
If you’ve ever taken a CPR course, you’ve likely been told to check for a pulse before starting chest compressions. But in a high-stress emergency, this step can feel confusing—should you spend precious seconds feeling for a pulse, or should you begin CPR immediately?
While the average person may assume that CPR is always necessary in an unconscious patient, medical professionals and trained responders know that pulse checks are critical. A weak or absent pulse confirms cardiac arrest, whereas a detectable pulse means CPR could do more harm than good.
Let’s explore why checking for a pulse is essential, how to do it correctly, and when exceptions apply.
Why Pulse Checks Are Critical During CPR?
The Importance of Accurate Pulse Assessment
Assessing whether a pulse is present or absent is vital for healthcare providers and trained responders when performing CPR. An accurate pulse check ensures that life-saving measures are appropriate and effective. Misidentifying the presence or absence of a pulse can have severe consequences, potentially leading to delays in care or unnecessary chest compressions.
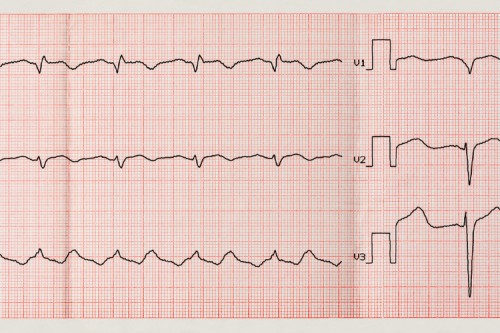
Pulse assessments allow responders to gauge the effectiveness of cardiopulmonary resuscitation and monitor signs of recovery. The carotid artery is often the preferred site for pulse checks for trained individuals due to its reliability and accessibility in emergencies. However, even with training, assessing for a pulse can be challenging under stressful conditions, particularly when adrenaline is high, time is limited, and the patient’s condition is critical.
This is why adhering to evidence-based guidelines, including limiting pulse checks to 10 seconds or less, is paramount. Rapid and accurate identification minimizes interruptions in chest compressions, critical for optimizing blood flow to vital organs like the brain and heart. Research consistently supports the importance of maintaining uninterrupted compressions; therefore, the speed and precision of pulse checks become even more significant.
How Pulse Checks Guide CPR Decisions
Pulse checks are more than a procedural step; they guide every major decision during CPR. For example, pulse assessments help determine whether to start, continue, or pause chest compressions. If there is no detectable pulse and the patient remains unresponsive, immediate chest compressions should be initiated to maintain blood circulation. Conversely, if a pulse is present, chest compressions may be paused to avoid causing unnecessary trauma or complications, such as rib fractures or internal injuries.
Additionally, pulse checks are instrumental in monitoring patient response to advanced interventions such as defibrillation, medication administration, or advanced airway management. For instance, after a shock from a defibrillator, checking for a pulse helps determine whether electrical therapy restored spontaneous circulation. This assessment allows providers to decide the following steps, including repeating defibrillation, modifying medications, or continuing CPR.
It is crucial to recognize that timing and technique are everything during pulse checks. Extended delays in resuming compressions—even by a few seconds during an unnecessary or prolonged pulse check—can significantly reduce a patient’s chance of survival. This is why teams work together to communicate effectively, ensuring each step of the CPR process is timed for maximum efficiency.
Pulse checks also guide post-resuscitation care. Once spontaneous circulation (ROSC) is restored, pulse monitoring remains essential to evaluating the patient’s cardiovascular stability and determining the transition to advanced life support measures. By acting as a continuous guide, pulse checks help providers focus on delivering the right interventions at the right time, improving the chances of survival and recovery.
Understanding the Role of Pulse Checks in Cardiac Emergencies
Pulse checks are a vital part of cardiac emergency protocols. They play a critical role in assessing a patient’s circulatory status and guiding the steps of life-saving interventions like CPR. These checks provide medical responders with essential information about a patient’s condition by ensuring proper blood circulation and identifying signs of adequate resuscitation.
Pulse Checks and Blood Circulation
The pulse represents the rhythmic expansion and contraction of arteries as the heart pumps blood throughout the body. It provides a real-time indicator of blood circulation and heart function. During cardiac emergencies, such as a cardiac arrest, assessing a patient’s pulse can reveal whether the heart has stopped beating effectively or entirely.
