Ventricular fibrillation (V-fib) is a life-threatening cardiac arrhythmia that can lead to sudden cardiac arrest if not treated immediately. While most people may never think about the intricate electrical signals that keep their heart beating, disruptions in this system—like V-fib—can have devastating consequences.
Medical professionals and emergency responders recognize ventricular fibrillation as one of the most critical heart rhythm disorders, requiring rapid intervention to prevent death. Understanding its causes, recognizing its symptoms, and knowing the available treatments can mean the difference between life and death.
Let’s take a closer look at ventricular fibrillation, how it disrupts normal heart function, and the medical interventions that can restore a stable rhythm.
Understanding Ventricular Fibrillation
Ventricular fibrillation (VF) is a life-threatening cardiac arrhythmia characterized by rapid, erratic electrical impulses in the ventricles, leading to ineffective heart contractions and a cessation of blood circulation. As a major cause of sudden cardiac arrest, VF requires immediate medical intervention to prevent fatal outcomes. This guide explores the nature of ventricular fibrillation, explains its occurrence, and examines the types of arrhythmias associated with ventricular fibrillation.
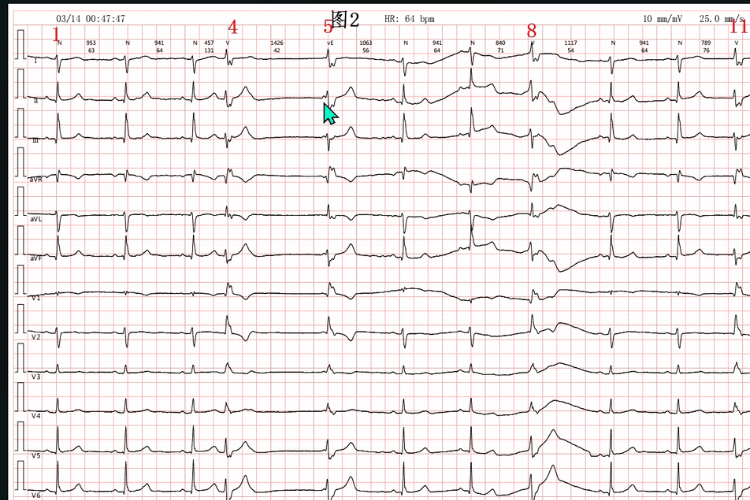
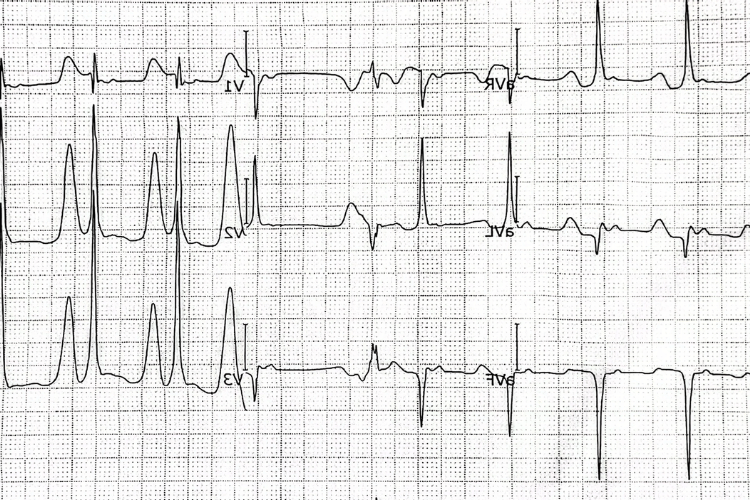
Ventricular parallel rhythm, sinus-ventricular fusion wave
What is Ventricular Fibrillation?
Ventricular fibrillation is a severe disruption of the heart’s electrical activity, causing the ventricles to quiver instead of contracting effectively. Key characteristics include:
- Loss of Cardiac Output: The heart cannot pump blood, leading to a lack of oxygen delivery to vital organs.
