
An occlusive dressing is a vital tool in wound care, designed to create a seal over injuries to protect them from air, moisture, and contaminants. Commonly used for chest wounds, burns, and other serious injuries, occlusive dressings play a critical role in preventing infection and promoting healing. In this blog, we’ll explore what occlusive dressings are, how they work, and when to use them for effective wound management.
Understanding Occlusive Dressings
Occlusive dressings are a vital component in wound care, designed to create a sealed environment that promotes healing by protecting the wound from external contaminants and maintaining moisture. These dressings are widely used in both medical and home care settings for various types of wounds, ranging from minor cuts to more severe injuries.What is an Occlusive Dressing?
 An occlusive dressing is a type of wound covering that forms a complete seal over the affected area, preventing air, water, and bacteria from entering. Unlike traditional gauze or bandages, occlusive dressings are designed to maintain a moist environment, which is essential for faster and more effective wound healing. This moisture retention helps to reduce scab formation, promote cell regeneration, and minimize scarring.
These dressings are particularly beneficial for wounds that require a sterile environment, such as surgical incisions, burns, or pressure ulcers. By creating a barrier against external contaminants, occlusive dressings significantly lower the risk of infection while also providing a cushioning effect to protect the wound from further trauma.
An occlusive dressing is a type of wound covering that forms a complete seal over the affected area, preventing air, water, and bacteria from entering. Unlike traditional gauze or bandages, occlusive dressings are designed to maintain a moist environment, which is essential for faster and more effective wound healing. This moisture retention helps to reduce scab formation, promote cell regeneration, and minimize scarring.
These dressings are particularly beneficial for wounds that require a sterile environment, such as surgical incisions, burns, or pressure ulcers. By creating a barrier against external contaminants, occlusive dressings significantly lower the risk of infection while also providing a cushioning effect to protect the wound from further trauma.
Types of Occlusive Dressings
Occlusive dressings come in various forms, each tailored to specific wound care needs. Below are some of the most common types:- Hydrocolloid Dressings: These are made of a gel-forming material that absorbs wound exudate while maintaining a moist environment. They are ideal for shallow wounds, minor burns, and pressure ulcers.
- Transparent Film Dressings: Thin and flexible, these dressings are often used for superficial wounds or as a secondary dressing. They allow for easy monitoring of the wound without removal.
- Foam Dressings: Designed for wounds with moderate to heavy exudate, foam dressings provide excellent absorption while keeping the wound moist. They are commonly used for surgical wounds and ulcers.
- Alginate Dressings: Derived from seaweed, alginate dressings are highly absorbent and suitable for wounds with significant drainage. They are often used for deeper wounds or those with irregular shapes.
- Hydrogel Dressings: These dressings are water-based and provide cooling relief for dry or painful wounds, such as burns or radiation injuries.
Materials Used in Occlusive Dressings
Occlusive dressings are made from a variety of materials, each chosen for its unique properties that contribute to effective wound care. Some of the most commonly used materials include:- Polyurethane: This material is often used in transparent film dressings due to its flexibility, durability, and ability to create a waterproof barrier.
- Hydrocolloids: These are composed of substances like gelatin, pectin, or carboxymethylcellulose, which form a gel when in contact with wound exudate, aiding in moisture retention.
- Foam: Polyurethane foam is commonly used in foam dressings for its excellent absorbent properties and cushioning effect.
- Alginates: Derived from seaweed, alginate fibers are highly absorbent and form a gel-like substance when exposed to wound fluid, making them ideal for heavily draining wounds.
- Hydrogels: These are water-based or glycerin-based materials that provide hydration and cooling, making them suitable for dry or painful wounds.
The Role of Occlusive Dressings in Wound Healing
Enhanced Moisture Retention
Occlusive dressings play a pivotal role in maintaining an optimal environment for wound healing by retaining moisture. Unlike traditional bandages, these dressings create a sealed barrier over the wound, preventing the evaporation of natural fluids. This moist environment is crucial as it accelerates the migration of skin cells, promotes the formation of new tissue, and reduces the risk of scab formation, which can delay healing. Additionally, the retained moisture helps dissolve dead tissue, making it easier for the body to naturally remove debris. By keeping the wound hydrated, occlusive dressings also minimize the risk of cracking or reopening, which is common with dry wounds. Moreover, the moisture retention provided by these dressings reduces the need for frequent dressing changes. This not only saves time and resources but also minimizes the disruption to the wound site, allowing the healing process to proceed uninterrupted. For individuals with chronic wounds or those prone to slow healing, such as diabetic patients, this feature is particularly beneficial.
