
Hemostasis is the body’s natural process of stopping bleeding, a critical function that prevents excessive blood loss after injury. While the body has its clotting mechanisms, severe wounds—especially in trauma or surgical settings—often require external intervention. This is where hemostatic agents come into play. These specialized topical dressings accelerate clotting, control hemorrhage, and can mean the difference between life and death in emergencies.
While most people may not think about hemostatic dressings in their daily lives, medical professionals, military personnel, and first responders rely on them to manage bleeding effectively and efficiently. Understanding how these agents work, their different types, and their applications is essential for optimizing patient outcomes.
Let’s explore the mechanisms of hemostasis, the different classes of hemostatic agents, and how they are used in clinical and emergency settings.
Understanding Hemostasis
Hemostasis is a critical biological process that prevents excessive bleeding while maintaining normal blood flow within the body. This intricate mechanism is essential for survival, as it protects against significant blood loss after injury and preserves the fluidity of blood in uninjured vessels. Understanding hemostasis offers valuable insights into its phases and relevance, particularly in surgical contexts such as orthopedic procedures, where managing bleeding is crucial for achieving successful outcomes.

Understanding Hemostasis
The Process of Hemostasis
Hemostasis is a finely tuned process that involves multiple cellular and molecular events working together to achieve blood clotting and vessel repair. When a blood vessel is damaged, the body initiates a cascade of responses to halt blood flow at the injury site. This mechanism relies heavily on the interplay between vascular walls, platelets, and clotting factors. The delicate balance ensures a controlled response, preventing uncontrolled bleeding while minimizing the risk of unnecessary clot formation.
Phases of Hemostasis
There are three primary phases of hemostasis, each playing a distinct role:
- Vascular Spasm
This initial phase occurs immediately after vascular injury. The damaged vessel constricts to reduce blood flow, limiting the extent of blood loss.
- Platelet Plug Formation
Platelets adhere to exposed collagen at the injury site, forming a temporary plug. This process is enhanced by platelet activation, which releases chemicals that recruit additional platelets to strengthen the plug.
- Coagulation
The final phase involves the activation of clotting factors in a cascading sequence, resulting in the transformation of fibrinogen into fibrin. Fibrin strands weave through the platelet plug, solidifying it into a stable clot.
Importance in Orthopedic Surgery
Hemostasis is particularly significant in orthopedic surgery, where managing blood loss is crucial during procedures involving bones, joints, and connective tissues. Effective hemostatic control not only reduces surgical complications but also promotes improved post-operative outcomes. Surgeons often employ specialized tools and techniques, such as tourniquets, bone wax, and hemostatic agents, to manage bleeding efficiently, ensuring precision and patient safety throughout the surgery.
By exploring the intricate mechanisms of hemostasis, one gains a deeper appreciation of its role in preserving life and supporting medical advancements, especially in fields like orthopedics where it is indispensable.
Types of Hemostatic Agents
Hemostatic agents play a critical role in controlling bleeding during surgical procedures, trauma care, and emergencies. These agents are designed to accelerate the body's natural clotting process, ensuring rapid hemostasis and reducing the risk of complications associated with excessive blood loss. This overview delves into the various types of hemostatic agents, their mechanisms of action, and their specific applications in medical practice.

Hemostatic Agents
Overview of Hemostatic Agents
Hemostatic agents are broadly categorized into mechanical, active, and combination agents. Mechanical agents, such as sponges and gauzes, provide a physical barrier to bleeding, while active agents, like thrombin, directly enhance the clotting cascade. Combination agents integrate both mechanical and active properties for enhanced efficacy. These agents are widely used in surgeries, battlefield medicine, and emergency care, offering tailored solutions for different bleeding scenarios.
Microfibrillar Collagen as a Hemostat
Microfibrillar collagen is a widely used hemostatic agent derived from bovine collagen. It works by attracting platelets to the site of bleeding, promoting aggregation and clot formation. This agent is particularly effective in controlling diffuse bleeding from soft tissues and is commonly used in surgical settings. Its biocompatibility and ability to absorb into the body over time make it a preferred choice for many medical professionals.
Absorbable Dressings and Their Benefits
Absorbable dressings, such as oxidized regenerated cellulose and gelatin sponges, are designed to provide temporary hemostasis while being gradually absorbed by the body. These dressings are ideal for internal use, as they eliminate the need for removal and reduce the risk of infection. Their versatility and ease of application make them indispensable in both surgical and emergency care settings.
