Vagal maneuvers are simple techniques used to stimulate the vagus nerve, which can help regulate heart rate and manage certain medical conditions, such as supraventricular tachycardia (SVT). These non-invasive methods are often recommended as a first-line approach to slow down a rapid heartbeat. In this blog, we’ll explore what vagal maneuvers are, how they work, and when they should be used.
Understanding Supraventricular Tachycardia (SVT)
Supraventricular tachycardia (SVT) is a condition characterized by an abnormally fast heart rhythm originating above the ventricles in the heart. It refers to a group of arrhythmias caused by misfiring electrical signals in the upper chambers of the heart, which can disrupt the heart's ability to pump blood efficiently. While SVT is generally not life-threatening, it can cause discomfort and symptoms such as palpitations, dizziness, or shortness of breath. Episodes of SVT can last from a few seconds to several hours and may occur sporadically or frequently, depending on the individual. Common triggers include stress, caffeine, or physical exertion, though it can also occur without an apparent cause. Prolonged episodes may strain the heart and require medical intervention to restore a normal rhythm. Understanding SVT involves recognizing its symptoms, causes, and potential complications, allowing for effective management of the condition.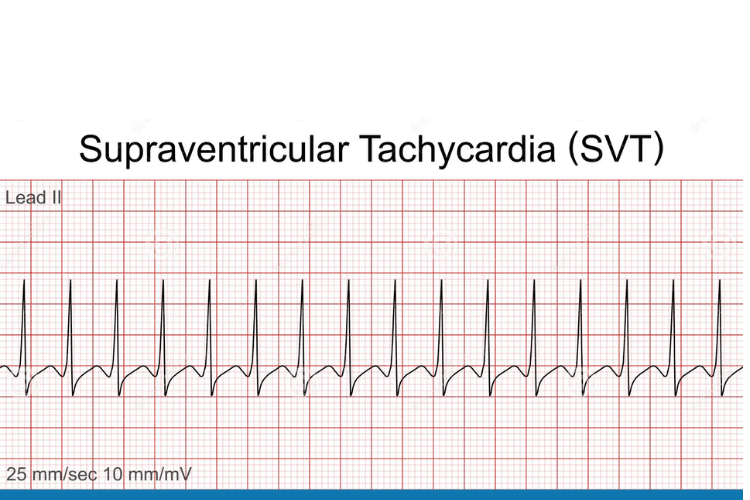
Supraventricular Tachycardia (SVT)
Symptoms of Supraventricular Tachycardia
The symptoms of SVT can vary in intensity and duration, but they typically include a rapid heartbeat, which may feel like a fluttering or pounding sensation in the chest. This is often accompanied by dizziness or lightheadedness, as the heart's inefficiency in pumping blood can reduce oxygen supply to the brain. Some individuals may also experience shortness of breath, chest discomfort, or a feeling of tightness in the chest. In more severe cases, SVT can cause fainting or near-fainting episodes, particularly if the rapid heart rate significantly affects blood flow. Other symptoms may include fatigue, sweating, or a sense of anxiety, as the body reacts to the sudden increase in heart rate. Recognizing these symptoms is crucial for seeking timely medical advice and managing the condition effectively.Causes of SVT
SVT is caused by disruptions in the heart's electrical system, which controls the rhythm and rate of heartbeats. These disruptions can result from structural abnormalities in the heart, such as extra electrical pathways or circuits that allow signals to loop and trigger rapid heartbeats. This is often seen in conditions like Wolff-Parkinson-White syndrome, a congenital heart defect. Other factors that can contribute to SVT include high levels of stress, excessive caffeine or alcohol consumption, and the use of certain medications or stimulants. Hormonal changes, such as those occurring during pregnancy, can also increase the likelihood of SVT episodes. Additionally, underlying health conditions like thyroid disorders, heart disease, or electrolyte imbalances may play a role in triggering or exacerbating the condition. Understanding these causes can help individuals identify potential triggers and work with healthcare providers to manage their risk.Introduction to Vagal Maneuvers
Vagal maneuvers are simple, non-invasive techniques designed to activate the vagus nerve, which plays a key role in regulating heart rate. These methods are commonly used as a first-line approach to slow down a rapid heartbeat, particularly in cases of supraventricular tachycardia (SVT). Examples include the Valsalva maneuver, where a person exhales forcefully while keeping their mouth and nose closed, and the carotid sinus massage, which involves gentle pressure applied to the neck. When performed correctly and under medical guidance, these maneuvers are typically safe and can often restore a normal heart rhythm without the need for medication or invasive procedures. However, their effectiveness depends on the underlying cause of the rapid heartbeat and may not work for all types of arrhythmias. Understanding how these maneuvers work and their connection to the vagus nerve can help individuals manage specific heart rhythm issues effectively.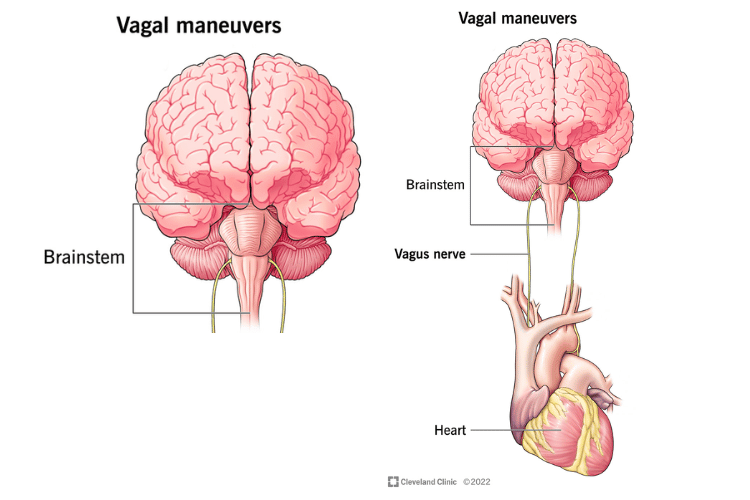
