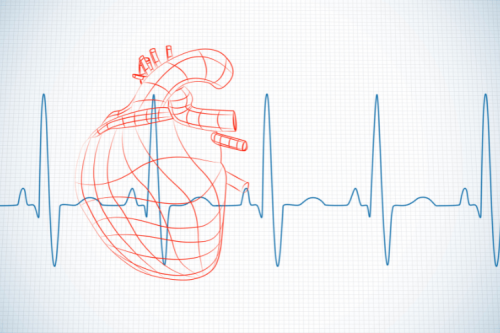
Atrial fibrillation (AFib) and ventricular fibrillation (VFib) are two types of irregular heart rhythms, but they differ significantly in their causes, symptoms, and severity. While AFib is a common condition that can often be managed, VFib is a life-threatening emergency requiring immediate medical attention. In this blog, we’ll break down the key differences between AFib and VFib, their symptoms, and how they are treated.
Atrial Fibrillation Overview
Atrial fibrillation, often abbreviated as AFib, is a common heart rhythm disorder that affects millions of people worldwide. It occurs when the heart's upper chambers (atria) beat irregularly and out of sync with the lower chambers (ventricles). This condition can lead to various complications, including blood clots, stroke, and heart failure, making early diagnosis and management essential.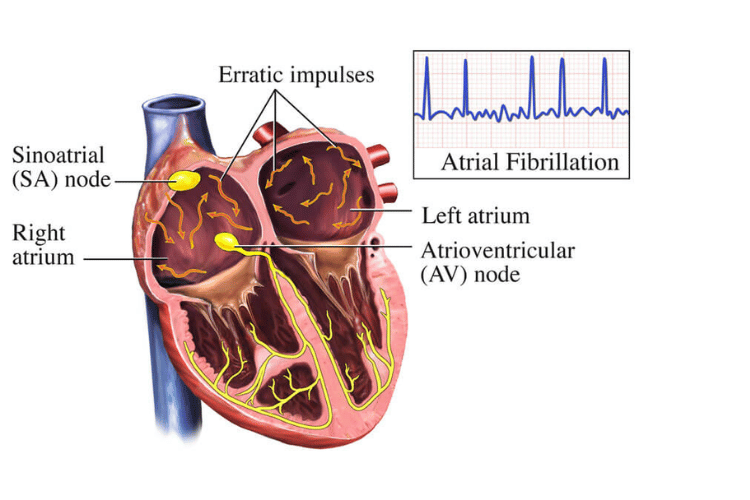
Atrial Fibrillation Overview
Definition of Atrial Fibrillation
Atrial fibrillation is a type of arrhythmia, or irregular heartbeat, where the electrical signals in the atria become chaotic. Instead of contracting in a coordinated manner, the atria quiver or fibrillate, disrupting the normal flow of blood into the ventricles. This irregular rhythm can be occasional (paroxysmal), persistent, or long-standing, depending on its duration and frequency. AFib can significantly impact the heart's efficiency, leading to symptoms like fatigue and shortness of breath. In some cases, it may go unnoticed, while in others, it can cause severe complications, such as the formation of blood clots that increase the risk of stroke. Understanding the nature of AFib is crucial for effective treatment and prevention of related health issues.Causes of Atrial Fibrillation
Atrial fibrillation can result from a variety of factors, including underlying health conditions, lifestyle choices, and age-related changes in the heart. Common causes include:- Heart-Related Conditions:
- High blood pressure (hypertension)
- Coronary artery disease
- Heart valve disorders
- Congenital heart defects
- Heart failure or cardiomyopathy
- Non-Cardiac Factors:
- Hyperthyroidism or other thyroid disorders
- Sleep apnea, which disrupts normal breathing during sleep
- Chronic lung diseases, such as COPD
- Excessive alcohol consumption or binge drinking (often referred to as "holiday heart syndrome")
- Stimulant use, including caffeine, nicotine, or certain medications
- Age and Genetics:
- The risk of AFib increases with age, particularly in individuals over 65.