- Medical Emergency: VF is a primary cause of sudden cardiac death and requires immediate defibrillation to restore normal rhythm.
- Underlying Causes: Conditions such as coronary artery disease, myocardial infarction, or electrolyte imbalances often trigger VF.
How Ventricular Fibrillation Occurs
VF results from abnormalities in the heart’s electrical conduction system. The process typically involves:
- Electrical Instability: Damage to the heart muscle, such as from a heart attack, creates areas of electrical instability.
- Re-Entry Circuits: Disrupted electrical signals form circular pathways, leading to chaotic impulses.
- Rapid Ventricular Activity: The ventricles lose their coordinated contraction, resulting in ineffective blood pumping. These mechanisms underscore the urgent need for prompt diagnosis and treatment to prevent irreversible damage.
Types of Arrhythmias Associated with VF
Ventricular fibrillation is often linked to other arrhythmias, including:
- Ventricular Tachycardia (VT): A fast but organized rhythm that can deteriorate into VF if untreated.
- Premature Ventricular Contractions (PVCs): Extra heartbeats originating in the ventricles, which may precede VF in susceptible individuals.
- Torsades de Pointes: A specific type of polymorphic VT associated with prolonged QT intervals, which can escalate to VF. Understanding these arrhythmias is essential for identifying patients at risk and implementing preventive measures. By recognizing the mechanisms and associated conditions of VF, healthcare providers can improve outcomes and reduce the risk of sudden cardiac death.
Causes of Ventricular Fibrillation
Ventricular fibrillation (VF) is a critical cardiac arrhythmia that disrupts the heart’s ability to pump blood effectively, often leading to sudden cardiac arrest. Understanding the causes of VF involves examining the underlying heart conditions, identifying key risk factors, and recognizing external triggers that can precipitate this life-threatening event. This guide provides a detailed overview of these contributing factors to help in prevention and management.

Causes of Ventricular Fibrillation
Underlying Heart Conditions
Several heart conditions increase the likelihood of developing ventricular fibrillation. These include:
- Coronary Artery Disease (CAD): Blockages in the coronary arteries reduce blood flow to the heart muscle, leading to ischemia and increasing the risk of VF.
- Myocardial Infarction (Heart Attack): Damage to the heart muscle from a heart attack can create electrical instability, a common precursor to VF.
- Cardiomyopathy: Conditions that weaken or enlarge the heart muscle, such as dilated or hypertrophic cardiomyopathy, can disrupt normal electrical conduction.
- Congenital Heart Defects: Structural abnormalities present at birth may predispose individuals to arrhythmias, including VF.
Risk Factors for Ventricular Fibrillation
Certain factors elevate the risk of VF, including:
- Previous Cardiac Events: A history of heart attacks or arrhythmias significantly increases the likelihood of VF.
- Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium can interfere with the heart’s electrical activity.
- Genetic Predisposition: Inherited conditions, such as long QT syndrome or Brugada syndrome, are associated with a higher risk of VF.
- Age and Gender: VF is more common in older adults and men, particularly those with pre-existing heart conditions.
External Triggers of VF
In addition to internal factors, external triggers can provoke ventricular fibrillation. These include:
- Electrical Shock: Exposure to high-voltage electricity can disrupt the heart’s rhythm and induce VF.
- Drug Use: Stimulants like cocaine or amphetamines can overstimulate the heart and lead to arrhythmias.
- Severe Trauma: Blunt chest injuries, such as those sustained in accidents, may cause commotio cordis, a rare but fatal trigger of VF. By understanding the causes, risk factors, and triggers of ventricular fibrillation, healthcare providers can better identify at-risk individuals and implement strategies to prevent this life-threatening condition.
