
When babies younger than one year old start to choke, every second is essential. For this reason, knowing how to respond in such situations appropriately can be a lifesaver. The following guide contains a comprehensive step-by-step approach to dealing with infant choking situations, including how to spot the signs of a child who is choking, how to evaluate the problem, and how to perform first aid to aid the child if there is an obstruction in his throat. It reviews some essential details for infants, such as how to give back blows and chest thrusts in a harmful way. Aiming at this particular audience explains why we’ve started covering a case designed for adults, not babies. By the end of this article, the readers will learn how to provide rescue aid and how to avert such situations by taking care of resources and being aware of the circumstantial factors that influence the chances of choking.
How to Recognize Signs a Baby is Choking

Identifying the signs of an infant choking is all the more critical for performing rescues. As a rule, a choking infant will suddenly be seen to struggle for breath with coughing or gagging on mucus. In cases where only partial airway blockage occurs and the infant tries to breathe, it may produce weak or shrill sounds. But when the airway is wholly slapped shut, the baby will be seen as unable to either cry, cough,h or make any sound while their faces will turn pale or blue due to oxygen deficiency. With any prying signs, look out for excessive saliva drooling or a scared and bewildered face and do something about it so the case can be de-escalated.
What are the common choking hazards for babies?
My findings indicate that the Strangest things to choke on for babies include small, complex types of food such as nuts, popcorn, candy, and such that the infant cannot bite well. Grape, hotdog, and cherry tomatoes are hazardous unless cut into smaller pieces. On the other hand, babies also put a lot of items in their mouths, so I put small toys, buttons, coins, deflated balloons, etc. Ensuring a thriving environment and monitoring mealtime or playtime can significantly curb these risks.
How can you tell if a baby is choking?
A baby suffering from choking might show some life-threatening signals, which should be regarded with extreme concern. Airway obstruction is indicated by the baby's failure to cry, cough, or make any other sound. The infant could be grunting or retracting his or her chest or have both nostrils and mouth open with no breath coming through and showing signs of cyanosis around the lips, face, or extremities, which appear blueish or pale, which indicates lack of sufficiency of oxygen. Fern drooling and/or a worried look are also some common signs. These symptoms need to be acknowledged instantly as they are key to allowing life-saving procedures to begin.
What should you do if a baby becomes silent?
If a baby suddenly goes quiet and you suspect choking, then initiate actions without delay but in a careful manner. Primarily, take stock if the baby is choking by observing if there is airflow or cause for combusting energy to cry, cough, or any noise. If this is the case, proceed to do the following.
1.Call Emergency Services: You could also ask someone else to place the call while dealing with the situation.2 .Offer Back Blows and Chest Thrusts (For Infants under 1 year of age):
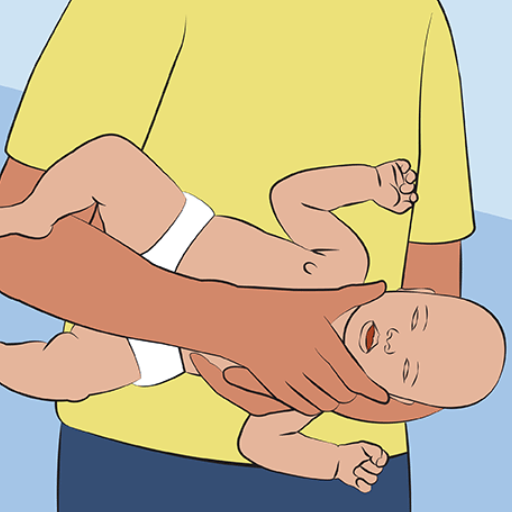
- Back Blows: The infant should be placed face down on your forearm, stabilising his or her head and neck before you deliver five measured blows to the upper middle back with your palm.
- Chest Thrusts: In case the obstruction doesn't go away, the baby can be placed on his or her back on your forearm or lap before proceeding to stick two fingers to the undersides of the nipples and push five times.
3 . Look for the Item: After each cluster of back blows and chest thrusts, look for items that the baby might be concealing or can pick up securely. Avoid placing your finger in the mouth and move it around, as this may cause the object to shift deeper.