Why Blood Circulation Matters in Emergencies
Blood circulation delivers oxygen and nutrients to the body’s organs and tissues while removing waste products. When the heart’s ability to pump blood is compromised, this vital process is interrupted. If not addressed quickly, this can lead to tissue damage, organ failure, and death. The role of pulse checks is directly tied to detecting this interruption and implementing immediate corrective measures.
Assessing the Pulse
Healthcare providers and trained responders use key pulse points, such as the carotid artery in the neck or the femoral artery in the groin, to assess emergency circulation. These pulse sites are chosen because they are closer to the heart and provide a clearer sense of blood flow, especially when peripheral circulation may be weak or absent. The absence of a palpable pulse often indicates either no blood flow or insufficient cardiac output, calling for prompt action.
When to Perform a Pulse Check During CPR
CPR (cardiopulmonary resuscitation) is the primary life-saving intervention for patients in cardiac arrest. It involves manual chest compressions to maintain blood flow to vital organs until the heart can be restarted. Pulse checks during CPR help evaluate whether resuscitation efforts are practical or if additional steps are needed.
When Pulse Checks Are Performed
According to CPR guidelines, pulse checks are performed at precise intervals during resuscitation efforts:
-
Before Starting CPR A pulse check is conducted to confirm cardiac arrest. CPR must begin immediately if no pulse is detected within 10 seconds, as delays could reduce survival chances.
-
During Rhythmic Restorative Efforts Pulse checks may be conducted when there is a potential return of spontaneous circulation (ROSC). This can occur after defibrillation or if the patient shows signs such as movement or breathing. Confirming a detectable pulse is critical before stopping compressions to avoid pauses in treatment.
-
After ROSC Is Achieved Once signs of circulation return, pulse checks are used to monitor the patient’s condition and ensure stable blood flow until further medical management can occur.
Avoiding Inefficient Pulse Checks During CPR
Interruptions in chest compressions to check the pulse can decrease the overall effectiveness of CPR. For this reason, many guidelines emphasize minimizing interruptions to no more than 10 seconds. Emergency responders are trained to integrate pulse checks as seamlessly as possible within the rhythm of resuscitation.
Challenges in Detecting a Pulse
Detecting a pulse during an emergency can sometimes be challenging, especially in high-stress situations. Thick chest walls, peripheral vascular issues, or faint cardiac output can make the pulse difficult to palpate. Advanced tools like Doppler devices or capnography might be used in some cases to confirm circulation, especially in hospital settings.
Pulse checks are essential for determining the patient’s circulatory status and ensuring proper management during cardiac emergencies. By understanding when and how to perform them effectively, emergency responders can optimize the chances of survival and recovery for individuals in critical situations. Coordination, minimal interruptions, and precise assessment are cornerstones of this crucial life-saving skill.
Key Pulse Points for Different Age Groups
Carotid Artery for Adults and Children
The carotid artery is one of the most reliable pulse points in adults and children. It is on either side of the neck, adjacent to the trachea. This site is preferred because the carotid artery provides a strong and consistent pulse, making it easy to locate even during emergencies.
When checking the carotid pulse, gently place your index and middle fingers on the neck, avoiding excessive pressure. Pressing too hard can obstruct blood flow, especially in vulnerable individuals. This pulse point is most commonly used in situations like cardiac arrest, as it quickly measures heart function. However, routine checks are not ideal for children who may feel discomfort.
Brachial Artery for Infants
The brachial artery is the go-to pulse point for infants. This artery is located on the inside of the upper arm, between the bicep and tricep muscles. Infants are chosen for the brachial pulse due to their small anatomy and their inability to use other adult-preferred sites effectively.
To find the brachial pulse, position the infant’s arm with the palm facing upward, then place two fingers along the inside of the arm close to the elbow. This pulse point is particularly valuable during neonatal resuscitation or when assessing circulation. Since infants cannot verbalize distress, monitoring the brachial pulse is crucial for ensuring adequate blood flow and oxygen delivery.
Radial and Pedal Pulse: When and Why to Use Them
Radial Pulse
The radial artery on the thumb side of the wrist is one of the most commonly used pulse points for routine health checks. This site offers a convenient way to assess heart rate and circulation in older children, adults, and even cooperative younger children.
Radial pulses are ideal for non-emergency situations, such as monitoring heart rate during physical activity or assessing general health in clinical settings. However, in cases of shock or poor peripheral blood flow, the radial pulse may weaken, and other sites, like the carotid artery, may be preferred.
