
Hypercapnia, also known as hypercarbia, occurs when there is an excessive buildup of carbon dioxide (CO2) in the bloodstream. This condition can result from respiratory issues, reduced lung function, or other underlying health problems. In this blog, we’ll explore the causes, symptoms, and treatment options for hypercapnia, helping you understand its impact on the body and the importance of timely medical intervention.
Understanding Hypercapnia and Hypercarbia
Hypercapnia and hypercarbia are terms often used interchangeably to describe a condition involving elevated levels of carbon dioxide (CO2) in the blood. While they share similarities, understanding their definitions and subtle differences is essential for accurate diagnosis and treatment. Both conditions are closely linked to respiratory function and can indicate underlying health issues.Definition of Hypercapnia
Hypercapnia refers specifically to the excessive accumulation of carbon dioxide in the bloodstream, typically caused by inadequate ventilation. This condition occurs when the lungs fail to expel CO2 effectively, leading to an imbalance in the body’s acid-base levels. Hypercapnia is often associated with respiratory disorders such as chronic obstructive pulmonary disease (COPD), asthma, or sleep apnea. The condition can manifest in varying degrees of severity. Mild hypercapnia may cause symptoms like headaches, fatigue, and shortness of breath, while severe cases can lead to confusion, dizziness, and even respiratory failure. The primary diagnostic tool for hypercapnia is an arterial blood gas (ABG) test, which measures CO2 levels and blood pH to assess respiratory efficiency.Definition of Hypercarbia
Hypercarbia is a broader term that also describes elevated carbon dioxide levels in the blood. However, it is often used in a more general context to refer to any condition or situation where CO2 levels are abnormally high. This term is commonly applied in medical and environmental discussions, such as in cases of CO2 buildup in confined spaces or during anesthesia. Like hypercapnia, hypercarbia can result from respiratory dysfunction, but it may also occur due to external factors, such as exposure to high concentrations of CO2 in the environment. Symptoms of hypercarbia are similar to those of hypercapnia and include shortness of breath, flushed skin, and mental confusion. The treatment approach depends on the underlying cause and may involve improving ventilation or addressing environmental factors.Difference Between Hypercapnia and Hypercarbia
While hypercapnia and hypercarbia are often used interchangeably, there are subtle distinctions between the two terms. Hypercapnia is more commonly used in clinical settings to describe a medical condition caused by respiratory issues, such as hypoventilation or lung disease. It specifically focuses on the physiological impact of CO2 retention within the body. Hypercarbia, on the other hand, is a more general term that can refer to elevated CO2 levels in any context, including environmental exposure or medical scenarios. For example, hypercarbia might describe CO2 buildup in a poorly ventilated room or during certain medical procedures, such as laparoscopic surgery. In summary, hypercapnia is a subset of hypercarbia, with the former being a medically specific condition and the latter encompassing a broader range of situations involving high CO2 levels. Understanding these differences is important for accurate communication in both medical and non-medical contexts.Causes of Hypercapnia
Hypercapnia, a condition characterized by elevated levels of carbon dioxide (CO2) in the blood, arises when the body is unable to expel CO2 effectively. This imbalance can result from various factors, including respiratory disorders, lifestyle-related conditions, and other underlying health issues. Understanding the causes of hypercapnia is essential for identifying at-risk individuals and implementing effective treatment strategies.Common Causes of Hypercapnia
Hypercapnia can develop due to a range of conditions that impair the respiratory system’s ability to function efficiently. Some of the most common causes include:- Respiratory Disorders: Chronic respiratory conditions, such as asthma, bronchitis, and interstitial lung disease, can reduce lung capacity and hinder the expulsion of CO2.
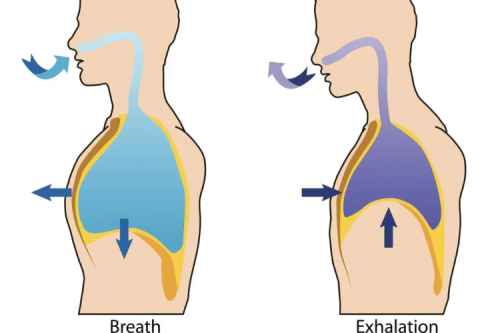
- Hypoventilation: Shallow or slow breathing, often caused by sedative medications, neuromuscular disorders, or obesity, can lead to CO2 retention.
- Chest Trauma: Injuries to the chest wall or rib cage can restrict lung expansion, making it difficult to breathe deeply and expel CO2.