Application of Topical Dressings
Topical dressings are essential tools in managing bleeding, particularly in surgical, emergency, and trauma care settings. These dressings are designed to control hemorrhage, protect wounds, and promote healing. This section explores the application of topical dressings, focusing on their selection, techniques for effective use, and real-world examples of their success in clinical practice.
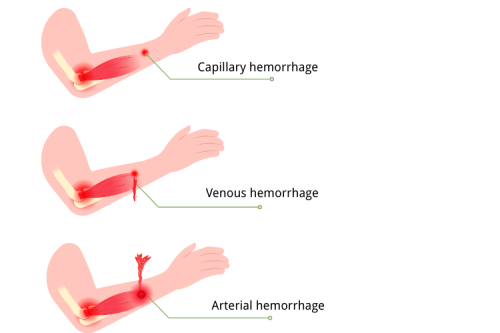
Choosing the Right Dressing for Bleeding
Selecting the appropriate topical dressing depends on the type and severity of bleeding, the location of the wound, and the patient's overall condition. Options include hemostatic dressings, absorbable materials, and pressure dressings, each tailored to specific needs. For instance, hemostatic dressings are ideal for arterial bleeding, while absorbable dressings are suited for internal wounds. Proper assessment ensures optimal outcomes and minimizes complications.
Techniques for Effective Application
The effectiveness of topical dressings relies heavily on proper application techniques. Key steps include cleaning the wound, applying direct pressure, and ensuring full contact between the dressing and the bleeding site. In surgical settings, securing the dressing with sutures or adhesives may be necessary. Adhering to these techniques enhances the dressing's ability to control bleeding and support tissue repair.
Case Studies: Successful Use of Topical Dressings
Numerous case studies highlight the efficacy of topical dressings in diverse scenarios. For example, in trauma care, hemostatic dressings have been shown to rapidly control severe bleeding, saving lives in critical situations. Similarly, absorbable dressings have demonstrated success in managing post-operative bleeding, reducing the need for additional interventions. These examples underscore the importance of topical dressings in modern medical practice.
Advanced Hemostatic Solutions
The field of hemostasis has evolved significantly, with advanced solutions now offering faster, more effective, and targeted bleeding control. These innovations address limitations of traditional methods, providing enhanced safety and efficiency in both surgical and emergency settings. This section examines the latest advancements in hemostatic agents, compares traditional and modern dressings, and explores future trends shaping the management of bleeding.
Innovations in Hemostatic Agents
Recent innovations in hemostatic agents have focused on bioengineered materials, nanotechnology, and synthetic compounds. Products like fibrin sealants, recombinant thrombin, and chitosan-based dressings have revolutionized bleeding control by mimicking or enhancing the body’s natural clotting mechanisms. These agents are designed for rapid action, biocompatibility, and minimal side effects, making them indispensable in critical care and complex surgical procedures.
Comparing Traditional vs. Modern Dressings
Traditional dressings, such as gauze and cotton pads, primarily rely on physical pressure to control bleeding. While effective in minor cases, they often fall short in managing severe or arterial hemorrhages. Modern dressings, on the other hand, incorporate hemostatic agents, advanced polymers, and absorbable materials. These innovations not only stop bleeding more efficiently but also reduce infection risks and promote faster healing, offering a significant advantage over conventional methods.
Future Trends in Hemostasis Management
The future of hemostasis management lies in personalized medicine, smart dressings, and regenerative technologies. Smart dressings equipped with sensors to monitor bleeding and wound healing are under development, promising real-time feedback and improved outcomes. Additionally, research into regenerative materials aims to create dressings that not only stop bleeding but also actively repair damaged tissues. These advancements are set to redefine bleeding management in the years to come.
Transfusion and Hemostasis
Transfusion plays a pivotal role in managing significant blood loss and restoring hemostasis in critical medical situations. While transfusions are often necessary to replenish blood volume and clotting factors, they are frequently complemented by hemostatic agents to optimize bleeding control. This section explores the circumstances requiring transfusion, the integration of hemostatic agents in transfusion scenarios, and the associated risks and benefits.
When is Transfusion Necessary?
Transfusions are typically required in cases of severe blood loss due to trauma, surgery, or medical conditions like anemia or coagulopathies. They are essential when the patient’s hemoglobin levels drop critically or when clotting factors are depleted, impairing the body’s ability to achieve hemostasis. The decision to transfuse is guided by clinical assessments, including blood tests, vital signs, and the extent of bleeding.