Pedal Pulse
The pedal pulse, found on the top of the foot, is primarily used to assess circulation in the lower extremities. It helps detect conditions such as peripheral arterial disease or monitor blood flow after specific surgical procedures.
To locate the pedal pulse, place fingers over the dorsalis pedis artery, which runs along the top of the foot between the first and second metatarsal bones. This pulse point is typically reserved for specific medical evaluations rather than general heart rate checks. It is most often used in adults and older children, as locating this pulse in infants can be challenging due to their smaller anatomy and less defined landmarks.
Step-by-Step Guide to Checking a Pulse During CPR
During CPR, checking for a pulse is crucial to determine whether the heart is still pumping blood effectively. Performing this task correctly can help guide your subsequent actions, whether continuing CPR or monitoring for signs of spontaneous circulation. This guide will walk you through the essentials of locating a pulse, how long to check, and what to do if a pulse isn’t detected.
Locating the Pulse: Carotid, Brachial, and Radial
Knowing where to check for a pulse is essential; your chosen location will depend on the patient’s age and physical condition. Below, we cover identifying the carotid, brachial, and radial pulses.
Carotid Pulse
The carotid artery is the most commonly checked location for a pulse during CPR, particularly for adults. It is a large artery located on either side of the neck. Here's how to find it:
- Place two fingers (index and middle) on the individual’s trachea (windpipe).
- Slide your fingers laterally (toward the side of the neck) until they rest in the groove between the trachea and the muscle on the neck.
- Press gently to feel for a pulse. Apply only enough pressure to detect movement; pressing too hard can impede blood flow.
Brachial Pulse
The brachial artery is typically used for infants under one year old because it is easier to palpate in smaller individuals. To find the brachial pulse:
- Lay the infant on their back and extend one arm slightly out.
- Use two fingers to palpate along the inside of the upper arm, midway between the shoulder and the elbow.
- Apply gentle pressure until you detect a pulsing sensation.
Radial Pulse
The radial artery on the wrist is another accessible spot for checking a pulse. While it is less commonly used in emergencies, it can be an alternative for conscious patients. To locate it:
- Turn the patient’s palm upward.
- Place two fingers on the thumb side of the wrist, just below the base of the thumb.
- Press lightly until you detect a pulse.
How Long to Check for a Pulse
Timing is vital when checking for a pulse during CPR. The standard recommendation is to spend no more than 10 seconds assessing for a pulse. This time frame ensures you act quickly, since any delays can reduce the chances of survival. Follow these steps:
- Once the patient shows no signs of responsiveness and breathing is absent or abnormal (like gasping), begin checking for a pulse.
- Position your fingers correctly based on the pulse site (carotid, brachial, or radial).
- Count silently to 10 as you check for any rhythmic pulsation.
If no pulse is identified within this period, proceed with CPR immediately. Prolonged pauses while trying to detect a pulse can waste precious seconds, hindering the chance of successful resuscitation.
What to Do If You Can’t Find a Pulse
Finding no pulse is a critical determination in CPR. It signals that the heart is not effectively pumping blood and that immediate intervention is required. Here’s what you should do:
-
Start Chest Compressions Immediately Begin high-quality chest compressions at a rate of 100-120 compressions per minute. Push hard and fast, allowing the chest to recoil between compressions fully. For adults, use the heel of your hand; for infants, use two fingers or two thumbs, depending on the technique.
-
Follow CPR Protocols Depending on your training level, alternate between chest compressions and rescue breaths at a 30:2 ratio, or provide compressions only if breathing assistance is not feasible. When it becomes available, use an automated external defibrillator (AED) and follow the device prompts.
-
Reassess Regularly After every two minutes of CPR or after an AED shock, pause briefly to reassess for a pulse and signs of breathing. Limit this interruption to 10 seconds. If no pulse is found, resume chest compressions without delay.
-
Activate Emergency Services Ensure someone has called emergency responders. If you are alone and unable to find a pulse, call 911 immediately or use speakerphone to communicate with emergency services while maintaining compressions.
-
Provide Care Until Help Arrives Continue performing CPR until advanced medical personnel arrive and take over, or until the individual starts to regain spontaneous circulation (indicated by movement or a steady pulse).
By following these steps, you can effectively respond to a cardiac emergency, giving the individual the best chance of survival.
