
Cardiopulmonary resuscitation (CPR) is a life-saving technique used in emergencies when someone’s breathing or heartbeat has stopped. While chest compressions are crucial for maintaining blood circulation, adequate ventilation is equally vital to ensure oxygen delivery to the brain and vital organs. Among the various methods of providing rescue breaths, the bag-mask device (BMD) stands out as a key tool for healthcare providers and first responders.
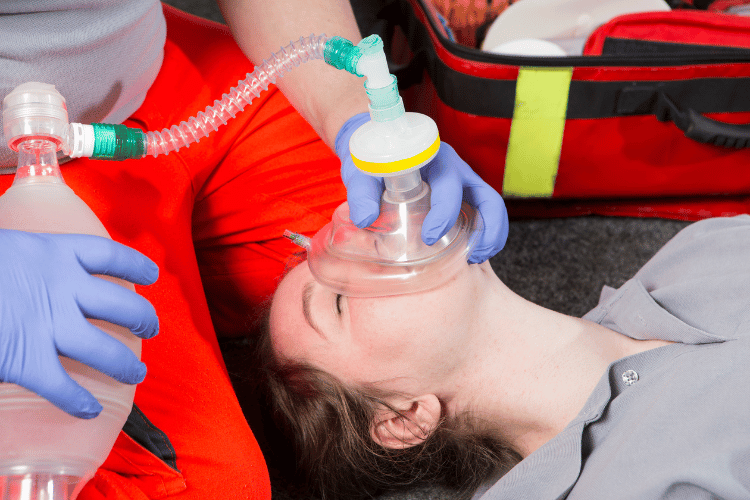
While bystanders may rely on mouth-to-mouth ventilation during CPR, medical professionals often use a bag-mask device for more controlled and efficient breath delivery. Understanding how to properly use this device properly—from achieving a proper seal to delivering the right volume of air—can mean the difference between life and death in a cardiac or respiratory arrest.
Let’s explore how bag-mask ventilation works, the correct technique for delivering breaths, and common challenges faced during resuscitation efforts.
Understanding CPR and the Importance of Ventilation
Cardiopulmonary resuscitation (CPR) is a life-saving technique used during cardiac arrest to maintain blood flow and oxygen delivery to vital organs. While chest compressions are the cornerstone of CPR, ventilation plays a critical role in ensuring oxygenation, especially in prolonged resuscitation efforts. This guide explains what CPR entails, highlights the role of ventilation in the process, and provides guidance on delivering effective breaths.
What is CPR?
CPR is an emergency procedure designed to restore circulation and oxygenation in individuals experiencing cardiac arrest. Key components include:
- Chest Compressions: Rhythmic compressions on the chest mimic the heart’s pumping action, maintaining blood flow to the brain and other vital organs.
- Ventilation: Providing breaths to supply oxygen to the lungs, which is essential for oxygenating the blood being circulated by compressions.
- Goal: The primary aim of CPR is to preserve life until advanced medical care, such as defibrillation or advanced life support, can be administered. CPR is most effective when initiated immediately after cardiac arrest, as every minute of delay reduces survival chances.

What is CPR
Role of Ventilation in CPR
Ventilation ensures that oxygen is available for circulation during CPR. Its importance includes:
- Oxygen Delivery: Without ventilation, oxygen levels in the blood rapidly decline, compromising organ function.
- Carbon Dioxide Removal: Ventilation helps expel carbon dioxide, preventing acidosis and further complications.
- Balance with Compressions: While compressions are prioritized, ventilation is critical in prolonged resuscitation or cases of respiratory arrest. In certain scenarios, such as witnessed cardiac arrest in adults, compression-only CPR may be sufficient initially, but ventilation becomes essential over time.
How to Deliver Breaths Effectively
Adequate ventilation during CPR requires proper technique to maximize oxygen delivery and minimize complications. Key steps include:
- Open the Airway: Use the head-tilt, chin-lift method to ensure the airway is clear and open.
- Provide Rescue Breaths: Deliver two breaths after every 30 compressions, ensuring each breath lasts about one second and causes visible chest rise.
- Avoid Over-Ventilation: Excessive or forceful breaths can lead to gastric inflation and reduce the effectiveness of compressions. By understanding the role of ventilation and mastering proper techniques, rescuers can enhance the effectiveness of CPR and improve outcomes for individuals in cardiac arrest.
The Bag-Mask Device: Overview and Functionality
The bag-mask device, also known as a bag-valve mask (BVM), is a critical tool in emergency medicine used to provide ventilation to patients who are not breathing or are experiencing inadequate respiration. It is commonly employed in pre-hospital, hospital, and resuscitation settings to deliver oxygen and maintain airway patency. This guide explains what a bag-valve mask is, details its components, and provides instructions on how to use it effectively.
What is a Bag-Valve Mask?