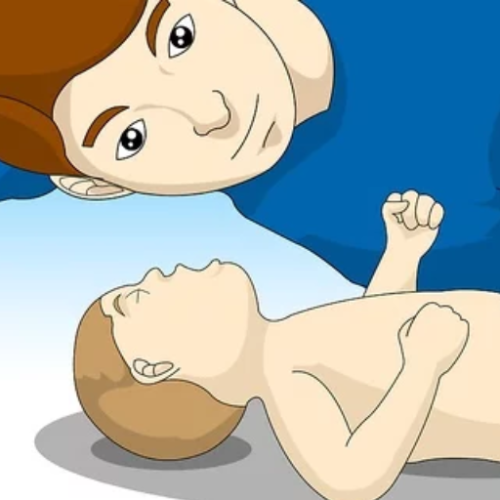
4 . If the baby choke,s do CPR: If the baby has choked and is unresponsive, line the baby on a flat surface and start infant CPR as follows:
- Chest Compressions: Compress the chest with two fingers (1.5 in or 1/3 of the chest depth ) at the speed of one hundred to hundred twenty beats every minute.
- Rescue Breaths: Slightly move the head backward and begin giving rescue breaths, ensuring the air goes in so the chest expands; aim for two soft breaths.
- Provide rescue and first aid until help is needed.
Choking is one leading cause of almost all of the baby’s complications, so it’s necessary for you always to consult a professional. Always perform CPR after the baby chokes.
What Immediate First Aid Steps Should Be Taken?

- Assess the Situation: Determine if the person is conscious and breathing. If they are choking but can cough or speak, encourage them to continue coughing to dislodge the object.
- Call for Emergency Assistance: Dial emergency services immediately if the person is having difficulty breathing or is unable to respond.
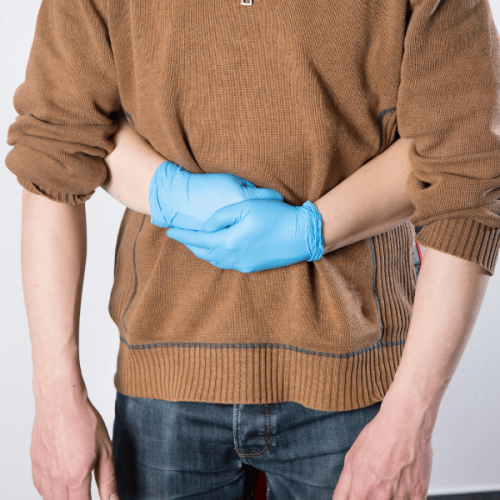
- For a Responsive Adult or Child Over 1-Year-Old:
- Perform the Heimlich Maneuver by standing behind the person, placing your arms around their waist, and delivering abdominal thrusts by pulling inward and upward just above the navel. Repeat until the object is expelled.
- For Infants Under 1 Year Old:
- Place the infant face down along your forearm, supporting their head and neck. Deliver five firm back blows between the shoulder blades, followed by five chest thrusts using two fingers in the center of the chest. Repeat this cycle.
- Administer CPR if Unresponsive: If the person becomes unresponsive, perform CPR, starting with chest compressions. Before each rescue breath, check the airway for an obstructing object.
Always follow up with a medical professional to ensure no residual complications remain, even if the choking incident is resolved.
How to perform back blows on a baby?
Performing back blows on an infant can be distressing for both the child and the parent. To perform back blows on a baby, I would use my controlling hand to position their head lower than their chest while using my forearm and letting my thigh act as a support. I would then proceed to back blows, delivering an average of five blows onto their back. After that, I would check to see if there was any obstruction, and if yes, use the chest thrust. Always ensure that you remain relaxed while performing the steps.
When and how to use chest thrusts?
Chest thrusts can be useful if a very young infant fails to respond to back blows. Gently strike the back with the fist or heel of the hand. Even if the baby stops breathing while being choked, it is still reasonable to employ this technique. The technique ensures that additional damage is avoided and provides the necessary force for expulsion in an airway obstruction case. The blocking object is displaced in a focused manner.
