Airway management is a critical skill in emergency medicine, anesthesia, and critical care. When a patient's ability to maintain an open airway is compromised, healthcare providers often turn to simple yet effective adjuncts like oropharyngeal (OPA) and nasopharyngeal (NPA) airways. These devices help prevent airway obstruction, ensuring adequate oxygenation and ventilation until more definitive measures can be taken.
While the average person may never encounter these tools outside of a medical setting, their proper use can mean the difference between life and death in emergency scenarios. Understanding the differences, indications, and insertion techniques of these devices is essential for medical professionals.
Let's explore the key differences between OPAs and NPAs, when to use each, and the step-by-step process for safe and effective insertion.
Understanding Airway Management
Airway management is a critical component of emergency care, ensuring that oxygen can flow freely into the lungs to sustain life. Maintaining airway patency is often the first step in responding to respiratory distress or cardiac arrest, and it requires both foundational knowledge and practical skills. This overview highlights the significance of airway patency, introduces airway devices, and compares the differences between oropharyngeal and nasopharyngeal airways.
Understanding Airway Management
The Importance of Airway Patency
Airway patency refers to the openness of the airway, which is essential for effective breathing and oxygenation. Key reasons for maintaining airway patency include:
- Preventing Hypoxia: Blocked airways can lead to oxygen deprivation, causing organ failure or brain damage within minutes.
- Supporting Ventilation: Ensuring a clear airway allows for effective rescue breaths during CPR or mechanical ventilation.
- Managing Emergencies: Conditions such as choking, trauma, or unconsciousness often require immediate airway intervention to prevent further complications. Proper airway management is vital for stabilizing patients and improving outcomes in critical situations.
Overview of Airway Devices
Airway devices are tools used to maintain or restore airway patency. Common devices include:
- Bag-Valve-Mask (BVM): Used to deliver ventilation manually in patients who are not breathing adequately.
- Suction Devices: Remove obstructions such as mucus, blood, or vomit from the airway.
- Advanced Airways: Devices like endotracheal tubes or supraglottic airways are used in advanced life support settings to secure the airway. These tools are essential for both basic and advanced airway management, depending on the severity of the situation.
Types of Airways: Oropharyngeal vs. Nasopharyngeal
Two commonly used airway adjuncts are:
- Oropharyngeal Airways (OPA): Inserted into the mouth to prevent the tongue from obstructing the airway. OPAs are suitable for unconscious patients without a gag reflex.
- Nasopharyngeal Airways (NPA): Inserted through the nose to maintain airway patency. NPAs are ideal for semi-conscious patients or those with an intact gag reflex. Both devices play a crucial role in emergency care, and selecting the appropriate type depends on the patient's condition and level of consciousness.
By understanding airway management techniques and tools, responders can effectively address respiratory emergencies and improve patient survival rates.
Oropharyngeal Airways
Oropharyngeal airways (OPAs) are essential tools in airway management, designed to maintain patency by preventing the tongue from obstructing the airway. They are commonly used in emergency and clinical settings to support ventilation in patients who are unconscious or unable to maintain their airway. This guide explores the indications for using OPAs, outlines proper insertion techniques, and highlights potential complications and considerations.

Oropharyngeal Airways
Indications for Use
OPAs are indicated in specific scenarios where airway obstruction is a concern. Key indications include:
- Unconscious Patients: OPAs are suitable for patients who are unresponsive and lack a gag reflex, as this minimizes the risk of triggering vomiting or aspiration.
- Airway Obstruction: Used to prevent the tongue from collapsing backward and blocking the airway, particularly in cases of respiratory arrest or deep sedation.
- Facilitating Ventilation: OPAs provide a clear pathway for manual ventilation using a bag-valve-mask (BVM) or other devices. They are not recommended for conscious or semi-conscious patients due to the risk of gagging or laryngospasm.