Understanding how to check a pulse during CPR is fundamental for anyone providing first aid. Proper technique, speed, and guideline adherence can make all the difference during a critical situation. Remember, prioritizing compressions can save a life if you're unsure or unable to locate a pulse.
Common Mistakes to Avoid When Checking a Pulse
The Importance of Accurate Pulse Checks
Checking a pulse is a crucial skill in assessing someone's health, whether in a medical emergency or routine health monitoring. A pulse reflects the heart's rhythm, rate, and strength, providing valuable insights into cardiovascular health. However, even small mistakes can lead to inaccurate readings, which might result in misinterpretation and delayed responses during critical situations. Below, we’ll discuss some common mistakes people make when checking a pulse and how to avoid them to ensure precise and practical evaluations.
Spending Too Much Time on Pulse Checks
Why Timing Matters
When checking a pulse, efficiency is just as important as accuracy. Spending too much time locating or measuring the pulse can waste precious seconds in emergencies. The goal is to quickly identify the rate, rhythm, and any abnormalities within a reasonable timeframe. Delays in pulse checks could interfere with your ability to administer prompt care, such as CPR or defibrillation, if necessary.
How to Avoid This Mistake
To prevent spending too much time on this step, practice locating common pulse points like the carotid artery (neck) or radial artery (wrist). Familiarize yourself with the correct positioning and amount of pressure to apply. Once you've located the pulse, count the beats for 15-30 seconds and multiply appropriately to calculate the beats per minute, depending on the situation's urgency. Prioritize confidence and speed through regular practice.
Implications of Prolonged Pulse Checks
If too much time is spent, you may risk delaying critical interventions. Particularly in emergencies, hesitation or uncertainty could compromise patient outcomes. Developing this skill ensures you can transition seamlessly into the following necessary action.
Using the Thumb Instead of Fingers
The Problem with Using Your Thumb
Using your thumb to check someone's pulse is one of the most common errors people make, especially for those who are inexperienced. The issue lies in the anatomy of the thumb itself. The thumb contains its own pulse point, known as the princeps pollicis artery, which can easily interfere with your ability to feel the pulse of the person you're assessing. This can result in confusing or inaccurate readings.
The Correct Technique
Always use your index and middle fingers to check for a pulse. These fingers are more sensitive and lack the interference of a distinct pulse point. Place them on the designated pulse site and apply light pressure until you feel the rhythmic beating. Avoid pressing too hard, as this can obstruct the blood flow and make the pulse more challenging to detect.
Why It Matters
Misreading the pulse due to thumb interference might lead to incorrect heart rate or rhythm conclusions. For example, you could mistakenly assess a pulse as irregular or weak when it’s not. Ensuring accurate technique significantly reduces this risk.
Misinterpreting Weak or Irregular Pulses
Understanding Normal vs. Abnormal Pulses
Interpreting pulses can sometimes be challenging, especially when weak, irregular, or faint. A weak pulse may feel faint and hard to detect, while an irregular pulse may skip beats or vary in rhythm. Both may indicate underlying medical conditions, such as arrhythmias, shock, or dehydration. However, inexperienced individuals may mistake these characteristics, leading to missed or mismanaged health concerns.
Tips for Accurate Interpretation
- Practice Consistency - Regularly practice detecting regular pulses to develop a baseline understanding of average rhythms and strengths.
- Compare to Other Sites - If one pulse point feels weak, assess different sites, such as switching from the wrist to the neck. Weak pulses might vary by location due to issues like poor circulation.
- Time Your Assessment - When identifying irregularities, spend a full minute measuring to account for inconsistencies and better evaluate abnormalities.
Medical Implications
Misinterpreting weak or irregular pulses can have serious consequences, as these findings often point to conditions that require urgent care. For example, a weak pulse might suggest poor blood flow, potentially signaling shock or cardiac arrest, while an irregular pulse might indicate atrial fibrillation. Recognizing these signs early can facilitate faster medical intervention and prevent further complications.
Pulse checks are a straightforward but essential skill in evaluating heart health and responding to emergencies. However, even minor missteps can lead to significant consequences, such as spending too much time identifying a pulse, using the thumb instead of fingers, or failing to interpret weak or irregular pulses correctly. You can ensure adequate and reliable pulse assessments by understanding these common mistakes, practicing proper techniques, and refining your accuracy over time.
What to Do After Checking the Pulse?