Protection from Contamination
One of the primary advantages of occlusive dressings is their ability to shield wounds from external contaminants. The sealed barrier prevents bacteria, dirt, and other harmful particles from entering the wound, significantly reducing the risk of infection. This is especially important for wounds in areas exposed to frequent contact with the environment, such as hands or feet. By keeping the wound sterile, occlusive dressings create a safer healing environment and lower the chances of complications. In addition to blocking external contaminants, these dressings also help maintain a stable temperature around the wound. A consistent temperature is essential for cellular activity and tissue regeneration, both of which are critical for effective healing. The protective layer also guards against mechanical irritation, such as friction from clothing or accidental bumps, which can aggravate the wound and prolong recovery.Reduction of Pain and Discomfort
Occlusive dressings are designed to provide a soothing effect, reducing pain and discomfort associated with wounds. By maintaining a moist environment, they prevent the wound from drying out, which is a common cause of pain due to tight, cracked skin. The cushioning effect of these dressings also protects the wound from external pressure and friction, offering relief to patients who experience discomfort during daily activities. Furthermore, the reduced need for frequent dressing changes contributes to less pain. Traditional dressings often stick to the wound, causing discomfort when removed. In contrast, occlusive dressings are less likely to adhere to the wound bed, making the removal process gentler and less painful. This feature is particularly valuable for individuals with sensitive skin or those recovering from surgical procedures.Application of Occlusive Dressings in Wound Management
Occlusive dressings play a pivotal role in modern wound care by creating a moist environment that promotes faster healing. These dressings are designed to seal the wound completely, preventing external contaminants like bacteria and debris from entering. By maintaining a moist environment, occlusive dressings facilitate the natural healing process, reduce the risk of infection, and minimize scarring. They are particularly effective for wounds that require prolonged healing, such as pressure ulcers, burns, and surgical incisions. Additionally, these dressings help regulate the temperature around the wound, which further accelerates tissue repair. However, it is essential to understand the specific needs of each wound to determine whether an occlusive dressing is the best option.
Choosing the Right Dressing for Different Wounds
Selecting the appropriate dressing depends on the type, size, and condition of the wound. For shallow wounds with minimal exudate, thin film dressings are often sufficient as they provide a protective barrier without excessive bulk. On the other hand, hydrocolloid dressings are ideal for wounds with moderate exudate, as they absorb fluid while maintaining a moist environment. For heavily exuding wounds, foam dressings are a better choice due to their superior absorption capacity. Chronic wounds, such as diabetic ulcers, may benefit from advanced occlusive options like alginate dressings, which are derived from seaweed and promote faster healing. It is also crucial to consider patient-specific factors, such as allergies, skin sensitivity, and mobility, when choosing a dressing. Consulting a healthcare professional can ensure the most effective treatment plan.Step-by-Step Guide to Applying Occlusive Dressings
- Prepare the Wound Area: Begin by cleaning the wound thoroughly with a saline solution or an antiseptic to remove debris and reduce the risk of infection. Pat the surrounding skin dry with a sterile cloth.
- Select the Appropriate Dressing: Choose a dressing that matches the wound's size and exudate level. Ensure the dressing is large enough to cover the wound and extend slightly onto the surrounding healthy skin.
- Apply the Dressing: Carefully place the occlusive dressing over the wound, ensuring it adheres securely to the skin. Avoid stretching the dressing, as this can cause discomfort or damage to the skin.
- Secure the Edges: Use medical tape or an adhesive border to seal the edges of the dressing. This step is crucial to prevent contaminants from entering and to maintain the moist environment.
- Monitor and Replace: Check the dressing regularly for signs of leakage or saturation. Replace it as needed, typically every 2-3 days, or as recommended by a healthcare provider.
Common Mistakes to Avoid
- Using the Wrong Dressing Type: Applying a dressing that does not match the wound's needs can delay healing or worsen the condition. For example, using a non-absorbent dressing on a heavily exuding wound can lead to maceration.
- Improper Wound Cleaning: Failing to clean the wound thoroughly before applying the dressing increases the risk of infection and complications.
- Overlooking Skin Preparation: Neglecting to dry the surrounding skin can cause the dressing to lose adhesion, leading to gaps that allow bacteria to enter.
- Changing Dressings Too Frequently: While it is important to monitor the wound, changing the dressing too often can disrupt the healing process and irritate the skin.
- Ignoring Signs of Infection: Redness, swelling, or an unusual odor around the wound may indicate an infection. If these signs are present, consult a healthcare professional immediately.