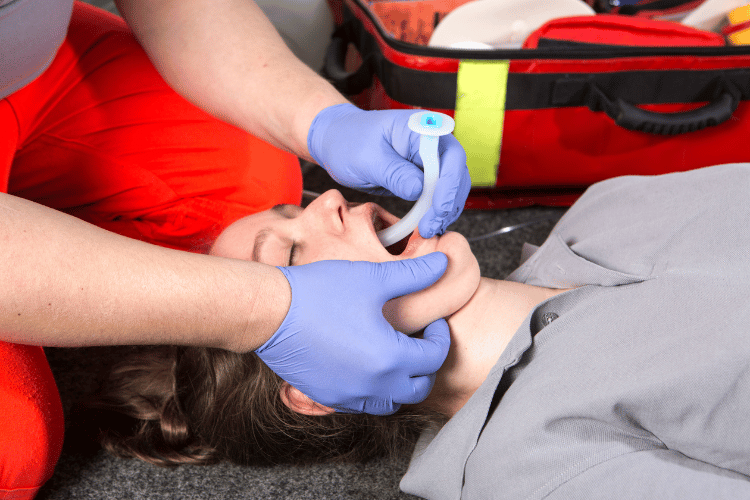
Insertion Techniques
Proper insertion of an OPA is critical to ensure effectiveness and patient safety. Steps include:
- Select the Correct Size: Measure from the corner of the patient's mouth to the angle of the jaw to determine the appropriate size.
- Position the Patient: Place the patient in a supine position with the head tilted back to maintain an open airway.
- Insert the OPA: Insert the airway upside down (concave side up) and rotate it 180 degrees as it advances into the oropharynx. This technique prevents the tongue from being pushed further back.
- Secure the Device: Ensure the flange rests against the patient's lips or teeth to keep the airway in place.
Complications and Considerations
While OPAs are effective, they can present certain risks and require careful consideration:
- Gag Reflex Stimulation: Inserting an OPA in a patient with an intact gag reflex can cause vomiting or aspiration.
- Oral Trauma: Improper insertion may lead to injuries such as lacerations or dental damage.
- Airway Obstruction: Using an incorrect size or improper placement can worsen airway obstruction. Clinicians must assess the patient's condition and monitor for complications during and after insertion.
By understanding the indications, techniques, and potential risks associated with OPAs, healthcare providers can use this device effectively to manage airways and improve patient outcomes.
Nasopharyngeal Airways
Nasopharyngeal airways (NPAs) are versatile tools in airway management, designed to maintain patency by providing a clear passage through the nasal cavity to the pharynx. They are particularly useful in situations where oropharyngeal airways are not suitable, offering an alternative for semi-conscious patients or those with an intact gag reflex. This guide explores the indications for using NPAs, outlines proper insertion techniques, and highlights potential complications and considerations.
Indications for Use
NPAs are indicated in various scenarios where maintaining airway patency is critical. Key indications include:
- Semi-Conscious Patients: NPAs are ideal for patients who are not fully unconscious but require airway support, as they do not stimulate the gag reflex.
- Facial or Oral Trauma: When oral access is restricted due to injuries or obstructions, NPA provides a reliable alternative.
- Prolonged Airway Management: NPAs are often used for patients requiring repeated suctioning or extended airway support. They are not recommended for patients with suspected skull fractures or severe nasal trauma due to the risk of further injury.
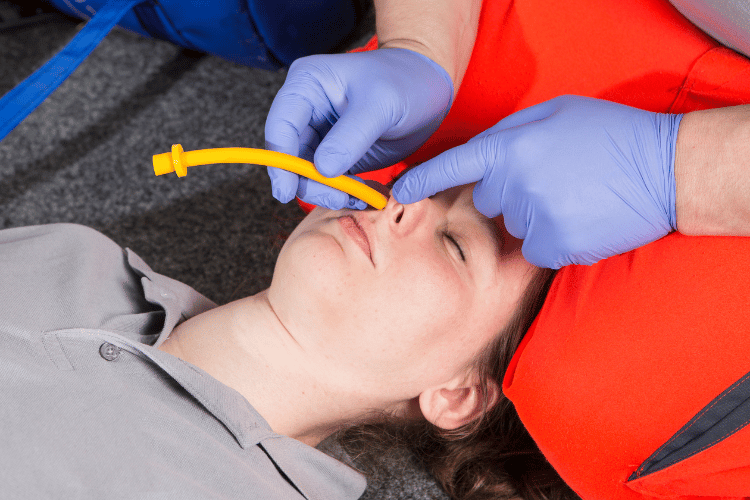
Insertion Techniques
Proper insertion of an NPA is essential to ensure effectiveness and minimize discomfort. Steps include:
- Select the Correct Size: Measure from the tip of the patient's nose to the earlobe to determine the appropriate length.