Checking someone's pulse can be crucial in understanding their condition, particularly during an emergency. Knowing what steps to take afterward could significantly affect their outcome. Follow specific actions based on whether a pulse is detected or not, and ensure continuous monitoring of their vital signs.
Actions If a Pulse Is Detected
If you find a pulse, it indicates that the person's heart is still functioning. However, this does not necessarily mean they are out of danger. Here's what to do:
-
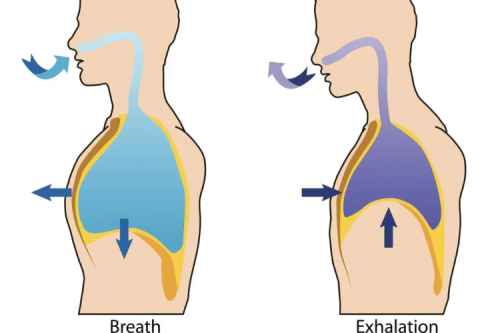
Assess Breathing Check if the individual is breathing normally. Look for regular chest movements, listen for airflow, and feel for breath against your cheek. If they are breathing adequately, position them in the recovery position (on their side) to keep their airway open and prevent choking.
-
Monitor Signs of Life Continue to observe the individual's breathing and pulse closely while waiting for emergency services to arrive. Deterioration in their condition can occur rapidly, so stay attentive.
-
Provide Comfort and Reassurance If the person is conscious, speak to them calmly. Explain that help is on the way and try to keep them as still and comfortable as possible to avoid unnecessary movement.
-
Manage Other Potential Issues Look for signs of bleeding, injury, or shock, and take appropriate actions as needed. For instance, apply pressure to control bleeding or cover them with a blanket to maintain body warmth in case of shock.
Actions If No Pulse Is Detected
The absence of a pulse is a clear emergency and requires immediate intervention. Here are the necessary steps:
-
Begin Cardiopulmonary Resuscitation (CPR) Initiate chest compressions without delay. Place your hands, one over the other, on the center of the person's chest, and push hard and fast at 100–120 compressions per minute. Ensure the chest fully recoils between compressions for maximum effectiveness.
-
Rescue Breaths (If Trained) If you are trained in CPR, which includes rescue breaths, alternate 30 chest compressions with two rescue breaths. Tilt the person's head back, lift their chin, and seal your mouth over theirs to deliver breaths while watching for the chest to rise.
-
Use an Automated External Defibrillator (AED) If available, retrieve and use an AED as soon as possible. Please turn it on, follow the voice prompts, and attach the pads as directed. The device will analyze the heart rhythm and advise if a shock should be delivered.
-
Call Emergency Services Ensure emergency medical services have been contacted. If someone else is nearby, delegate this task while you continue CPR until professional help arrives or the AED indicates you can pause.
Monitoring Pulse and Breathing Continuously
Regardless of whether a pulse is detected, ongoing monitoring of the individual’s pulse and breathing is essential. Here’s how to do this effectively:
-
Reassess Regularly If performing CPR, pause every two minutes to check for the return of a pulse and breathing. Pay close attention to any changes and adjust accordingly.
-
Avoid Interruptions Minimize interruptions during CPR. If someone else is present, take turns to ensure compressions remain consistent and adequate.
-
Be Prepared for Changes The person’s condition may suddenly improve or worsen. Remain vigilant and ready to adjust your actions as needed.
-
Relay Information Once emergency services arrive, please provide them with detailed information on your actions so far, including the duration of CPR and any AED interventions.
By following these detailed steps, you can provide critical assistance during an emergency, potentially saving a life.
Tools and Devices to Assist in Pulse Monitoring
Monitoring your pulse is essential for assessing cardiovascular health, identifying potential medical issues, and ensuring overall well-being. Today, various tools and devices are available to simplify pulse monitoring, providing both accurate results and real-time insights. These devices cater to many users, from healthcare professionals to fitness enthusiasts. Below, we explore two key categories of devices pivotal in pulse monitoring.
Using Pulse Oximeters and Heart Rate Monitors
Pulse Oximeters Pulse oximeters are small devices commonly used to measure the oxygen saturation levels in the blood, along with the pulse rate. They send light through the fingertip, toe, or earlobe and analyze how much light the blood absorbs. This painless and non-invasive method provides a quick and reliable way of identifying oxygenation issues. Pulse oximeters are widely used in hospitals, clinics, and even at home by individuals managing chronic illnesses like COPD or heart conditions. They are essential for tracking vital data during sleep studies, exercise, or emergencies.
