Almost no incidents are as electrifying as witnessing an infant's choking. For caregivers and onlookers. A comprehensive understanding of how to react when an infant’s choking could prove invaluable. This helps showcase the relevance of having this knowledge when it matters most. Knowing how to perform timely intervention can enhance your chances of pulling through a critical situation like this. Ensuring timely interventions, proper actions and anticipation goes a long way in ensuring responsible guardians manage to keep the infants fragile lives safe from getting into risky situations.
What Is Infant Choking?
Infant choking happens when an object blocks an infant's airway, preventing air from reaching the lungs. Since infants’ airways are small and developing, even minor obstructions can become life-threatening. This can occur due to various causes, such as food, small toys, or other items they explore with their mouths.
Common Causes of Infant Choking
- Food: Grapes, nuts, popcorn, hot dogs, and other foods large enough to block the airway.
- Small Objects: Coins, buttons, batteries, and toy parts are frequent hazards.
- Swelling or Illness: Allergies or infections that cause swelling in the airway.
Signs That an Infant Is Choking
Caregivers must know how to recognize choking immediately. Key signs include:
- Difficulty Breathing: Struggling to inhale or making wheezing sounds.
- Silent Crying or No Noise: Signals a complete airway blockage.
- Cyanosis: Bluish discoloration around the lips and face due to lack of oxygen.
- Coughing or Gagging: The body’s natural defense to clear a blockage.
- Distress or Panic: Wide eyes, frantic limb movements, or signs of panic.

How to Respond to a Choking Infant?
Responding effectively requires a calm, systematic approach. Follow these steps to dislodge the obstruction safely.
Step 1: Assess the Situation
Determine if the infant is indeed choking. If the baby is coughing or making sounds, they might be able to clear the obstruction on their own. However, stay close and monitor. If there’s no sound, crying, or breathing, act immediately.
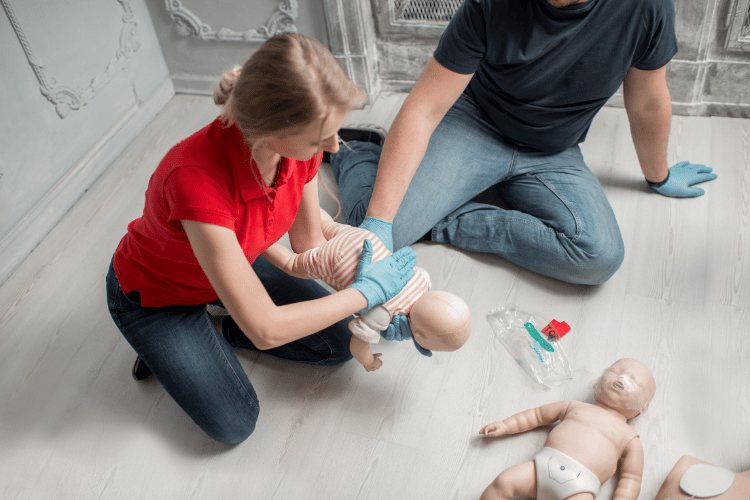
Step 2: Perform Back Blows
- Place the infant face-down along your forearm, ensuring its head is lower than its chest. Support the infant's head and neck with your hand.
- Sit or kneel, resting your arm on your thigh for stability.
- Using the heel of your free hand, deliver up to 5 firm back blows between the shoulder blades. Check after each blow to see if the object is dislodged.
Step 3: Perform Chest Thrusts
- If back blows don’t work, turn the infant face-up along your forearm, keeping their head lower than the chest.
- Use two fingers to press down in the center of the chest, just below the nipple line. Perform up to 5 quick chest thrusts, pressing about 1.5 inches deep and letting the chest rise between thrusts.
- Alternate between 5 back blows and five chest thrusts until the airway clears or the infant becomes unresponsive.
Step 4: When to Call for Help
- If the obstruction doesn’t clear quickly.
- If the infant loses consciousness or stops responding.
- If you cannot perform the back blows or chest thrusts effectively.
Call emergency services immediately while continuing the steps above. If the infant becomes unresponsive, begin CPR (described below) until help arrives.
What to Do If the Infant Becomes Unresponsive
- Check for Breathing: Place your ear near the infant’s mouth and nose while watching their chest. If there is no breathing, begin infant CPR immediately.
- Begin CPR:
- Position the infant on a flat, firm surface.
- Place two fingers on the center of the chest and administer 30 compressions at 100–120 compressions per minute, pressing about 1.5 inches deep.
- After compressions, give two gentle rescue breaths by covering their mouth and nose with your mouth, watching the chest rise.
- Repeat the cycle until help arrives or the infant recovers.
Preventing Infant Choking
While knowing what to do in an emergency is essential, prevention is always the best strategy. Follow these tips to minimize risk.
Mealtime Safety
- Supervise infants during meals.
- Avoid giving high-risk foods like whole grapes, nuts, popcorn, or hard candies.
- Cut foods into small, manageable pieces.
Toys and Objects
- Choose age-appropriate toys and ensure they don’t have small, detachable parts.
- Keep small items like buttons, batteries, and jewelry out of reach.
- Regularly inspect the environment to remove potential choking hazards.
General Precautions
- Always place the infant in an upright position during feeding.
- Learn infant first aid and CPR to prepare for emergencies.
- Be aware of developmental stages where choking is more likely, such as teething or exploratory phases.
Why Is Knowing Choking Response Important?
Acting quickly and correctly during a choking emergency can save a life. Delayed action or incorrect techniques can have severe consequences. By learning how to perform back blows, chest thrusts, and CPR, caregivers are empowered to act decisively and confidently.
This is essential knowledge for anyone who spends time with infants, including parents, babysitters, daycare staff, and relatives. It provides peace of mind and strengthens the safety net around your loved ones.
Frequently Asked Questions (FAQ)
Q1. What should I do if my infant is choking but coughing?
If your infant is coughing, it shows that some air is passing through the airway. Allow them to continue coughing, but stay vigilant. If the situation worsens, prepare to perform back blows and chest thrusts.
Q2. What should I do if my infant becomes unconscious while choking?
Place the infant on a flat surface and call emergency services immediately. Begin CPR by administering 30 chest compressions and 2 rescue breaths in each cycle. Continue until help arrives or the infant recovers.
Q3. Can I perform the Heimlich maneuver on an infant?
No, the Heimlich maneuver (abdominal thrusts) is not recommended for infants under one year, as it can cause internal injury. Use back blows and chest thrusts instead.
Q4. How can I prevent choking hazards in my home?
Keep small objects and dangerous foods out of reach. Inspect toys for detachable parts and supervise infants during play and meals.
Q5. Why is proper positioning important during back blows and chest thrusts?
Positioning the infant with its head lower than its chest allows gravity to dislodge the obstructing object effectively.
Conclusion
Choking is a frightening reality, but being prepared with the proper knowledge and skills can prevent tragedy. Recognizing the signs of choking, knowing how to perform back blows and chest thrusts, and taking preventive measures are all essential steps in ensuring an infant’s safety.
You can provide a safer environment and act confidently in emergencies by staying informed and diligent. Remember, preparation can save lives, and knowing the steps to respond makes all the difference.







 Login with Google
Login with Google Login with Facebook
Login with Facebook