A bag-valve mask is a handheld device designed to assist or replace spontaneous breathing. Key features include:
- Purpose: It delivers positive pressure ventilation by manually squeezing the bag, forcing air or oxygen into the patient’s lungs.
- Applications: Used in cases of respiratory arrest, severe respiratory distress, or during cardiopulmonary resuscitation (CPR).
- Oxygen Delivery: Can be connected to an oxygen source to provide high concentrations of oxygen, improving oxygenation during resuscitation efforts. The BVM is a vital tool for healthcare providers and first responders, providing a non-invasive method to support breathing.

What is a Bag-Valve Mask
Components of the Bag-Mask Device
The bag-mask device consists of several key components that work together to deliver adequate ventilation:
- Self-Inflating Bag: A squeezable bag that refills with air or oxygen after each compression.
- Mask: A soft, transparent mask that creates a seal over the patient’s nose and mouth.
- Reservoir Bag: An optional attachment that stores oxygen, ensuring higher oxygen delivery.
- Oxygen Inlet: A port for connecting an external oxygen source to enhance ventilation. Each component plays a vital role in ensuring the device functions efficiently and delivers adequate ventilation.
How to Use a Bag-Mask Device
Using a bag-mask device requires proper technique to maximize its effectiveness. Key steps include:
- Position the Patient: Place the patient in a supine position and open the airway using the head-tilt, chin-lift,
or jaw-thrust maneuver.
Effective Bag-Mask Ventilation
- Create a Seal: Position the mask over the patient’s nose and mouth, ensuring a tight seal to prevent air leakage.
- Deliver Ventilations: Squeeze the bag gently and steadily, delivering one breath every 5-6 seconds for adults or every 3-5 seconds for children.
- Monitor Effectiveness: Observe for visible chest rise to confirm adequate ventilation and adjust technique as needed. By understanding the functionality and proper use of the bag-mask device, healthcare providers can deliver effective ventilation and improve patient outcomes in critical situations.
Techniques for Effective Bag-Mask Ventilation
Bag-mask ventilation is a critical skill in emergency care, used to provide oxygen and maintain ventilation in patients who are not breathing adequately. Proper technique is essential to ensure effective oxygen delivery and prevent complications. This guide outlines the key methods for achieving adequate bag-mask ventilation, including proper seal and positioning, delivering breaths at the correct rate, and avoiding common mistakes.
Proper Seal and Positioning
Creating a proper seal and positioning the patient correctly are foundational to effective bag-mask ventilation. Key steps include:
- Head and Airway Positioning: Use the head-tilt, chin-lift maneuver to open the airway. For patients with suspected spinal injuries, use the jaw-thrust technique to avoid neck movement.
- Mask Placement: Position the mask over the patient’s nose and mouth, ensuring it covers both without gaps.
- Hand Technique: Use the "E-C clamp" method, where the thumb and index finger form a "C" to hold the mask, while the other fingers form an "E" to lift the jaw and maintain the seal. Proper seal and positioning prevent air leakage and ensure effective ventilation.
Delivering Breaths: 1 Breath Every 6 Seconds
Delivering breaths at the correct rate and volume is crucial for oxygenation and avoiding complications. Guidelines include:
- Breath Rate: Provide one breath every 6 seconds (10 breaths per minute) for adults, ensuring adequate oxygenation without hyperventilation.
- Breath Volume: Squeeze the bag gently to deliver just enough air to cause visible chest rise, avoiding excessive force.
- Monitoring: Observe the chest for rise and fall to confirm effective ventilation and adjust as needed. Maintaining the correct rate and volume ensures optimal oxygen delivery while minimizing risks.
Common Mistakes in Bag-Mask Ventilation
Avoiding common errors is essential for effective bag-mask ventilation. Frequent mistakes include:
- Inadequate Seal: Poor mask placement or hand positioning can lead to air leakage and ineffective ventilation.
- Over-Ventilation: Delivering breaths too quickly or with excessive force can cause gastric inflation, increasing the risk of aspiration.
- Improper Airway Positioning: Failure to open the airway properly can obstruct airflow and reduce ventilation effectiveness. By recognizing and addressing these mistakes, healthcare providers can improve the quality of bag-mask ventilation and enhance patient outcomes in critical situations.
Advanced Considerations in Bag-Mask Ventilation
Bag-mask ventilation is a versatile and essential technique in emergency care, but its effectiveness depends on adapting to specific patient needs and addressing potential challenges. Advanced considerations include tailoring ventilation techniques for different age groups, incorporating supplemental oxygen, and recognizing and managing complications. This guide provides a detailed overview of these critical aspects to enhance the effectiveness of bag-mask ventilation.
Adjusting Ventilation Techniques for Different Age Groups
Ventilation requirements vary significantly across age groups, necessitating adjustments in technique and equipment. Key considerations include:
- Infants and Children: Use smaller masks and bags designed for pediatric patients. Deliver one breath every 3-5 seconds (12-20 breaths per minute) with gentle pressure to avoid lung injury.