How Vagal Maneuvers Work?
The effectiveness of vagal maneuvers lies in their ability to stimulate the vagus nerve, which is part of the parasympathetic nervous system. This nerve extends from the brainstem to various organs, including the heart, and helps regulate involuntary functions such as heart rate and digestion. When the vagus nerve is activated, it sends signals to the heart to slow down its electrical activity, which can help interrupt the rapid rhythms associated with SVT. For example, the Valsalva maneuver increases pressure in the chest cavity, which temporarily affects blood flow to the heart and triggers a reflex that slows the heart rate. Similarly, the carotid sinus massage stimulates pressure sensors in the neck, prompting the vagus nerve to reduce the heart's electrical activity. These mechanisms make vagal maneuvers a valuable tool for managing certain types of arrhythmias.Importance of the Vagus Nerve
The vagus nerve is a critical component of the body's autonomic nervous system, responsible for maintaining balance between the "fight or flight" and "rest and digest" responses. Its role in regulating heart rate is particularly significant, as it helps ensure that the heart functions efficiently under varying conditions. By slowing down the heart rate, the vagus nerve prevents excessive strain on the cardiovascular system and promotes overall stability. Beyond its impact on heart rhythm, the vagus nerve influences a wide range of bodily functions, including digestion, immune response, and mood regulation. This highlights the broader importance of maintaining vagal tone, which refers to the nerve's ability to function optimally. Techniques such as deep breathing, meditation, and regular exercise can enhance vagal tone, contributing to better overall health and resilience against stress.Types of Vagal Maneuvers
Vagal maneuvers are a group of techniques designed to stimulate the vagus nerve, which can help regulate heart rhythm and slow down a rapid heartbeat. These methods are often used as a first-line approach for managing certain arrhythmias, such as supraventricular tachycardia (SVT). Below are the most common types of vagal maneuvers, their applications, and when they are typically used.Valsalva Maneuver
The Valsalva maneuver is one of the most widely used vagal maneuvers due to its simplicity and effectiveness. This technique involves forcefully exhaling against a closed airway, which can be achieved by pinching the nose, closing the mouth, and attempting to breathe out. The increased pressure in the chest cavity temporarily alters blood flow to the heart, triggering a reflex that slows the heart rate. This maneuver is particularly effective for terminating episodes of SVT and is often recommended as a first step before considering medication or other interventions. However, it is important to perform the Valsalva maneuver correctly to avoid complications. For example, excessive force or prolonged attempts can lead to dizziness or fainting. Medical supervision is advised, especially for individuals with underlying heart conditions.Other Common Vagal Maneuvers
In addition to the Valsalva maneuver, there are several other techniques that can stimulate the vagus nerve and help manage rapid heart rhythms:- Carotid Sinus Massage: This involves gently massaging the carotid artery on one side of the neck. The pressure stimulates sensors in the artery, which activate the vagus nerve and slow the heart rate. This method should only be performed by a healthcare professional, as improper technique can lead to complications, especially in individuals with carotid artery disease.