I remember performing chest when the infant or child was first placed on their back, putting my hand behind the baby’s head to support and gain more control over the child’s neck. Bears the head, clearly leaning shoulder and above the sternum, onto my forearm, resting so it is convenient for the operation. My thumbs followed the bottoms of the ribcage. They interlaced to cradle the head, and the index and middle fingers weren't used to reinforce and crush everything in the chest and around the tibia elbows, as the pressure needed to be varied, necessarily grasping onto the metacarpal ends before pressing them against the rib spine. That came about with five forceful voiding deposits against the sternum, quite surprisingly. Each motion was precisely and carefully executed and reached a depth of 1.5 inches (4 cm). Care had to be taken to ensure the chest was wholly relaxed or ready to take the blow of every thrust or press. This was succeeded by gradually thicknessing out the child’s capillaries. If pulling the baby’s or toddler’s chest through a set, there was a concern that it was still not fed properly; I also reached out for clinical assistance.
It’s important to use precision and appropriate power when doing chest thrusts to lessen the risk of injury to the infant’s ribs and/or internal organs.
Should you attempt abdominal thrusts on an infant?
Under no circumstances should you attempt to execute the Heimlich Maneuver on a baby who is less than a year old. Given their delicate anatomy, such maneuvers might result in violent internal damage, which might include the laceration of the liver or other organs. For a choking infant, the basic principles of back blows and chest thrusts that were mentioned earlier will ensure that the appropriate tactics are used, which are crafted bearing their safety and biomechanics in mind.
How to Minimize the Risk of Choking in Babies?
Many serious accidents can happen if the infant is not fed or taken care of properly. If a baby has to eat, the adult needs to assist the baby throughout the meal, and the baby must be in an upright position to avoid the risk of choking. It is advisable to give the baby food that is easy to swallow and thoroughly safe for the infant, such as soft pieces of banana or mushed potatoes. This also means avoiding round-shaped food items such as whole grapes, nuts, chewing gum, and popcorn extras. Other than this, ensure that sharp-edged toys or small pieces of a toy that can come off are not close to the infant, or the baby can not chew them as they can be a choking hazard. Also, help educate other family members who can assist with the baby by providing them with the same education.
How can introducing solid foods safely reduce risks?
Babies should be introduced to solid foods safely, and gradual exposure should be ensured to the mechanical chewing and swallowing of the mouth and its surrounding structures. It is, therefore, correct to start with food substances that they can quickly try, such as mashed bananas, cooked carrots, or finely ground cereals, and then progress to harder ones. Food should not be placed in the mouth in larger than ¼ inch (6 millimeters) cubes, and it should be understood that other safe cuts can be made because large cut sizes are a threat to choking. Only one new food should be fed to the infant at a time to enable him to identify specific reactions that may indicate allergic reactions. Also, always put the infant in a high chair supporting him so that he can safely swallow what is lapsed. Never try to force the infant to open her mouth; at least try to do it less, not to impose a burden on him; and do not instruct him to eat quickly but rather allow him to eat as slowly as he wishes. Implementing all the measures described above, accompanied by permanent parental control during the meals, may significantly reduce already minimal existing risks.
What are the best ways to prevent choking hazards?
To minimize the risk of choking, I take a few precautions. To begin with, I see to it that all meals are adequately diced into smaller particles that neither exceed ¼ inch (6mm) in depth or width. Additionally, I reduce the likelihood of using round, complex, or sticky foods such as whole grapes or nuts, popcorn, and chunky meat or cheese, which pose higher dangers. When food is ingested, I sit the child on a high chair and supervise closely, ensuring the child is in an upright position to allow easy and safe swallowing. Furthermore, I promote hygienic practices such as a solid focus on the meal and not distracting the child with toys or screens during food to promote safe and efficient chewing and swallowing. In addition, I am aware of the various suitable meals for children of different ages and ensure I remember the proper methods of dealing with choking,g such as the Heimlich maneuver.
When should you seek first aid advice or call emergency services?