- A family history of atrial fibrillation may also predispose someone to the condition.
- Lifestyle Factors:
- Obesity and a sedentary lifestyle can contribute to the development of AFib.
- Stress and poor sleep patterns may also play a role in triggering irregular heart rhythms.
Symptoms of Atrial Fibrillation
The symptoms of atrial fibrillation can vary widely, ranging from mild to severe, and some individuals may not experience any noticeable symptoms at all. Common signs of AFib include:- Irregular Heartbeat: A sensation of the heart racing, fluttering, or skipping beats is one of the most common symptoms.
- Fatigue: Many individuals with AFib report feeling unusually tired or lacking energy, even after minimal physical activity.
- Shortness of Breath: Difficulty breathing, especially during exertion or while lying down, is a frequent complaint.
- Chest Discomfort: Some people may experience chest pain or pressure, which should always be evaluated by a healthcare provider.
- Dizziness or Lightheadedness: The irregular heart rhythm can reduce blood flow to the brain, causing feelings of dizziness or fainting.
Ventricular Fibrillation Overview
Ventricular fibrillation, often referred to as VFib, is a life-threatening heart rhythm disorder that requires immediate medical attention. It occurs when the ventricles, the heart's lower chambers, quiver instead of contracting effectively, disrupting the heart's ability to pump blood to the body and brain. Without prompt treatment, VFib can lead to cardiac arrest and death within minutes, making it one of the most critical cardiac emergencies.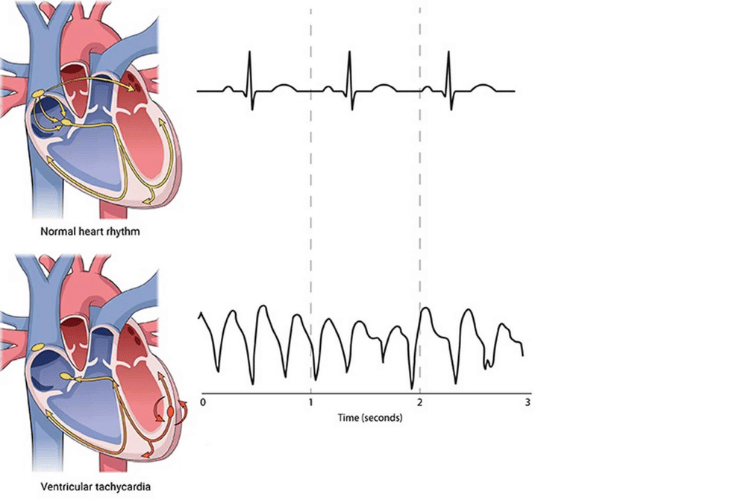
Ventricular Fibrillation
Definition of Ventricular Fibrillation
Ventricular fibrillation is a type of arrhythmia characterized by rapid, erratic electrical impulses in the ventricles. These disorganized signals cause the heart's lower chambers to quiver or "fibrillate" instead of pumping blood efficiently. As a result, blood flow to vital organs, including the brain, is severely compromised. Unlike other arrhythmias, VFib is almost always a medical emergency. It is often associated with sudden cardiac arrest, where the heart stops beating altogether. Immediate intervention, such as defibrillation or cardiopulmonary resuscitation (CPR), is essential to restore normal heart rhythm and prevent fatal outcomes.Causes of Ventricular Fibrillation
Ventricular fibrillation can be triggered by various factors, most of which are related to underlying heart conditions or external influences. Common causes include:- Heart-Related Conditions:
- Coronary Artery Disease (CAD): Blocked or narrowed arteries can reduce blood flow to the heart, increasing the risk of VFib.
- Heart Attack (Myocardial Infarction): Damage to the heart muscle during a heart attack can disrupt electrical signals, leading to VFib.
- Cardiomyopathy: Conditions that weaken or enlarge the heart muscle can make it more susceptible to erratic rhythms.
- Congenital Heart Defects: Structural abnormalities present at birth can increase the likelihood of VFib.