- Lubricate the Airway: Apply a water-soluble lubricant to reduce friction and ease insertion.
- Insert the NPA: Gently insert the airway into the nostril, following the natural curvature of the nasal passage. Avoid forcing the device if resistance is encountered.
- Secure the Device: Ensure the flange rests against the nostril to prevent the airway from slipping further into the nasal cavity.
Complications and Considerations
While NPAs are effective, they can present certain risks and require careful consideration:
- Nasal Trauma: Improper insertion may cause bleeding or damage to the nasal mucosa.
- Airway Obstruction: Using an incorrect size or improper placement can lead to partial or complete obstruction.
- Infection Risk: Prolonged use of NPAs may increase the risk of infection if not monitored and replaced as needed. Clinicians must assess the patient's condition and monitor for complications during and after insertion to ensure safe and effective use.
By understanding the indications, techniques, and potential risks associated with NPAs, healthcare providers can confidently use this device to manage airways and improve patient outcomes.
Comparing Oropharyngeal and Nasopharyngeal Airways
Oropharyngeal (OPA) and nasopharyngeal (NPA) airways are two commonly used devices in airway management, each designed to maintain patency and support ventilation in different clinical scenarios. While both serve the same overarching purpose, their applications, advantages, and limitations vary significantly. This guide compares the two devices, highlighting their advantages and disadvantages, situational use cases, and how they can be combined for effective airway management.
Advantages and Disadvantages
Each device offers unique benefits and potential drawbacks depending on the patient's condition and the clinical setting:
- Oropharyngeal Airways (OPA):
-
- Advantages: Easy to insert, effective in preventing tongue obstruction, and ideal for unconscious patients without a gag reflex.
- Disadvantages: Cannot be used in conscious or semi-conscious patients due to gag reflex stimulation and risk of aspiration.
- Nasopharyngeal Airways (NPA):
-
- Advantages: Suitable for semi-conscious patients, does not trigger the gag reflex, and can be used in cases of oral trauma or restricted mouth access.
- Disadvantages: Risk of nasal trauma, bleeding, and contraindicated in patients with suspected skull fractures or severe nasal injuries.
Situational Use Cases
The choice between OPA and NPA depends on the specific clinical scenario:
- OPA Use Cases: Ideal for unconscious patients during CPR, anesthesia, or deep sedation where the gag reflex is absent.
- NPA Use Cases: Preferred for semi-conscious patients, those with oral injuries, or when repeated suctioning is required. Understanding the patient's condition and contraindications is critical for selecting the appropriate device.
Combined Use in Airway Management
In some cases, OPAs and NPAs can be used together to optimize airway management:
- Sequential Use: An NPA may be used initially in semi-conscious patients, transitioning to an OPA once the patient becomes fully unconscious.
- Dual Airway Support: Both devices can be employed simultaneously in complex cases to ensure airway patency and facilitate ventilation. By leveraging the strengths of both devices, healthcare providers can address a wider range of airway challenges and improve patient outcomes.
Endotracheal Intubation and Its Relation to Airways
Endotracheal intubation is a critical procedure in advanced airway management, providing a secure and reliable method to maintain airway patency and facilitate ventilation. It is often employed in emergency, surgical, and critical care settings when basic airway adjuncts, such as oropharyngeal or nasopharyngeal airways, are insufficient. This guide explores when to consider endotracheal intubation, outlines key intubation techniques, and examines the role of supraglottic airway devices as complementary tools.
When to Consider Endotracheal Intubation
Endotracheal intubation is indicated in situations where airway protection or mechanical ventilation is required. Common scenarios include:
- Respiratory Failure: Patients unable to maintain adequate oxygenation or ventilation on their own.
- Airway Obstruction: Severe obstructions caused by trauma, swelling, or foreign bodies.
- Anesthesia: Ensuring airway control during surgical procedures requiring general anesthesia.
- Cardiac Arrest: Providing a secure airway for effective ventilation during resuscitation efforts. This procedure is typically reserved for cases where less invasive methods are inadequate or contraindicated.
Intubation Techniques
Successful intubation requires precision and adherence to proper techniques. Key steps include:
- Preparation: Assemble necessary equipment, including an endotracheal tube, laryngoscope, and suction device.