- Diving Reflex Stimulation: Splashing cold water on the face or immersing the face in ice-cold water can activate the diving reflex, a natural response that slows the heart rate. This technique is particularly useful for children or individuals who may not tolerate other maneuvers.
- Coughing or Gagging: Forceful coughing or inducing a gag reflex can also stimulate the vagus nerve. These methods are less commonly used but can be effective in certain situations.
Indications for Use
Vagal maneuvers are primarily indicated for managing episodes of supraventricular tachycardia, a condition characterized by a rapid heart rate originating above the ventricles. These techniques are most effective when performed early in the episode, before the heart rhythm becomes too unstable. They are also used as a diagnostic tool to help identify the type of arrhythmia by observing how the heart responds to vagal stimulation. While vagal maneuvers are generally safe, they are not suitable for all individuals or conditions. For example, people with carotid artery disease, recent strokes, or certain heart conditions should avoid specific maneuvers, such as carotid sinus massage. It is essential to consult a healthcare provider to determine the most appropriate technique and ensure it is performed safely.Performing the Valsalva Maneuver for SVT
The Valsalva maneuver is a widely used technique to manage episodes of supraventricular tachycardia (SVT). By stimulating the vagus nerve, this maneuver can help slow down a rapid heart rate and restore a normal rhythm. Proper execution is essential for its effectiveness, and understanding when to use it can make a significant difference in managing SVT episodes.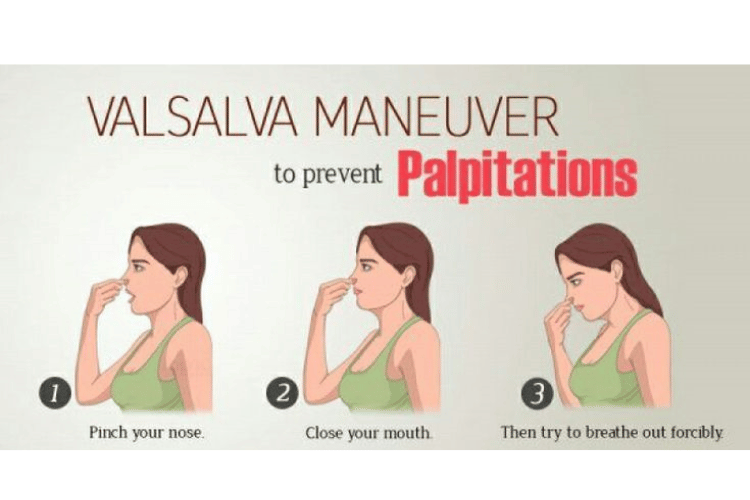
Step-by-Step Guide
Performing the Valsalva maneuver involves a series of simple steps that can be done in most settings. Here’s how to do it correctly:- Prepare Your Position: Sit or lie down in a comfortable position to avoid dizziness or fainting during the maneuver. Ensure you are in a safe environment where you can rest if needed.