- Sleep Apnea: Repeated interruptions in breathing during sleep can cause CO2 to accumulate over time, particularly in individuals with obstructive sleep apnea.
- Neurological Conditions: Disorders affecting the brain or spinal cord, such as Guillain-Barré syndrome or multiple sclerosis, can impair the muscles involved in breathing, leading to hypercapnia.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of hypercapnia. This progressive lung condition includes diseases like chronic bronchitis and emphysema, which damage the airways and reduce the lungs’ ability to expel CO2. In COPD, the airways become inflamed and narrowed, trapping air in the lungs and leading to CO2 buildup. Patients with COPD often experience symptoms such as chronic cough, wheezing, and shortness of breath. Over time, the inability to expel CO2 can result in respiratory acidosis, where the blood becomes too acidic. This can lead to further complications, including fatigue, confusion, and even respiratory failure in severe cases. Managing COPD through medications, oxygen therapy, and lifestyle changes is crucial for reducing the risk of hypercapnia.Obesity Hypoventilation Syndrome
Obesity hypoventilation syndrome (OHS) is another significant cause of hypercapnia. This condition occurs when excess body weight interferes with normal breathing, leading to shallow or slow respiration. In OHS, the diaphragm and other respiratory muscles may struggle to function effectively due to the added pressure from abdominal fat, reducing lung capacity and impairing CO2 elimination. Individuals with OHS often experience symptoms such as daytime sleepiness, fatigue, and shortness of breath. The condition is closely associated with obstructive sleep apnea, which further exacerbates breathing difficulties. Left untreated, OHS can lead to severe hypercapnia, respiratory failure, and cardiovascular complications. Treatment typically involves weight loss, respiratory support such as CPAP therapy, and addressing any coexisting conditions like sleep apnea. By understanding the common causes of hypercapnia, including conditions like COPD and OHS, healthcare providers can take proactive steps to manage and prevent this potentially serious condition. Early intervention and targeted treatment are essential for improving respiratory health and overall quality of life.Symptoms of Hypercapnia
Hypercapnia, a condition characterized by elevated carbon dioxide (CO2) levels in the blood, presents with a range of symptoms depending on its severity and the underlying cause. Recognizing these symptoms early is crucial for timely intervention and preventing complications. While mild cases may go unnoticed, more severe instances can lead to significant health issues.
of symptoms depending on its severity and the underlying cause. Recognizing these symptoms early is crucial for timely intervention and preventing complications. While mild cases may go unnoticed, more severe instances can lead to significant health issues.
Signs and Symptoms
The symptoms of hypercapnia can range from mild to severe, often progressing as CO2 levels in the blood increase. Common signs include:- Shortness of Breath: Difficulty breathing or feeling like you’re not getting enough air is one of the earliest and most noticeable symptoms.
- Fatigue and Weakness: Elevated CO2 levels can cause a lack of energy and general muscle weakness, making daily activities more challenging.
- Headaches: A dull or throbbing headache is often an early indicator of CO2 buildup in the bloodstream.
- Confusion or Drowsiness: High CO2 levels can impair brain function, leading to mental fog, confusion, or excessive sleepiness.
- Flushed Skin: Increased blood flow caused by CO2 retention may result in redness or warmth in the skin.
- Rapid Heart Rate: The heart may beat faster as the body attempts to compensate for reduced oxygen levels.
- Cyanosis: A bluish tint to the lips or fingertips may appear, indicating low oxygen levels in the blood.
- Altered Mental Status: Severe hypercapnia can cause disorientation, agitation, or even loss of consciousness.
Symptoms of Hypercarbia
Hypercarbia, often used interchangeably with hypercapnia, also refers to elevated CO2 levels in the blood. The symptoms of hypercarbia are similar and include shortness of breath, headaches, and confusion. However, hypercarbia may also occur in non-medical contexts, such as exposure to high CO2 levels in confined spaces, which can lead to additional symptoms like dizziness or nausea.When to Seek Medical Attention
It is essential to seek medical attention if symptoms of hypercapnia or hypercarbia become severe or persistent. Warning signs that require immediate care include:- Severe Difficulty Breathing: If breathing becomes labored or shallow, it may indicate a critical level of CO2 retention.
- Altered Mental State: Confusion, extreme drowsiness, or unresponsiveness are signs of severe hypercapnia and require urgent evaluation.
- Cyanosis: A bluish discoloration of the lips, skin, or nails suggests dangerously low oxygen levels and should be treated as a medical emergency.
- Rapid Heart Rate or Chest Pain: These symptoms may indicate the body is under significant stress due to respiratory dysfunction.