The American Academy of Pediatrics has made specific guidelines for dealing with choking cases and administering first aid. If a child has airway obstruction due to food or any foreign object and cannot communicate or show signs of an improved attempt to breathe, the child’s skin becomes bluish, or constant coughing is observed from the child. In such cases, you can first administer the first aid technique, which includes micromanagement of back blows and abdominal thrusts. Still, it is always advisable to seek some form of professional training for this. Suppose the forceful coughing doesn’t relieve the object firmly lodged in the child’s airway, and it attempts to cough forcefully through a few inhalations without yielding any productive result during submersion. In that case, notifying the authorities is crucial and should be done as soon as possible to provide the child with the appropriate medical care required. Even if the object is completely removed and no remains of the ailment are seen, it is best to consult a physician who can provide you with a first-aid perspective, which might further help the child.
When should you call 911?
You should call 911 immediately in the following situations:
- Complete Airway Obstruction:
- The child is unable to breathe, cough, or speak at all.
- There are visible signs such as a bluish skin tone (cyanosis) or loss of consciousness.
- Unresponsive Child:
- If the child becomes unresponsive during the choking incident, start CPR if trained and contact emergency services immediately.
- Prolonged Distress:
- The object causing the blockage does not dislodge after performing appropriate first aid techniques (e.g., back blows and abdominal thrusts).
- Post-Choking Complications:
- Even if the object appears to be entirely removed, call 911 if the child has difficulty breathing, continues to cough excessively, or shows signs of respiratory distress, as this could indicate airway trauma or residual blockage.
Always act swiftly and calmly, ensuring assistance is coming while applying the appropriate first aid measures.
What to do when help arrives?
Help is coming, and I would keep calm and concentrate on the child’s condition. If the patient is still alive but is gasping for air, which means he is still conscious, I would continue the intervals of 5 back slaps and five thrusts. This would be done by making sure the technique is on point. In the cases where the primary patient no longer responds, I would start CPR immediately. In cases where I passed the course, I would perform the following ventilation steps — 30 chest push exercises. These compressions are done to a depth of around two inches (5 cm) and have a tempo of 100 to 120 push tugs every minute; after that, I follow it with two mouth-to-mouth resuscitation. Proper recognition is vital, and consideration of the mouth of the child should be discouraged from pushing deep into the blockage unless the item can be noticed from the view. This ensures nothing is moved unless a more qualified individual arrives.
Why is First Aid Training Crucial for Parents?

Providing parents with first aid training is an essential part of maintaining child welfare as it can help the parent to save the child’s life when in danger. Children are naturally inquisitive, and parents would require knowing how to deal with situations such as a child choking, getting burns, etc. It also helps the parents to have the requisite physiological disposition and the knowledge of any situation quickly while professional assistance is en route. Moreover, such skills ensure parents do not panic, evaluate the circumstances, and provide timely and specific care. So to sum it up, first aid training helps to equip the parents with the means and the ability to protect their child in crucial circumstances.
How can St John Ambulance training help save lives?
Training with St John Ambulance can save lives by giving practical insight into essential first aid skills. From such courses, I have mastered dealing with simple life-threatening issues like CPR, choking, severe bleeding, or burns. The organized system allows me to analyze problems and take action that might lessen adverse effects or prevent higher-order ones. The segment uses repetition, thereby infusing crucial skills within me to ensure I am ready to perform during competitive activities. This information enables me to become quite helpful in deadly situations as St John Ambulance does not train in vain.
Are there training courses for new parents?
Indeed, there are educational programs for first-time mothers and fathers, which include elements like the care of a woman during pregnancy and after giving birth, the development of the baby, and even parenting skills. Usually, such courses are offered over the Internet or at hospitals, community institutions, or organizations. Many programs also have technical components such as essential management of infant feeding methods, baby sleep safety, including the AAP's safe sleep recommendations, and basic first aid for infants. The time spent in each course varies from one to several hours, and the cost can run from $50 to $200 based on the course specification and the service provider. It is within the parent’s right to ensure the course he or she has enrolled in meets endorsed health and safety requirements.
What are the benefits of a first-aid app?