- Positioning: Place the patient in the "sniffing" position to align the airway for optimal visualization.
- Laryngoscopy: Use a laryngoscope to visualize the vocal cords and guide the tube into the trachea.
- Tube Placement: Insert the endotracheal tube through the vocal cords and confirm placement using capnography or auscultation.
- Securing the Tube: Secure the tube to prevent displacement and ensure continuous ventilation.
Role of Supraglottic Airway Devices
Supraglottic airway devices (SGAs) serve as valuable alternatives or adjuncts to endotracheal intubation:
- Bridge to Intubation: SGAs can provide temporary airway support while preparing for intubation.
- Difficult Airway Management: In cases where intubation is challenging, SGAs offer a less invasive option to maintain ventilation.
- Emergency Use: Quick to deploy, SGAs are ideal for pre-hospital or emergency settings when time is critical. By understanding the relationship between endotracheal intubation and other airway devices, healthcare providers can make informed decisions to optimize patient care in complex airway scenarios.
Frequently Asked Questions
What is an oropharyngeal airway (OPA)?
An oropharyngeal airway, commonly referred to as an OPA, is a medical device designed to maintain an open airway in patients who are unable to do so themselves. It is inserted into the oropharynx, allowing for adequate ventilation and preventing airway obstruction caused by the tongue or soft tissue in the throat.
How do you insert an oropharyngeal airway?
The oral airway is inserted by gently depressing the tongue and placing the OPA along the roof of the mouth, following the curvature of the posterior pharynx. It is important to ensure that the tip of the airway is directed towards the posterior wall of the pharynx while rotating the device 180 degrees to ensure proper placement.
What are the indications for using an OPA?
OPAs are often used in emergency situations to relieve upper airway obstruction, particularly in unconscious patients who lack a gag reflex. They are also indicated for patients undergoing anesthesia or those requiring mechanical ventilation to maintain a patent airway.
How do you determine the correct size of an OPA?
To select the appropriate size, measure the distance from the patient's incisors to the angle of the mandible. An appropriately sized airway will fit comfortably without obstructing the airway. If the airway is too small, it may not keep the airway open, while an airway that is too large may obstruct the airway instead.
What are the potential complications of using an OPA?
Complications may include gagging, vomiting, or trauma to the oral cavity or pharynx. If the device is not inserted correctly, it can obstruct the airway instead of relieving it. Additionally, improper sizing can lead to inadequate ventilation or airway obstruction due to the device itself.
What is the difference between an oropharyngeal airway and an endotracheal tube?
While both devices serve to maintain an open airway, an oropharyngeal airway is designed for use in unconscious patients and does not provide a secure airway. In contrast, an endotracheal tube is inserted into the trachea for more secure airway management and is often used during surgical procedures involving general anesthesia.
How can an OPA help prevent airway obstruction?
An OPA helps prevent obstruction of the airway by keeping the tongue from falling back into the pharynx, which can obstruct airflow. By maintaining an open airway, the OPA allows for adequate ventilation and oxygenation, especially in patients with a compromised airway.
What is the Guedel pattern airway?
The Guedel pattern airway, also known as the Guedel airway, is a specific design of oropharyngeal airway that has a flange to prevent the device from being inserted too deeply. This design helps ensure the airway remains patent while minimizing the risk of trauma to the pharyngeal wall.
Can an OPA be used in conscious patients?
Generally, OPAs are not recommended for conscious patients as they may provoke the gag reflex and cause discomfort. In conscious patients, other airway adjuncts, such as a nasopharyngeal airway, may be more appropriate to maintain an open airway without causing obstruction.
The Bottom Line
Both oropharyngeal and nasopharyngeal airways are indispensable tools in airway management, each with specific indications and techniques. OPAs are best for unconscious patients without a gag reflex, while NPAs offer a less invasive option for those who are semi-conscious or have oral obstructions.
Mastering their insertion ensures prompt and effective airway support, preventing hypoxia and improving patient outcomes. Whether in an emergency department, ICU, or pre-hospital setting, these simple devices play a vital role in keeping patients breathing—until more advanced interventions can be applied.
Choose the right airway adjunct, apply proper technique, and you'll be well-equipped to handle critical airway challenges with confidence.















 Login with Google
Login with Google Login with Facebook
Login with Facebook