Role of Hemostatic Agents in Transfusion Scenarios
Hemostatic agents are often used alongside transfusions to enhance clot formation and stabilize bleeding. For instance, fibrin sealants, thrombin-based products, and absorbable dressings can be applied locally to control hemorrhage while transfusions restore systemic blood volume and clotting components. This combination approach is particularly effective in surgical and trauma settings, where rapid and comprehensive bleeding control is critical.
Risks and Benefits of Transfusion in Hemostasis
While transfusions are life-saving, they carry potential risks, including allergic reactions, infections, and iron overload. Additionally, improper use can lead to complications like transfusion-related acute lung injury (TRALI). However, the benefits often outweigh the risks, as transfusions restore oxygen delivery, improve clotting, and prevent shock. When combined with hemostatic agents, transfusions provide a robust strategy for managing complex bleeding scenarios.
Frequently Asked Questions
What are hemostatic agents?
Hemostatic agents are substances used to promote hemostasis, which is the process of stopping bleeding. They can be classified into various categories, such as topical hemostatic agents, biological hemostatic agents, and mechanical hemostatic agents. These agents are commonly used in surgical settings to control blood loss and ensure effective coagulation at the bleeding site.
How do topical hemostatic agents work?
Topical hemostatic agents work by facilitating the clot formation process at the site of bleeding. They promote the aggregation of platelets and enhance the coagulation cascade, leading to the formation of a fibrin clot. Common examples include oxidized cellulose, absorbable gelatin sponge, and topical thrombin, which can be applied directly to the surgical site to help control bleeding.
What is the role of fibrin in hemostasis?
Fibrin plays a crucial role in hemostasis as it forms the structural framework of a blood clot. During the clotting process, fibrinogen is converted into fibrin by thrombin. This fibrin meshwork helps stabilize the platelet plug formed during primary hemostasis, thus preventing further blood loss and promoting wound healing.
What are the different types of hemostatic dressings?
Hemostatic dressings come in various forms, such as gauze impregnated with hemostatic agents, gelatin sponges, and oxidized regenerated cellulose. These dressings are designed to control bleeding by providing a physical barrier, promoting platelet aggregation, and accelerating the clotting process. They are widely used in surgical procedures and emergency settings.
How does a gelatin sponge aid in hemorrhage control?
A gelatin sponge aids in hemorrhage control by serving as a scaffold for clot formation. When applied to a bleeding site, it absorbs blood and provides a surface for platelets to adhere and aggregate. This action enhances the coagulation cascade, leading to the formation of a stable fibrin clot that helps stop bleeding effectively.
What is the coagulation cascade?
The coagulation cascade is a series of biochemical reactions involving clotting factors that lead to the formation of a fibrin clot. It consists of two pathways: the intrinsic and extrinsic pathways, which converge at a common pathway to produce thrombin. This cascade is essential for normal hemostasis and is activated in response to blood vessel injury.
What is the difference between primary and secondary hemostasis?
Primary hemostasis involves the formation of a platelet plug at the site of injury, while secondary hemostasis refers to the stabilization of this plug through the formation of a fibrin clot. Primary hemostasis occurs rapidly, but secondary hemostasis is crucial for ensuring long-term control of bleeding and involves the activation of the coagulation cascade.
Which conditions can lead to thrombosis?
Thrombosis can occur when there is an abnormal increase in blood clot formation, which can be influenced by factors such as vascular damage, stasis of blood flow, and hypercoagulability. Conditions like surgery, prolonged immobility, and certain medical conditions can increase the risk of thrombosis, leading to complications such as deep vein thrombosis (DVT) or pulmonary embolism.
How can human fibrinogen be used in hemostatic applications?
Human fibrinogen can be used in hemostatic applications as a biologic agent to promote clot formation. When combined with thrombin, it forms a fibrin sealant that can be applied to surgical sites to enhance hemostasis. This combination effectively augments the coagulation cascade and provides a strong, adhesive clot that helps control bleeding during surgical procedures.
The Bottom Line
Hemostatic agents are a lifesaving innovation in bleeding control, offering tailored solutions for everything from minor cuts to catastrophic hemorrhage. Whether in a hospital, battlefield, or everyday emergency kit, the right hemostatic dressing can drastically improve survival rates.
Choosing the appropriate agent depends on the type of bleeding, patient condition, and setting—whether it's a kaolin-impregnated gauze for traumatic wounds or a fibrin sealant for surgical precision. As research advances, next-generation hemostatics promise even faster clotting with fewer side effects, further revolutionizing bleeding management.
For medical professionals and emergency responders, staying updated on these technologies ensures the best possible outcomes when seconds count.





 Login with Google
Login with Google Login with Facebook
Login with Facebook