- Close Your Airway: Pinch your nose shut with your fingers and close your mouth tightly to prevent air from escaping.
- Exhale Forcefully: Attempt to exhale as if you are blowing up a balloon, but keep your airway closed. This creates pressure in your chest cavity, which is key to stimulating the vagus nerve.
- Hold the Pressure: Maintain the exhalation effort for about 10 to 15 seconds. Avoid straining excessively, as this can cause discomfort or dizziness.
- Release and Relax: After holding the pressure, release your breath and relax. You may feel your heart rate begin to slow down as the maneuver takes effect.
Tips for Effectiveness
To maximize the effectiveness of the Valsalva maneuver, consider the following tips:- Stay Calm: Anxiety or stress can make it harder to perform the maneuver correctly. Take a moment to relax before starting.
- Use Proper Timing: Perform the maneuver as soon as you notice symptoms of SVT, such as a rapid heartbeat or palpitations. Early intervention increases the likelihood of success.
- Combine with Positioning: Lying down or reclining during the maneuver can enhance its effectiveness by improving blood flow and reducing the risk of dizziness.
- Hydrate Beforehand: Dehydration can affect the body’s response to the maneuver. Ensure you are well-hydrated, especially if you are prone to SVT episodes.
When to Seek Medical Attention
While the Valsalva maneuver is a safe and effective technique for many individuals, there are situations where medical attention is necessary. Seek immediate help if:- The maneuver does not resolve the rapid heartbeat after one or two attempts.
- Symptoms such as chest pain, severe dizziness, or fainting occur during or after the maneuver.
- The individual has a history of heart conditions or other medical issues that may complicate the use of vagal maneuvers.
Medications and Procedures for SVT
When managing supraventricular tachycardia (SVT), vagal maneuvers are often the first step in attempting to restore a normal heart rhythm. However, in cases where these techniques are ineffective or the condition is recurrent, medications and medical procedures may be necessary. Understanding these options can help individuals and healthcare providers make informed decisions about treatment.When Vagal Maneuvers are Insufficient
While vagal maneuvers are effective for many individuals, they may not always resolve an episode of SVT. This can occur if the arrhythmia is particularly persistent or if the underlying cause is not responsive to vagal nerve stimulation. In such cases, medical intervention is required to prevent complications and restore a normal heart rhythm. If symptoms such as chest pain, severe dizziness, or fainting accompany the rapid heartbeat, immediate medical attention is essential. Additionally, individuals who experience frequent or prolonged episodes of SVT may require a more comprehensive treatment plan to manage the condition and reduce the risk of recurrence.Medications to Manage SVT
Medications are often used to control the heart rate and prevent future episodes of SVT. These drugs work by targeting the electrical signals in the heart that cause the arrhythmia. Commonly prescribed medications include:- Adenosine: This is often administered in a hospital setting to quickly terminate an episode of SVT. Adenosine works by temporarily blocking electrical signals in the heart, allowing it to reset to a normal rhythm.
- Beta-Blockers: These medications, such as metoprolol or propranolol, reduce the heart rate by blocking the effects of adrenaline. They are often prescribed for long-term management of SVT.
- Calcium Channel Blockers: Drugs like verapamil or diltiazem help relax the heart’s muscles and slow down electrical conduction, making them effective for controlling SVT episodes.
- Antiarrhythmic Drugs: Medications such as flecainide or amiodarone are used to stabilize the heart’s electrical activity and prevent arrhythmias. These are typically reserved for individuals with more severe or recurrent SVT.
Procedures for Persistent SVT
For individuals with persistent or recurrent SVT that does not respond to medications, medical procedures may be necessary. These interventions are designed to address the root cause of the arrhythmia and provide long-term relief. Common procedures include:- Catheter Ablation: This minimally invasive procedure involves threading a catheter through a blood vessel to the heart. Once the source of the abnormal electrical signals is identified, it is destroyed using heat (radiofrequency ablation) or cold (cryoablation). Catheter ablation is highly effective and often considered a permanent solution for SVT.