Specific Uses of Occlusive Dressings
Occlusive dressings are a critical component in medical care, particularly in emergency and trauma situations. These specialized dressings are designed to create an airtight seal over wounds, preventing air, moisture, and contaminants from entering the affected area. Their unique properties make them indispensable in managing specific injuries, such as chest wounds, burns, and open fractures. By maintaining a sterile environment and promoting optimal healing conditions, occlusive dressings play a vital role in reducing the risk of infection and complications. Below, we explore their specific applications in various medical scenarios.Occlusive Dressings for Chest Wounds
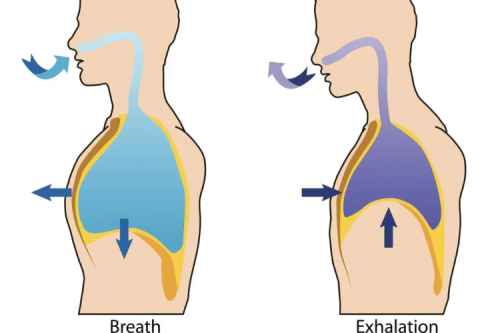
Chest wounds, especially those classified as open or "sucking" chest wounds, require immediate attention to prevent life-threatening complications like tension pneumothorax. Occlusive dressings are particularly effective in these cases because they seal the wound, preventing air from entering the pleural cavity. This helps stabilize the patient and reduces the risk of lung collapse. When applying an occlusive dressing to a chest wound, it is essential to ensure a proper seal. Typically, the dressing is secured on three sides, leaving one side open to act as a vent. This venting mechanism allows trapped air to escape while preventing additional air from entering. Materials such as petroleum gauze, plastic wrap, or specialized chest seals are commonly used for this purpose. The effectiveness of the dressing depends on its ability to adhere securely to the skin, even in the presence of blood or other fluids.Utilizing Hyfin Chest Seal for Open Chest Wounds
The Hyfin Chest Seal is a widely recognized product explicitly designed for managing open chest wounds. This advanced occlusive dressing features a strong adhesive and a built-in venting system, making it highly effective in emergency situations. Its compact design and ease of application make it a preferred choice for first responders and military personnel. To use the Hyfin Chest Seal, first clean the surrounding area to ensure proper adhesion. Then, peel off the backing and apply the seal directly over the wound, pressing firmly to create an airtight seal. The venting system allows air and fluids to escape, reducing the risk of tension pneumothorax. Additionally, the Hyfin Chest Seal is designed to work in extreme conditions, including wet or bloody environments, ensuring reliable performance when it matters most.Occlusive Dressings in First Aid Scenarios
In first aid scenarios, occlusive dressings are invaluable for managing a variety of injuries. Their versatility allows them to be used for wounds that require an airtight seal, such as chest injuries, or for protecting burns and abrasions from external contaminants. In emergency kits, occlusive materials like plastic wrap or adhesive dressings are often included due to their practicality and effectiveness. For chest wounds, as mentioned earlier, occlusive dressings can be improvised using available materials if commercial options are not accessible. For example, a piece of plastic wrap secured with tape can serve as a temporary solution. In the case of burns, occlusive dressings help retain moisture and create a barrier against infection, promoting faster healing. Their application in first aid underscores their importance in both professional medical settings and everyday emergencies.Contraindications and Considerations for Occlusive Dressings
Occlusive dressings are widely used in wound care due to their ability to create a moist environment that promotes healing. However, they are not suitable for every situation, and understanding their contraindications is crucial for effective treatment. These dressings should not be used on infected wounds, as the sealed environment can exacerbate bacterial growth. Additionally, wounds with heavy exudate may not benefit from occlusive dressings, as the accumulation of fluid can lead to maceration of the surrounding skin. Patients with fragile or sensitive skin, such as those with eczema or dermatitis, may also experience irritation or adverse reactions when using these dressings. It is essential to assess the patient’s overall health and the specific characteristics of the wound before choosing an occlusive dressing. For example, individuals with compromised immune systems or conditions like diabetes may require alternative wound care methods to prevent complications. Always consider the patient’s medical history and consult with a healthcare professional if there is any uncertainty about the suitability of occlusive dressings.
When Not to Use an Occlusive Dressing
There are specific scenarios where occlusive dressings should be avoided to prevent further harm. These include:- Infected Wounds: Occlusive dressings can trap bacteria and create an environment conducive to infection, worsening the wound condition.
- Deep or Puncture Wounds: These types of wounds require drainage to prevent abscess formation, which occlusive dressings may hinder.
- Allergic Reactions: Some patients may be allergic to the materials used in occlusive dressings, leading to skin irritation or rashes.