A first aid application can provide a lifesaving advantage to a person facing a medical emergency. In an emergency, time is essential; thus, readily available first aid information can help save lives. Some of the key benefits that this app provides include:
- Convenient to Use: First aid apps work without the internet and instruct users on how to react to life-threatening situations like CPR or choking. These apps are available offline, so the user can access the information and follow the steps even in critical situations.
- In Case Of An Emergency: In certain apps, some timetables include to-do lists or audio messages that guide users on assisting people, marking the beginning of first aid helping apps. For example, the issued American Heart Association prescribes around 100 to 120 CPR per minute.
- Centralized Emergency Integration: A few of these applications offer their users complete information on their contacts, and with just a tap on the app, the user can directly call the local medical services nearest their geographic location.
- Parenting: The responsive design covers complete tutorials and includes videos on saving lives and teaching the proper steps in an emergency to be better prepared while simplifying the overall process.
- Improved Features: First Aid applications have advanced features that help users map nearby hospitals with clear guidelines to reach them.
A detailed explanation outlining how offline capabilities, voice guidance, and offline information retention make first aid applications versatile. User interface beta testing and approval by the respective mandates improve their reliability and efficiency even more.
References
Choking First aid ThoraxFrequently Asked Questions (FAQ)
Q: What should I do if my baby is gagging and seems to be choking?
A: If your baby is gagging, it may be a sign that the airway is partially blocked. Stay calm and observe if the infant is coughing forcefully. If they can cough, let them continue, which may dislodge the blockage. If the infant is still choking, follow the choking first aid steps.Q: How do I perform choking first aid for infants under 1 year old?
A: For choking first aid for babies, place the baby face down along your forearm, supporting their head and neck. With the heel of your hand, give up to 5 quick back blows between the infant's shoulder blades. If the blockage does not dislodge, turn the infant over and give up to 5 chest thrusts along the infant's chest using two fingers.Q: When should I call for emergency help if my child is choking?
A: If the baby becomes unresponsive or if the blockage does not clear after trying the choking first aid steps, call emergency services immediately. Continue to assist as instructed by the operator until help arrives.Q: What are some everyday objects that cause choking in infants?
A: Small objects such as toys, food pieces, and household items can quickly get stuck in a baby’s airway. Always ensure these items are out of reach to prevent choking.Q: How can I prevent choking in my baby?
A: Prevent choking by keeping small objects out of reach, supervising meal times, and ensuring the baby is seated upright while eating. Avoid giving them foods that quickly get stuck, such as nuts or hard candies.Q: What should I do if the infant is coughing forcefully?
A: If the infant is coughing forcefully, it indicates that the airway is partially blocked, and they may be able to clear it themselves. Encourage them to cough and do not interfere unless they stop coughing or become unable to breathe.Q: What is the difference between gagging and actual choking in infants?
A: Gagging is a reflex that helps protect the airway and often resolves independently. Actual choking occurs when the airway is blocked and requires immediate intervention, such as the choking first aid steps.Q: How can using CPR help when a choking baby becomes unresponsive?
A: If a choking baby becomes unresponsive, CPR can help maintain circulation and oxygenation until the blockage is removed. Begin with chest compressions and follow the steps instructed by emergency personnel or the Red Cross guidelines.Q: Can vomiting be a sign that the blockage is clearing?
A: Sometimes, vomiting can occur if the blockage is dislodged or the baby is trying to clear the airway. If vomiting happens, ensure the baby is in a safe position to prevent aspiration.Q: What are the signs that a baby may be choking?
A: Signs that a baby may be choking include difficulty breathing, coughing or gagging, a high-pitched noise when breathing, or the inability to cry or make noise. The infant might also display distress, a bluish skin color, or become unresponsive.Q: What should I do immediately if my baby is choking?
A: If your baby is choking, call for emergency help and start choking first aid immediately. Position the baby face down along your forearm, supporting the infant's chest in your hand. Give up to 5 back blows between the infant's shoulder blades using the heel of your hand.











 Login with Google
Login with Google Login with Facebook
Login with Facebook