Low blood pressure, or hypotension, is a condition that often flies under the radar compared to its counterpart, hypertension. However, it plays a critical role in overall health and can lead to symptoms ranging from mild dizziness to life-threatening complications like shock. This comprehensive guide explores the causes, symptoms, and types of low blood pressure, as well as practical strategies for diagnosis, treatment, and management. Whether you're experiencing occasional lightheadedness or dealing with chronic hypotension, understanding the nuances of this condition is key to maintaining your well-being.
Understanding Low Blood Pressure
What is Hypotension? A Practical Overview
Low blood pressure, or hypotension, happens when the force of blood moving through your arteries is lower than normal. While it might seem harmless, it can lead to symptoms like dizziness, fainting, or even life-threatening complications like shock if blood flow to vital organs is severely reduced. For some, low blood pressure is normal and symptom-free. For others, it can signal an underlying issue that needs attention. Understanding your body’s response is key to knowing when to act.
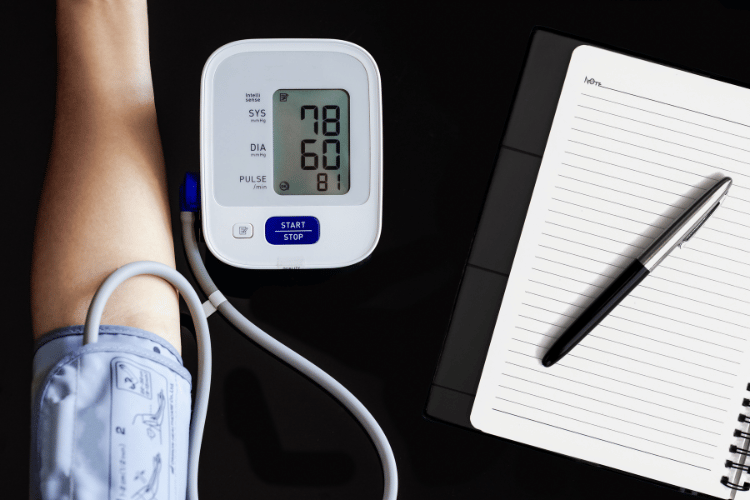
Normal vs. Low Blood Pressure: What Do the Numbers Mean for You?
Blood pressure readings consist of two numbers:
- Systolic pressure (top number): The pressure when your heart pumps blood.
- Diastolic pressure (bottom number): The pressure when your heart rests between beats.
A typical reading is around 120/80 mmHg, while hypotension is generally defined as below 90/60 mmHg. However, these numbers aren’t one-size-fits-all. For some, a reading of 85/55 might be perfectly fine, while for others, it could cause symptoms like fatigue or dizziness. The key takeaway? Pay attention to how you feel, not just the numbers.
How Blood Pressure is Measured and Why It Matters
Blood pressure is measured using a cuff (sphygmomanometer) that inflates around your arm. This simple test provides valuable insights into your heart and overall health:
- High readings may indicate stress on your heart and arteries.
- Low readings could mean your organs aren’t getting enough blood flow.
If you experience symptoms like fainting, blurred vision, or extreme fatigue, regular monitoring can help identify patterns and guide treatment. Knowing your baseline blood pressure and how it fluctuates is crucial for managing your health effectively.
Symptoms of Low Blood Pressure
Common Warning Signs: What to Watch For
Low blood pressure (hypotension) can show up in different ways, depending on the cause and severity. Here are the most common symptoms and what they mean for you:
- Dizziness or Lightheadedness: Often triggered by standing up quickly or sudden movements, this is a key sign that your brain isn’t getting enough blood flow.
- Fatigue: Feeling unusually tired or drained could mean your body is struggling to circulate oxygen-rich blood effectively.
- Blurred Vision: Temporary vision issues may occur when blood flow to the eyes is reduced.
- Fainting (Syncope): In more severe cases, a lack of blood flow to the brain can cause you to pass out.
- Nausea: Some people experience an upset stomach or queasiness as a result of low blood pressure.
If you notice these symptoms frequently, it’s important to track when they occur and consult a healthcare provider to identify the underlying cause.
Recognizing a Sudden Drop in Blood Pressure: When to Take Action
A sudden and significant drop in blood pressure, known as acute hypotension, can be life-threatening. This might happen due to severe dehydration, blood loss, or a medical emergency like septic shock. Key warning signs include:
- