, disorganized electrical signals with no effective heart contractions. PEA is treated by addressing underlying causes and performing CPR, whereas VF requires immediate defibrillation.
Q: What is the role of cardiopulmonary resuscitation (CPR) in PEA?
A: Cardiopulmonary resuscitation (CPR) is vital for patients with pulseless electrical activity. It maintains blood flow to critical organs, such as the brain and heart, until advanced treatments can be applied. High-quality CPR, as recommended by the American Heart Association, significantly improves survival rates and outcomes in PEA cases.
Q: How does the initial rhythm affect the treatment of cardiac arrest patients?
A: The initial rhythm observed during cardiac arrest determines the resuscitation strategy. Shockable rhythms, like ventricular fibrillation, require defibrillation, while non-shockable rhythms, such as PEA, demand immediate CPR and a focus on identifying and treating reversible causes. Tailoring treatment to the rhythm type is crucial for effective care.
Q: What is the significance of return of spontaneous circulation (ROSC) in PEA cases?
A: Return of spontaneous circulation (ROSC) is a key goal in resuscitation efforts for PEA patients. It indicates that the heart has resumed effective pumping, restoring blood flow to the body. Achieving ROSC is critical for survival to hospital discharge and is often associated with better long-term outcomes.
Q: Can patients with out-of-hospital cardiac arrest survive with PEA?
A: Yes, survival is possible for patients with out-of-hospital cardiac arrest presenting with PEA, especially when timely and effective CPR is provided. Survival chances improve significantly when reversible causes of PEA, such as hypoxia or hypovolemia, are promptly identified and treated during resuscitation.
Q: What are the survival rates for patients with pulseless electrical activity?
A: Survival rates for PEA patients vary based on factors like the underlying cause, the quality of resuscitation, and the timeliness of intervention. While overall survival rates are lower compared to shockable rhythms, early CPR and advanced resuscitation measures have been shown to improve outcomes in PEA cases.
Q: What is the importance of identifying PEA in out-of-hospital cardiac arrest patients?
A: Identifying pulseless electrical activity in out-of-hospital cardiac arrest is crucial for guiding resuscitation efforts. Recognizing that electrical activity is present despite the absence of a pulse allows responders to focus on CPR and address reversible causes, increasing the likelihood of a successful outcome.
Conclusion
Understanding Pulseless Electrical Activity (PEA) is crucial for effective management of cardiac arrest. By identifying and treating its reversible causes, healthcare providers can significantly improve survival rates and patient recovery. While PEA presents unique challenges, advancements in resuscitation techniques and post-cardiac arrest care continue to enhance outcomes, offering hope for those affected by this critical condition.








 Login with Google
Login with Google Login with Facebook
Login with Facebook