Heart Rate Monitors Heart rate monitors are invaluable for tracking your pulse during physical activities or throughout the day. Most modern heart rate monitoring devices, like fitness trackers and smartwatches, use advanced sensors to provide continuous, real-time heart rate data. They help users to stay within target heart rate zones during workouts, thereby improving the effectiveness of their training sessions. Some models also provide advanced features such as stress level tracking and heart rate variability analysis, offering more profound insights into cardiovascular health. These tools are invaluable for athletes, as well as individuals managing chronic conditions like hypertension or arrhythmias.
Benefits of Automated External Defibrillators (AEDs) with Pulse Detection
Automated External Defibrillators (AEDs) are life-saving devices designed to restore normal heart rhythm in cases of sudden cardiac arrest. While traditional AEDs rely on analyzing heart rhythms to determine the need for a shock, models with integrated pulse detection offer heightened precision and efficiency.
These advanced AEDs assess the presence of a pulse before delivering a shock, reducing the risks of unnecessary electrical intervention. This capability minimizes potential harm and speeds up the decision-making process during emergencies. Furthermore, AEDs with pulse detection often come equipped with voice prompts and clear visual instructions, allowing even untrained bystanders to operate them effectively. This inclusivity maximizes their impact in saving lives, particularly in public spaces like airports, gyms, and schools.
Integrating automated pulse detection in AEDs enhances their utility across broader scenarios, ensuring better outcomes for individuals experiencing cardiac emergencies. These devices remain crucial to modern emergency response systems by bridging the gap between technology and user-friendliness.
Frequently Asked Questions
Q: What is CPR, and why is it important?
A: CPR, or cardiopulmonary resuscitation, is a life-saving technique used in emergencies when someone's heartbeat or breathing has stopped, such as in cases of cardiac arrest. It helps maintain blood flow and oxygenation to the brain and vital organs until professional medical help arrives.
Q: How do I check for a pulse during CPR?
A: To check for a pulse, locate the carotid artery on the side of the neck. Use your index and middle fingers to press gently against the artery for no more than 10 seconds. If you do not feel a pulse, you should begin CPR immediately.
Q: What is the correct way to perform hands-only CPR?
A: To perform hands-only CPR, place the heel of one hand on the center of the chest and the other on top. Push hard and fast at 100 to 120 compressions per minute, compressing to a depth of about 2 inches. Continue chest compressions until emergency medical help arrives or an automated external defibrillator (AED) is available.
Q: How can I determine if someone is in cardiac arrest?
A: You can check for responsiveness if someone is in cardiac arrest. Tap the person and shout to see if they respond. If there is no response and they are not breathing or only gasping, you should call 911 and begin CPR immediately.
Q: What should I do if I find a pulse during CPR?
A: If you detect a pulse during CPR, monitoring the person's breathing is crucial. If they are not breathing normally, you should continue chest compressions. If they are breathing, place them in recovery and wait for medical help.
Q: How long should I check for a pulse?
A: You should check for a pulse for no longer than 10 seconds. If you do not find a pulse within that time frame, you should start CPR immediately.
Q: Is mouth-to-mouth ventilation necessary in CPR?
A: In hands-only CPR, mouth-to-mouth ventilation is not necessary. You can provide effective chest compressions alone to maintain blood flow. However, if you are trained in CPR and feel comfortable, you can perform chest compressions and rescue breaths.
Q: When should I use an AED during CPR?
A: An AED, or automated external defibrillator, should be used as soon as it is available. After calling 911, you can apply the AED pads to the person's chest, follow the device's prompts, and continue CPR until the AED is ready to analyze the heart rhythm.
Q: How can I get CPR training?
A: CPR training is available through various organizations, including the Red Cross and the American Heart Association (AHA). You can find courses online or in person to become certified in CPR and learn the latest CPR guidelines and techniques.
The Bottom Line
Checking for a pulse before CPR is a critical step for trained responders, ensuring compressions are only used when truly needed. However, for untrained bystanders, the rule is simple: If someone is unresponsive and not breathing normally, start CPR immediately.
In emergencies, seconds count. Whether a medical professional or a concerned bystander, understanding when and how to check for a pulse can make the difference between life and death.





 Login with Google
Login with Google Login with Facebook
Login with Facebook