- Electrolyte Imbalances:
- Low levels of potassium, magnesium, or calcium in the blood can interfere with the heart's electrical activity, triggering VFib.
- Electrical Shock or Trauma:
- Direct injury to the heart or exposure to high-voltage electricity can disrupt normal heart rhythms.
- Drug Use or Overdose:
- Certain medications, recreational drugs, or toxic substances can affect the heart's electrical system, increasing the risk of VFib.
- Genetic Factors:
- Inherited conditions, such as long QT syndrome or Brugada syndrome, can predispose individuals to ventricular fibrillation.
Symptoms of Ventricular Fibrillation
The symptoms of ventricular fibrillation often appear suddenly and progress rapidly, making it essential to recognize the warning signs. Common symptoms include:- Sudden Loss of Consciousness: As the heart fails to pump blood effectively, the brain is deprived of oxygen, leading to fainting or collapse.
- No Pulse or Breathing: In VFib, the heart's pumping action stops, resulting in the absence of a detectable pulse or normal breathing.
- Chest Pain or Discomfort: Some individuals may experience chest pain or tightness before VFib occurs, particularly if it is related to a heart attack.
- Dizziness or Lightheadedness: Reduced blood flow to the brain can cause feelings of dizziness or impending fainting.
- Extreme Fatigue or Weakness: In some cases, individuals may experience unusual weakness or fatigue before the onset of VFib.
Key Differences Between Atrial Fibrillation and Ventricular Fibrillation
Atrial fibrillation (AFib) and ventricular fibrillation (VFib) are both types of arrhythmias, or irregular heart rhythms, but they differ significantly in their causes, symptoms, and severity. Understanding these differences is crucial for recognizing the conditions and ensuring appropriate treatment. While AFib is often a chronic condition that can be managed, VFib is a life-threatening emergency requiring immediate intervention.Differences in Heartbeat Patterns
The primary distinction between atrial fibrillation and ventricular fibrillation lies in the heart chambers affected and the nature of the irregular rhythm.- Atrial Fibrillation: In AFib, the irregular electrical signals originate in the atria, the heart's upper chambers. These chaotic signals cause the atria to quiver instead of contracting effectively, leading to an irregular and often rapid heartbeat. Despite the irregularity, the ventricles may still pump blood, albeit less efficiently. This means that AFib, while serious, is not immediately life-threatening in most cases.
- Ventricular Fibrillation: VFib, on the other hand, affects the ventricles, the heart's lower chambers responsible for pumping blood to the rest of the body. In VFib, the electrical signals in the ventricles become disorganized, causing the heart to quiver instead of pumping blood. This results in a complete loss of blood circulation, making VFib a medical emergency that can lead to sudden cardiac arrest within minutes.
Differences in Symptoms
The symptoms of atrial fibrillation and ventricular fibrillation also vary significantly due to the differing impacts on blood flow and heart function.- Atrial Fibrillation Symptoms:
AFib symptoms can range from mild to severe and may include:
- Irregular or rapid heartbeat (palpitations)
- Fatigue and weakness
- Shortness of breath, especially during physical activity
- Dizziness or lightheadedness
- Chest discomfort or mild pain
- Ventricular Fibrillation Symptoms:
VFib symptoms are far more severe and develop rapidly, often without warning. These include:
- Sudden loss of consciousness due to the lack of blood flow to the brain
- Absence of a detectable pulse or breathing
- Sudden collapse or fainting
- Cyanosis (bluish discoloration of the skin) due to oxygen deprivation
Differences in Treatment Approaches
The treatment strategies for atrial fibrillation and ventricular fibrillation differ significantly due to the varying severity and underlying causes of the conditions.- Atrial Fibrillation Treatment:
AFib is typically managed with a combination of medications and lifestyle changes to control the heart rate, restore normal rhythm, and prevent complications like blood clots. Common treatments include:
- Medications: Beta-blockers, calcium channel blockers, and antiarrhythmic drugs to regulate heart rate and rhythm. Anticoagulants are often prescribed to reduce the risk of stroke.