- Electrical Cardioversion: In cases of severe or prolonged SVT, electrical cardioversion may be performed. This involves delivering a controlled electric shock to the heart to reset its rhythm. It is typically used in emergency situations or when other treatments have failed.
- Pacemaker Implantation: For individuals with underlying heart conditions or recurrent arrhythmias, a pacemaker may be implanted to regulate the heart’s rhythm. This device ensures that the heart maintains a steady and normal rate.
Frequently Asked Questions
Q: What are vagal maneuvers and how do they work?
A: Vagal maneuvers are techniques used to stimulate the vagus nerve, which can help slow down the heart rate and restore a normal rhythm. These actions trigger responses in the autonomic nervous system, particularly the parasympathetic branch, which reduces heart rate and can terminate certain types of arrhythmias.
Q: What types of conditions can vagal maneuvers help with?
A: Vagal maneuvers are most commonly used to manage paroxysmal supraventricular tachycardia (PSVT), a condition characterized by a rapid heart rate originating from the atrioventricular (AV) node. They may also assist in stabilizing abnormal heart rhythms, offering a non-invasive alternative to medication in some cases.
Q: How effective are vagal maneuvers in terminating arrhythmias?
A: The effectiveness of vagal maneuvers varies depending on the type of arrhythmia and individual factors. Many patients find relief from symptoms of tachycardia through techniques like carotid sinus massage or the Valsalva maneuver. However, their success depends on the specific condition and may not work for all arrhythmias.
Q: What is carotid sinus massage and how is it performed?
A: Carotid sinus massage involves applying gentle pressure to the carotid artery in the neck to stimulate baroreceptors, which can enhance vagal tone and slow the heart rate. This procedure is typically performed by a healthcare professional in a clinical setting to ensure safety, as improper technique can pose risks.
Q: Are there any risks associated with performing vagal maneuvers?
A: While generally safe, vagal maneuvers can carry risks, especially for individuals with carotid sinus hypersensitivity or pre-existing cardiovascular conditions. Potential side effects include dizziness, fainting, or shortness of breath. It’s important to consult a healthcare provider before attempting these techniques, particularly outside a clinical setting.
Q: Can vagal maneuvers be used in emergency situations?
A: Yes, vagal maneuvers can be helpful in emergency situations to manage rapid heart rates. While they are often performed by medical professionals in a hospital, certain maneuvers, like the Valsalva maneuver, can be done at home. However, if symptoms persist or worsen, immediate medical attention is essential.
Q: What are some common physical maneuvers that can be used?
A: Common vagal maneuvers include holding your breath, immersing your face in ice water (diving reflex), and bearing down as if having a bowel movement (Valsalva maneuver). These actions stimulate the vagus nerve and may help slow the heart rate. Always practice these techniques under medical guidance to ensure safety.
Q: How do vagal maneuvers influence the autonomic nervous system?
A: Vagal maneuvers enhance the parasympathetic response of the autonomic nervous system, counteracting the effects of the sympathetic system. This balance reduces heart rate and stabilizes rhythm by releasing acetylcholine, which slows electrical impulses in the heart and promotes normal cardiac function.
Q: When should I seek medical attention after performing vagal maneuvers?
A: Seek medical attention if symptoms persist after attempting vagal maneuvers or if you experience severe chest pain, dizziness, or difficulty breathing. Persistent symptoms may indicate a more serious condition requiring further evaluation and treatment by a healthcare professional.
Conclusion
Vagal maneuvers are effective, non-invasive techniques for managing rapid heart rates and other conditions influenced by the vagus nerve. By understanding how and when to use these methods, you can take control of certain medical situations and potentially avoid more invasive treatments. Always consult a healthcare professional for guidance on using vagal maneuvers safely.















 Login with Google
Login with Google Login with Facebook
Login with Facebook