- Adults: Provide one breath every 5-6 seconds (10-12 breaths per minute), ensuring visible chest rise without overinflation.
- Elderly Patients: Be cautious of reduced lung compliance and underlying conditions, adjusting ventilation pressure and volume accordingly. Adapting techniques ensures effective oxygenation while minimizing the risk of complications in patients of all ages.
Use of Supplemental Oxygen with Bag-Mask Devices
Supplemental oxygen enhances the effectiveness of bag-mask ventilation by increasing the oxygen concentration delivered to the patient. Key points include:
- Oxygen Source: Connect the bag-valve mask to an oxygen supply, typically set at a flow rate of 10-15 liters per minute.
- Reservoir Bag: Attach a reservoir bag to achieve nearly 100% oxygen delivery, especially in critical situations.
- Monitoring Oxygenation: Use pulse oximetry to assess the patient’s oxygen saturation and adjust oxygen delivery as needed. Incorporating supplemental oxygen improves patient outcomes, particularly in cases of severe hypoxia.
Recognizing and Addressing Complications
Effective bag-mask ventilation requires vigilance to identify and manage potential complications. Common issues include:
- Gastric Inflation: Over-ventilation or improper technique can force air into the stomach, increasing the risk of aspiration. To prevent this, deliver breaths at the correct rate and volume.
- Airway Obstruction: Ensure the airway is open and clear of obstructions, using suction or advanced airway devices if necessary.
- Barotrauma: Excessive ventilation pressure can damage lung tissue, particularly in patients with reduced lung compliance. Use gentle, controlled breaths to avoid this. By addressing these advanced considerations, healthcare providers can optimize bag-mask ventilation and improve patient care in emergency settings.
Frequently Asked Questions
What is a bag mask device?
A bag mask device is a medical apparatus used to provide positive pressure ventilation to individuals who are not breathing adequately. It typically consists of a self-inflating bag, a face mask, and a reservoir bag to deliver oxygen effectively during emergencies.
How do you use a bag mask device?
To use a bag mask device, first, position the mask over the patient’s face, ensuring a proper seal. Hold the mask in place with one hand while using the other hand to squeeze the bag to deliver one breath every 5 to 6 seconds. It's essential to monitor the effectiveness of ventilation by watching for chest rise.
What is the proper technique to hold the mask?
The proper technique to hold the mask involves placing the mask on the patient’s face and using your thumb and index finger to create a seal around the edge of the mask. This ensures that air does not escape while delivering breaths.
How many breaths should be given during CPR?
During CPR, it is recommended to provide 1 breath every 5 to 6 seconds. This rhythm allows for effective ventilation while allowing time for chest compressions, which should be performed continuously.
What should you do if the mask does not seal properly?
If the mask does not seal properly, reposition the mask on the patient's face or adjust your grip to improve the seal. Make sure the mask is the correct size and covers the patient's nose and mouth effectively to prevent air leakage.
How do you know if the ventilation is successful?
Successful ventilation can be assessed by observing the rise and fall of the patient's chest with each squeeze of the bag. Additionally, you should listen for breath sounds and check for a pulse every 2 minutes to ensure effective oxygenation.
What is the significance of the breaths per minute during ventilation?
The breaths per minute are crucial for ensuring the patient receives adequate oxygen. For adults, the standard is 12 to 20 breaths per minute, but in emergencies, focus on delivering breaths every 5 to 6 seconds for effective ventilation.
When should you start CPR with a bag mask device?
You should begin CPR immediately if the patient is unresponsive and not breathing or only gasping. After ensuring the airway is clear, use the bag mask device to provide rescue breaths while also performing chest compressions for optimal care.
Can a bag mask device be used on children?
Yes, a bag mask device can be used on children, but it is important to use the appropriate mask size and adjust the ventilation rate to accommodate the child's needs, typically giving 1 breath every 3 to 5 seconds.
What are the steps for using a bag-mask for effective ventilation?
The steps for using a bag-mask include: first, position the patient appropriately; second, place the mask on the patient’s face and create a seal; third, squeeze the bag to deliver breaths; and finally, monitor the patient's response to ensure effective ventilation.
The Bottom Line
Effective bag-mask ventilation is a critical skill in CPR, ensuring that oxygen reaches the lungs and bloodstream when every second counts. While it requires practice to master—especially maintaining a proper seal and delivering the right volume—the BMD remains a versatile, essential tool in both pre-hospital and hospital settings.
For medical professionals, regular training and simulation drills can help refine technique, while bystanders should at least be familiar with basic rescue breathing methods. Whether used in cardiac arrest, respiratory failure, or during emergency transport, the bag-mask device bridges the gap between collapse and advanced life support, improving survival rates when used correctly.
Choose the right ventilation strategy, apply best practices, and ensure that every breath delivered maximizes the chance of recovery.







 Login with Google
Login with Google Login with Facebook
Login with Facebook