Diagnosing Hypercapnia and Hypercarbia
Diagnosing conditions like hypercapnia and hypercarbia involves identifying elevated levels of carbon dioxide (CO2) in the blood and determining the underlying causes. Accurate diagnosis is essential for effective treatment and prevention of complications. Healthcare providers rely on a combination of clinical evaluations, diagnostic tests, and interpretation of results to confirm these conditions.Diagnostic Tests for Hypercapnia
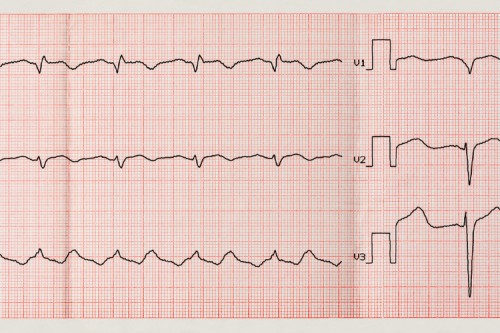
Hypercapnia, often associated with respiratory dysfunction, is typically diagnosed through specific tests that measure CO2 levels and assess lung function. The most common diagnostic tools include:- Arterial Blood Gas (ABG) Test: This is the gold standard for diagnosing hypercapnia. The test measures the levels of oxygen, carbon dioxide, and pH in the blood, providing a clear picture of respiratory efficiency. Elevated CO2 levels and a low pH indicate respiratory acidosis, a hallmark of hypercapnia.
- Capnography: This non-invasive test measures the concentration of CO2 in exhaled air, offering real-time data on respiratory function. It is often used in critical care settings or during surgeries to monitor patients at risk of CO2 retention.
- Pulmonary Function Tests (PFTs): These tests evaluate lung capacity and airflow, helping to identify conditions like chronic obstructive pulmonary disease (COPD) or restrictive lung diseases that may contribute to hypercapnia.
- Imaging Studies: Chest X-rays or CT scans can reveal structural abnormalities, such as lung damage or chest wall deformities, that impair breathing and lead to CO2 buildup.
Diagnostic Tests for Hypercarbia
Hypercarbia, a broader term that also refers to elevated CO2 levels, may require similar diagnostic approaches. However, it can also involve additional evaluations depending on the context, such as environmental exposure to CO2. Key diagnostic methods include:- Environmental CO2 Monitoring: In cases where hypercarbia is suspected due to external factors, such as poor ventilation in confined spaces, measuring ambient CO2 levels can help identify the source of exposure.
- Venous Blood Gas (VBG) Test: While less precise than an ABG test, a VBG test can provide an initial assessment of CO2 levels in the blood, particularly in non-critical situations.
- Clinical Observation: Symptoms like dizziness, nausea, or confusion in environments with high CO2 concentrations may prompt further testing to confirm hypercarbia.
Interpreting Test Results
Interpreting the results of diagnostic tests is a critical step in confirming hypercapnia or hypercarbia and determining the appropriate course of action. Key factors considered during interpretation include:- CO2 Levels: Elevated CO2 levels in an ABG or VBG test are the primary indicator of hypercapnia or hypercarbia. Normal arterial CO2 levels typically range between 35-45 mmHg, and values above this range suggest CO2 retention.
- pH Levels: A low blood pH (below 7.35) indicates acidosis, which often accompanies hypercapnia. This helps assess the severity of the condition and its impact on the body’s acid-base balance.
- Oxygen Levels: Low oxygen levels in the blood may point to coexisting hypoxemia, which can exacerbate symptoms and complicate treatment.
- Lung Function Metrics: Results from pulmonary function tests can reveal underlying respiratory conditions, such as COPD or restrictive lung disease, that contribute to CO2 retention.
- Imaging Findings: Structural abnormalities identified in chest X-rays or CT scans can provide additional context for the diagnosis and guide treatment planning.
Treatment Options for Hypercapnia
Hypercapnia, a condition characterized by elevated carbon dioxide (CO2) levels in the blood, requires a tailored approach to treatment based on its severity and underlying causes. Effective management involves immediate interventions, long-term strategies, and lifestyle adjustments to prevent recurrence and improve respiratory health.
Treatment for Hypercapnia
The primary goal of treating hypercapnia is to reduce CO2 levels in the blood and address the root cause of the condition. Common treatment options include:- Oxygen Therapy: Administering supplemental oxygen can help improve oxygenation in patients with respiratory distress. However, in conditions like COPD, oxygen therapy must be carefully monitored to avoid suppressing the respiratory drive.