- Cardioversion: A procedure that uses electrical shocks or medications to restore a normal heart rhythm.
- Ablation Therapy: A minimally invasive procedure that targets and destroys the areas of the heart causing irregular electrical signals.
- Lifestyle Modifications: Quitting smoking, reducing alcohol intake, and managing conditions like high blood pressure or sleep apnea.
- Ventricular Fibrillation Treatment:
VFib requires immediate emergency care to restore blood circulation and prevent death. Key treatments include:
- Defibrillation: The use of an automated external defibrillator (AED) or manual defibrillator to deliver an electric shock to the heart, resetting its rhythm.
- Cardiopulmonary Resuscitation (CPR): Performed until defibrillation is available, CPR helps maintain blood flow to vital organs.
- Medications: Epinephrine and antiarrhythmic drugs may be administered during resuscitation efforts.
- Implantable Cardioverter-Defibrillator (ICD): For individuals at high risk of VFib recurrence, an ICD may be implanted to monitor and correct abnormal rhythms.
Diagnosing Atrial Fibrillation and Ventricular Fibrillation
Accurate diagnosis of atrial fibrillation (AFib) and ventricular fibrillation (VFib) is essential for effective treatment and prevention of complications. While both conditions involve irregular heart rhythms, their diagnostic approaches differ due to the distinct nature and severity of each condition. Early detection plays a critical role in managing AFib and saving lives in cases of VFib.
Diagnostic Tests for Atrial Fibrillation
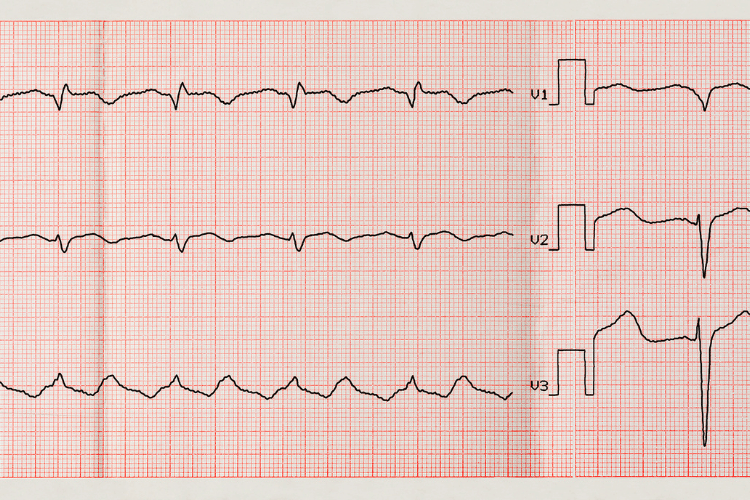
Diagnosing atrial fibrillation often involves a combination of clinical evaluation, patient history, and diagnostic tests to confirm the presence of irregular heart rhythms and identify underlying causes. Common diagnostic methods include:- Electrocardiogram (ECG): The most common and reliable test for detecting AFib, an ECG records the heart's electrical activity. It can identify irregular rhythms, rapid heart rates, and other abnormalities associated with AFib.
- Holter Monitor: For patients with intermittent symptoms, a Holter monitor is a portable device worn for 24 to 48 hours to continuously record heart activity. This helps detect episodes of AFib that may not occur during a standard ECG.
- Event Monitor: Similar to a Holter monitor, an event monitor is used for longer periods, allowing patients to record heart activity during specific symptoms.
- Echocardiogram: This imaging test uses ultrasound to assess the heart's structure and function. It can identify issues like blood clots, valve problems, or heart enlargement that may contribute to AFib.
- Blood Tests: These tests help identify potential triggers, such as thyroid disorders or electrolyte imbalances, that may cause or worsen AFib.