- Burns with Heavy Exudate: Burns that produce significant fluid may not heal effectively under an occlusive dressing, as the excess moisture can damage surrounding tissues.
Identifying Complications in Wound Healing
Complications in wound healing can arise due to improper use of dressings or underlying health issues. Common signs of complications include increased redness, swelling, or pain around the wound site. The presence of foul-smelling discharge or a sudden increase in exudate may indicate an infection. Additionally, delayed healing or the appearance of necrotic tissue can signal that the current treatment approach is ineffective. Healthcare providers should monitor wounds regularly to identify these warning signs early. If complications are suspected, it may be necessary to change the dressing type, adjust the treatment plan, or prescribe antibiotics to address infections. Patient education is also vital, as individuals should be aware of what to look for and when to seek medical attention.Consulting Healthcare Professionals for Wound Care
When dealing with complex wounds or uncertain treatment options, consulting a healthcare professional is essential. Medical experts can provide a thorough assessment of the wound and recommend the most appropriate dressing and care regimen. They can also identify underlying conditions, such as diabetes or vascular issues, that may impede healing. Patients should not hesitate to seek professional advice if they notice signs of infection, persistent pain, or delayed healing. Regular follow-ups with a healthcare provider can ensure that the wound is progressing as expected and that any necessary adjustments to the treatment plan are made promptly.FAQ About Occlusive Dressings
Q: What is an occlusive dressing?
A: An occlusive dressing is a specialized wound covering that creates a sealed barrier to protect the wound from moisture, bacteria, and other external contaminants. By maintaining a moist environment, these dressings promote faster healing and are particularly effective for superficial wounds, burns, and minor lacerations.
Q: How do occlusive dressings work in wound care?
A: Occlusive dressings work by sealing the wound completely, preventing external contaminants like bacteria and dirt from entering. They retain wound exudate, which helps create a moist environment conducive to tissue regeneration. This is especially beneficial for wounds such as burns, abrasions, and surgical incisions.
Q: What are the benefits of using hydrocolloid dressings?
A: Hydrocolloid dressings offer several benefits, including their ability to absorb wound exudate while maintaining a moist environment that accelerates healing. They are non-adherent to the wound bed, making removal painless and reducing the risk of damaging new tissue or causing unnecessary scarring.
Q: Can occlusive dressings prevent infection?
A: Yes, occlusive dressings act as a barrier against bacteria and other pathogens, significantly reducing the risk of infection. This is particularly important for open wounds, burns, and surgical sites, where the risk of contamination is high.
Q: What types of wounds benefit from occlusive dressings?
A: Occlusive dressings are suitable for a variety of wounds, including superficial cuts, minor burns, abrasions, and surgical incisions. They are especially effective for wounds that produce moderate to low levels of exudate, as they help maintain optimal moisture levels for healing.
Q: How do occlusive dressings affect wound healing?
A: Occlusive dressings positively impact wound healing by creating a moist environment that promotes cell growth and tissue repair. However, improper use, such as leaving the dressing on for too long or using it on inappropriate wound types, can lead to complications like infection or delayed healing.
Q: Are there any contraindications for using occlusive dressings?
A: Yes, occlusive dressings are not recommended for heavily exuding wounds, infected wounds, or those with necrotic tissue. In such cases, alternative dressings like alginate or gauze may be more effective in managing the wound and preventing complications.
Q: What materials are occlusive dressings made from?
A: Occlusive dressings are made from materials like polyurethane, polyethylene, hydrocolloids, and hydrogels. These materials are designed to create a protective barrier while allowing some moisture vapor transmission, which helps maintain a healthy wound environment.
Q: How should occlusive dressings be applied?
A: To apply an occlusive dressing, first clean and dry the surrounding skin thoroughly. Place the dressing directly over the wound, ensuring it adheres securely to create a complete seal. Follow the manufacturer’s instructions or consult a healthcare professional for proper application techniques to maximize effectiveness.
Q: What should I do if an occlusive dressing is not adhering properly?
A: If an occlusive dressing is not adhering well, it could be due to excessive moisture or improper application. Try using a self-adhesive dressing or applying additional adhesive strips to secure it. If the issue persists, consult a healthcare provider for alternative dressing options or recommendations.
Conclusion
Occlusive dressings are a crucial component of advanced wound care, providing protection and facilitating the healing process. By understanding their purpose and proper application, you can ensure better outcomes for injuries that require a sealed environment. Whether for emergencies or routine care, occlusive dressings are a reliable solution for safeguarding wounds and promoting recovery.












 Login with Google
Login with Google Login with Facebook
Login with Facebook