- Non-Invasive Ventilation (NIV): Devices such as CPAP (continuous positive airway pressure) or BiPAP (bilevel positive airway pressure) are often used to support breathing. These methods help maintain open airways and enhance CO2 elimination without the need for invasive procedures.
- Mechanical Ventilation: In severe cases where non-invasive methods are insufficient, mechanical ventilation may be required. This involves intubation and the use of a ventilator to assist or take over the patient’s breathing.
- Bronchodilators and Medications: Medications like bronchodilators can relax airway muscles, improving airflow and reducing CO2 retention. Corticosteroids may also be prescribed to reduce inflammation in the airways.
- Treating Underlying Conditions: Addressing the root cause, such as infections, airway obstructions, or medication side effects, is critical for resolving hypercapnia.
Management Strategies
For individuals with chronic or recurring hypercapnia, long-term management strategies are essential to maintain respiratory health and prevent future episodes. These strategies include:- Pulmonary Rehabilitation: A comprehensive program that combines exercise, education, and breathing techniques to improve lung function and overall quality of life. Pulmonary rehabilitation is particularly beneficial for patients with chronic respiratory conditions like COPD.
- Home Ventilation Support: Some patients may require ongoing use of non-invasive ventilation devices, such as CPAP or BiPAP, to maintain adequate ventilation during sleep or periods of respiratory distress.
- Medication Management: Long-term use of prescribed medications, such as bronchodilators or anti-inflammatory drugs, can help control symptoms and prevent exacerbations.
- Regular Monitoring: Routine check-ups and blood gas tests are crucial for tracking CO2 levels and ensuring that treatment plans remain effective.
Lifestyle Changes and Prevention
Lifestyle modifications play a vital role in preventing hypercapnia and improving overall respiratory health. Key changes include:- Weight Management: For individuals with obesity hypoventilation syndrome, losing weight can significantly improve breathing mechanics and reduce CO2 retention. This may involve dietary changes, regular exercise, or bariatric surgery in severe cases.
- Smoking Cessation: Quitting smoking is critical for individuals with respiratory conditions, as it helps slow disease progression and improves lung function over time.
- Avoiding Sedatives: Medications that depress the central nervous system, such as opioids or benzodiazepines, should be used cautiously, as they can impair breathing and contribute to CO2 buildup.
- Maintaining Physical Activity: Regular exercise can strengthen respiratory muscles, improve lung capacity, and enhance overall health.
- Managing Underlying Conditions: Proper management of chronic conditions like COPD, asthma, or sleep apnea is essential for preventing hypercapnia. This includes adhering to prescribed treatments and attending regular medical appointments.
Risks Associated with Hypercapnia
Hypercapnia, a condition characterized by elevated carbon dioxide (CO2) levels in the blood, poses significant health risks if left untreated. These risks can range from short-term complications to long-term health consequences, depending on the severity and duration of the condition. Understanding the associated risks and contributing factors is essential for early intervention and prevention.Short-term Risks
In the short term, hypercapnia can lead to a variety of symptoms and complications that may escalate quickly if not addressed. These include:- Respiratory Distress: Elevated CO2 levels can impair the body’s ability to breathe effectively, leading to shortness of breath and labored breathing.
- Mental Confusion: High CO2 levels can affect brain function, causing confusion, dizziness, and difficulty concentrating. In severe cases, this may progress to drowsiness or even loss of consciousness.
- Headaches and Fatigue: The buildup of CO2 in the bloodstream can cause persistent headaches and a general feeling of exhaustion, making it difficult to perform daily activities.
- Increased Heart Rate: The body may respond to CO2 retention by increasing the heart rate in an attempt to improve oxygen delivery to tissues. This can place additional strain on the cardiovascular system.
- Cyanosis: A bluish tint to the lips, skin, or nails may develop, indicating low oxygen levels in the blood. This is a warning sign of severe respiratory dysfunction and requires immediate medical attention.
Long-term Risks
Chronic or untreated hypercapnia can lead to more serious long-term health complications, including:- Respiratory Acidosis: Prolonged CO2 retention can disrupt the body’s acid-base balance, leading to respiratory acidosis. This condition can impair organ function and increase the risk of systemic complications.
- Cardiovascular Strain: Chronic hypercapnia can place significant stress on the heart, potentially leading to conditions such as pulmonary hypertension or heart failure over time.
- Reduced Lung Function: Persistent CO2 buildup can exacerbate underlying respiratory conditions, such as chronic obstructive pulmonary disease (COPD), further reducing lung capacity and efficiency.