Signs and Symptoms of Ventricular Fibrillation
Ventricular fibrillation (VF) is a life-threatening condition that requires immediate medical attention. It disrupts the heart’s ability to pump blood, leading to sudden cardiac arrest if untreated. Recognizing the signs and symptoms of ventricular fibrillation (VF) is crucial for prompt intervention. This guide explores how to identify symptoms of cardiac arrest, highlights common signs of VF, and emphasizes when to seek emergency help.
Signs and Symptoms of Ventricular Fibrillation
Identifying Symptoms of Cardiac Arrest
Ventricular fibrillation often leads to cardiac arrest, a medical emergency where the heart stops pumping blood effectively. Key symptoms include:
- Sudden Loss of Consciousness: The brain is deprived of oxygen, causing the individual to collapse and become unresponsive.
- No Pulse: The erratic electrical activity in VF prevents the heart from producing a detectable pulse.
- Cessation of Breathing: Breathing may stop entirely or become gasping and irregular (agonal respirations). These symptoms occur rapidly, often without warning, underscoring the need for immediate action.
Common Signs of VF
While VF progresses quickly to cardiac arrest, there may be warning signs in some cases. These include:
- Chest Pain or Discomfort: A sensation of pressure or tightness in the chest may precede VF, especially in individuals with underlying heart conditions.
- Dizziness or Lightheadedness: Reduced blood flow to the brain can cause faintness or a feeling of impending collapse.
- Palpitations: A sensation of rapid or irregular heartbeats may occur as the heart’s rhythm becomes unstable.
- Shortness of Breath: Difficulty breathing may signal reduced oxygen delivery to the body. These signs may appear moments before VF or during its onset, providing a brief window for intervention.
When to Seek Emergency Help
Ventricular fibrillation is a medical emergency that requires immediate treatment. Seek help if:
- Sudden Collapse Occurs: Call emergency services immediately if someone collapses and is unresponsive.
- Warning Signs Appear: Symptoms like chest pain, severe dizziness, or palpitations should prompt urgent medical evaluation.
- Use of an AED: If available, an automated external defibrillator (AED) should be used as soon as possible to restore normal heart rhythm. Recognizing the signs and symptoms of VF and acting quickly can save lives, making awareness and preparedness essential in managing this critical condition.
Treatment Options for Ventricular Fibrillation
Ventricular fibrillation (VF) is a medical emergency that requires immediate intervention to restore normal heart rhythm and prevent fatal outcomes. Beyond emergency care, long-term management and preventive measures are essential to reduce the risk of recurrence. This guide outlines the immediate steps for treating cardiac arrest caused by VF, explores strategies for long-term management, and highlights preventive measures to minimize future risk.
Immediate Care for Cardiac Arrest
The primary goal in treating VF during cardiac arrest is to restore effective circulation as quickly as possible. Key interventions include:
- Defibrillation: The use of an automated external defibrillator (AED) or manual defibrillator delivers an electric shock to reset the heart’s rhythm. This is the most effective treatment for VF.
- Cardiopulmonary Resuscitation (CPR): High-quality chest compressions maintain blood flow to vital organs until defibrillation can be performed.
- Advanced Life Support (ALS): In a hospital or advanced care setting, medications such as epinephrine and antiarrhythmic drugs (e.g., amiodarone) may be administered to stabilize the heart. Immediate action is critical, as survival rates decrease significantly with every minute of delay.
Long-term Management Strategies
After surviving an episode of VF, patients require ongoing care to prevent recurrence. Long-term strategies include:
- Implantable Cardioverter-Defibrillator (ICD): An ICD monitors heart rhythm and delivers shocks if VF or other dangerous arrhythmias occur.
- Medications: Antiarrhythmic drugs help regulate heart rhythm and reduce the likelihood of future episodes.
- Lifestyle Modifications: Managing underlying conditions, such as coronary artery disease or hypertension, through diet, exercise, and medication is essential for long-term health. These strategies aim to reduce the risk of future VF episodes and improve overall cardiac stability.