Diagnostic Tests for Ventricular Fibrillation
Ventricular fibrillation is a medical emergency, and its diagnosis often occurs in critical situations, such as during cardiac arrest. The focus is on rapid identification and immediate intervention. Key diagnostic methods include:- Electrocardiogram (ECG): An ECG is the primary tool for diagnosing VFib. It reveals chaotic, disorganized electrical activity in the ventricles, confirming the condition. In emergency settings, ECG monitoring is often performed during resuscitation efforts.
- Cardiac Monitoring: In hospital settings, continuous cardiac monitoring can detect VFib in patients at risk, such as those recovering from a heart attack or undergoing surgery.
- Blood Tests: After stabilizing the patient, blood tests may be conducted to identify contributing factors, such as electrolyte imbalances, drug toxicity, or underlying heart conditions.
- Imaging Tests: Once the patient is stabilized, imaging studies like echocardiograms or coronary angiography may be used to assess heart function and identify structural abnormalities or blockages that could have triggered VFib.
Importance of Early Diagnosis
Early diagnosis of atrial fibrillation and ventricular fibrillation is crucial for preventing complications and improving outcomes.- For Atrial Fibrillation: Early detection allows for timely management, reducing the risk of stroke, heart failure, and other complications. Identifying AFib in its early stages also provides an opportunity to address underlying causes, such as high blood pressure or thyroid disorders, and implement lifestyle changes to improve heart health.
- For Ventricular Fibrillation: In the case of VFib, early diagnosis is often a matter of life and death. Rapid identification and intervention, such as defibrillation, can restore normal heart rhythm and prevent sudden cardiac death. For individuals at high risk of VFib, such as those with a history of heart attacks or genetic conditions, early diagnosis and preventive measures, like implantable cardioverter-defibrillators (ICDs), can be life-saving.
Conclusion: Understanding AFib and VFib
Atrial fibrillation (AFib) and ventricular fibrillation (VFib) are two distinct heart rhythm disorders that differ significantly in their causes, symptoms, and severity. While AFib is often a manageable chronic condition, VFib is a life-threatening emergency requiring immediate intervention. Understanding these differences is essential for effective diagnosis, treatment, and prevention of complications.Summary of Key Differences
The primary differences between AFib and VFib lie in the heart chambers affected, the nature of the irregular rhythm, and the associated risks.- Heart Chambers Involved: AFib originates in the atria (upper chambers), causing them to quiver and disrupt blood flow to the ventricles. VFib occurs in the ventricles (lower chambers), leading to chaotic electrical activity that halts the heart's ability to pump blood.
- Severity: AFib, while serious, is rarely immediately life-threatening. In contrast, VFib is a critical emergency that can result in sudden cardiac arrest and death within minutes if not treated.
- Symptoms: AFib symptoms include palpitations, fatigue, and shortness of breath, while VFib symptoms are more severe, such as sudden collapse, loss of consciousness, and absence of a pulse.
- Treatment Approaches: AFib is managed with medications, lifestyle changes, and procedures like cardioversion or ablation. VFib requires immediate defibrillation, CPR, and potentially long-term solutions like implantable cardioverter-defibrillators (ICDs).
Implications for Treatment
The differences between AFib and VFib have significant implications for treatment strategies.- For Atrial Fibrillation: Treatment focuses on long-term management to control heart rate, restore normal rhythm, and prevent complications like stroke. Medications such as anticoagulants and antiarrhythmics play a central role, while procedures like ablation or cardioversion may be necessary for persistent cases. Lifestyle modifications, including weight management and smoking cessation, are also critical for improving outcomes.
- For Ventricular Fibrillation: The priority is immediate life-saving intervention. Defibrillation and CPR are essential to restore normal heart rhythm and maintain blood circulation. For individuals at high risk of recurrence, preventive measures like ICD implantation and addressing underlying conditions, such as coronary artery disease, are vital.
Future Directions in Research
Ongoing research into atrial and ventricular fibrillation aims to improve diagnostic methods, treatment options, and preventive strategies. Key areas of focus include:- Advancements in Technology: Innovations in wearable devices and remote monitoring are making it easier to detect arrhythmias early, even in asymptomatic individuals. These tools can provide real-time data on heart rhythms, enabling timely intervention.