- Neurological Impairment: Long-term exposure to high CO2 levels can affect cognitive function, potentially leading to memory problems, difficulty concentrating, and other neurological issues.
- Increased Risk of Respiratory Failure: If left unmanaged, chronic hypercapnia can progress to respiratory failure, a life-threatening condition that requires immediate medical intervention.
Risk Factors for Hypercapnia
Certain factors increase the likelihood of developing hypercapnia, particularly in individuals with preexisting health conditions or lifestyle-related challenges. Key risk factors include:- Chronic Respiratory Conditions: Diseases like COPD, asthma, or interstitial lung disease can impair the lungs’ ability to expel CO2 effectively.
- Obesity Hypoventilation Syndrome: Excess body weight, particularly around the chest and abdomen, can restrict lung expansion and lead to shallow breathing, increasing the risk of CO2 retention.
- Sleep Apnea: Repeated interruptions in breathing during sleep can cause CO2 to accumulate over time, particularly in individuals with obstructive sleep apnea.
- Neuromuscular Disorders: Conditions such as muscular dystrophy or amyotrophic lateral sclerosis (ALS) can weaken the respiratory muscles, making it difficult to maintain normal breathing patterns.
- Sedative Medications: Drugs that depress the central nervous system, such as opioids or benzodiazepines, can slow breathing and contribute to CO2 retention.
- Smoking: Smoking damages lung tissue and reduces respiratory efficiency, increasing the risk of hypercapnia in individuals with chronic lung conditions.
Frequently Asked Questions
Q: What is hypercapnia?
A: Hypercapnia, sometimes referred to as hypercarbia, is a condition where carbon dioxide (CO2) levels in the bloodstream become abnormally high. This occurs when the lungs are unable to expel CO2 effectively, leading to respiratory acidosis and potential complications if left untreated.
Q: What are the symptoms of hypercapnia?
A: Symptoms of hypercapnia can include shortness of breath, shallow breathing, confusion, headaches, and dizziness. In more severe cases, it may lead to respiratory failure, where the body struggles to maintain proper oxygen and CO2 levels, requiring immediate medical attention.
Q: What causes hypercapnia?
A: Hypercapnia can result from various factors, including chronic lung diseases like chronic obstructive pulmonary disease (COPD), obesity hypoventilation syndrome, and conditions that impair normal breathing. Other contributing factors include respiratory acidosis and reduced blood flow to the lungs.
Q: How is hypercapnia diagnosed?
A: Hypercapnia is typically diagnosed through arterial blood gas (ABG) tests, which measure CO2 levels, oxygen levels, and blood pH. Symptoms such as difficulty breathing or confusion may prompt further evaluations, including lung function tests, to identify the underlying cause.
Q: What are the treatment options for hypercapnia?
A: Treatment for hypercapnia focuses on addressing the root cause and may include oxygen therapy, medications like bronchodilators to improve lung function, and non-invasive ventilation such as CPAP or BiPAP. In severe cases, mechanical ventilation may be necessary to stabilize the patient.
Q: What is the risk of hypercapnia?
A: The risk of hypercapnia is higher in individuals with chronic lung conditions, obesity, or disorders that impair normal breathing, such as sleep apnea. If left untreated, chronic hypercapnia can lead to complications like respiratory failure and long-term organ damage.
Q: How can one prevent hypercapnia?
A: Preventing hypercapnia involves managing underlying respiratory conditions, maintaining a healthy weight, and avoiding exposure to environments with high CO2 levels. Regular exercise, breathing exercises, and quitting smoking can also improve lung function and reduce the risk of CO2 retention.
Q: What are the signs and symptoms of severe hypercapnia?
A: Severe hypercapnia may present with symptoms such as extreme confusion, lethargy, rapid heart rate, and loss of consciousness. These signs indicate a medical emergency and require immediate intervention to prevent life-threatening complications.
Q: What is the outlook for someone with hypercapnia?
A: The prognosis for individuals with hypercapnia depends on the underlying cause and the effectiveness of the treatment plan. With proper management, many people can lead normal lives, but severe cases may require ongoing monitoring and long-term care to prevent complications.
Conclusion
Hypercapnia is a serious condition that requires prompt attention to prevent complications and restore proper respiratory function. By understanding its causes and symptoms, you can recognize the warning signs and seek appropriate treatment. Managing hypercapnia effectively is key to maintaining overall health and preventing long-term respiratory issues.












 Login with Google
Login with Google Login with Facebook
Login with Facebook