Preventive Measures to Reduce Risk
Preventing VF involves addressing risk factors and maintaining heart health. Key measures include:
- Regular Medical Checkups: Routine monitoring can identify and manage conditions that increase VF risk, such as arrhythmias or electrolyte imbalances.
- Heart-Healthy Lifestyle: A balanced diet, regular exercise, and avoiding smoking or excessive alcohol consumption support cardiovascular health.
- Managing Chronic Conditions: Controlling diabetes, high blood pressure, and cholesterol levels reduces strain on the heart. By combining immediate care, long-term management, and preventive strategies, healthcare providers can improve outcomes and reduce the risk of ventricular fibrillation recurrence.
Frequently Asked Questions
What is ventricular fibrillation?
Ventricular fibrillation (V-fib or VF) is a type of abnormal heart rhythm that occurs when the electrical activity in the ventricles becomes chaotic, causing the heart to quiver instead of pump blood effectively. This can lead to sudden cardiac arrest if not treated immediately.
What are the causes of ventricular fibrillation?
Various factors, including coronary artery disease, heart failure, or a previous heart attack can trigger ventricular fibrillation. Other causes may include long QT syndrome, idiopathic ventricular fibrillation, and other forms of ventricular arrhythmia.
How is ventricular fibrillation diagnosed?
Ventricular fibrillation is typically diagnosed using an electrocardiogram (ECG), which records the heart's electrical activity. During an episode of ventricular fibrillation, the ECG will show a rapid and irregular heartbeat, indicating a lack of effective pumping action.
What is the treatment for ventricular fibrillation?
The immediate treatment for ventricular fibrillation is defibrillation, which involves delivering an electric shock to the heart using a defibrillator. This can restore a normal heart rhythm. Cardiopulmonary resuscitation (CPR) should also be administered until emergency medical services arrive.
What is the role of an automated external defibrillator (AED)?
An automated external defibrillator (AED) is a portable device that analyzes the heart's rhythm and delivers an electric shock if necessary. It is designed for use by laypersons and can be crucial in out-of-hospital cardiac arrest situations to treat ventricular fibrillation effectively.
What are the symptoms of ventricular fibrillation?
Symptoms of ventricular fibrillation may include sudden loss of consciousness, absence of pulse, and breathing difficulties. It is essential to recognize these symptoms promptly, as they indicate a medical emergency that requires immediate attention.
How does ventricular fibrillation relate to sudden cardiac death?
Ventricular fibrillation is a leading cause of sudden cardiac death. When the heart experiences this dangerous arrhythmia, it cannot pump blood effectively, leading to a rapid decline in blood flow to vital organs, which can be fatal without immediate intervention.
Can ventricular fibrillation be prevented?
While not all cases of ventricular fibrillation can be prevented, certain risk factors can be managed. Maintaining a healthy lifestyle, monitoring heart health, and following the American Heart Association guidelines can help reduce the risk for ventricular arrhythmias and subsequent episodes of ventricular fibrillation.
What should I do if I witness someone experiencing ventricular fibrillation?
If you witness someone collapse and suspect they are experiencing ventricular fibrillation, call 911 immediately and begin CPR. If an AED is available, use it as soon as possible to deliver a shock to the heart, which can help restore a normal rhythm.
The Bottom Line
Ventricular fibrillation is a medical emergency that demands immediate action. Without prompt CPR and defibrillation, survival rates drop drastically within minutes.
For those at risk—such as individuals with a history of heart disease or genetic arrhythmias—preventive measures like ICD implantation and regular cardiac monitoring are essential.
Understanding the causes, recognizing the signs, and knowing the life-saving steps can empower bystanders and medical professionals alike to act swiftly, turning a deadly arrhythmia into a survivable event.
If you or someone you know has risk factors for V-fib, consult a cardiologist to explore preventive strategies and emergency preparedness. Every second counts when the heart’s rhythm is on the line.















 Login with Google
Login with Google Login with Facebook
Login with Facebook