- Personalized Medicine: Research is exploring how genetic factors influence the development of AFib and VFib, paving the way for personalized treatment plans tailored to an individual’s unique risk profile.
- Improved Ablation Techniques: Advances in catheter ablation technology are enhancing the precision and success rates of procedures used to treat AFib, reducing the need for repeat interventions.
- Prevention Strategies: Studies are investigating the role of lifestyle factors, such as diet, exercise, and stress management, in preventing arrhythmias and improving overall heart health.
- New Medications: The development of novel drugs targeting specific pathways involved in arrhythmias holds promise for more effective and safer treatment options.
Frequently Asked Questions
Q: What is the main difference between AFib and VFib?
A: Atrial fibrillation (AFib) and ventricular fibrillation (VFib) are both types of arrhythmias, but they affect different parts of the heart and have varying levels of severity. AFib involves the upper chambers (atria) and causes an irregular heart rhythm, which can lead to complications like stroke. VFib, on the other hand, occurs in the lower chambers (ventricles) and disrupts the heart's ability to pump blood, making it a life-threatening emergency.
Q: What are the symptoms of AFib?
A: Symptoms of AFib may include heart palpitations, shortness of breath, fatigue, dizziness, and chest discomfort. While some individuals experience noticeable symptoms, others may not realize they have AFib until it is detected during a medical exam. If left untreated, AFib can lead to serious complications such as stroke or heart failure.
Q: What are the symptoms of AFib and VFib?
A: AFib symptoms typically include an irregular or rapid heartbeat, fatigue, and shortness of breath. In contrast, VFib often presents as sudden collapse, loss of consciousness, and the absence of a pulse. VFib is a medical emergency that requires immediate defibrillation and advanced care to prevent fatal outcomes.
Q: Can AFib cause VFib?
A: While AFib does not directly cause VFib, it can increase the risk of complications that may lead to VFib, particularly in individuals with preexisting heart conditions. AFib can contribute to changes in the heart's electrical system and structure, which may predispose someone to ventricular arrhythmias, including VFib.
Q: How is VFib treated?
A: VFib is treated as a critical medical emergency. The primary treatment is defibrillation, which delivers an electrical shock to the heart to restore a normal rhythm. Additional care may include CPR, medications like epinephrine, and interventions to address underlying causes, such as coronary artery blockages or electrolyte imbalances.
Q: What are the causes of VFib?
A: VFib can be triggered by several factors, including heart attacks, untreated arrhythmias like AFib, severe electrolyte imbalances (e.g., low potassium or magnesium), and structural heart diseases. Any condition that disrupts the heart's electrical signals can lead to VFib, making it essential to manage risk factors proactively.
Q: How can one diagnose AFib?
A: AFib is typically diagnosed using an electrocardiogram (ECG or EKG), which records the heart's electrical activity and identifies irregular rhythms. Additional diagnostic tools may include Holter monitors, echocardiograms, and blood tests to evaluate overall heart health and detect potential triggers.
Q: Who is at risk for developing AFib?
A: Risk factors for AFib include advanced age, high blood pressure, heart disease, obesity, and a history of other arrhythmias. Lifestyle factors such as smoking, excessive alcohol consumption, and poor sleep can also increase the likelihood of developing AFib. Managing these risks is key to maintaining a healthy heart rhythm.
Q: What should I know about the likelihood of both AFib and VFib?
A: AFib is the most common type of arrhythmia and is often manageable with proper treatment. VFib, while less common, is far more dangerous and requires immediate medical intervention. Understanding the differences between these conditions is crucial for recognizing symptoms, seeking timely care, and reducing the risk of complications.
Conclusion
Understanding the differences between AFib and VFib is crucial for recognizing their symptoms and seeking appropriate care. While AFib can often be managed with medication and lifestyle changes, VFib is a medical emergency that demands immediate intervention. Knowing these distinctions can help you act quickly and protect your heart health.






 Login with Google
Login with Google Login with Facebook
Login with Facebook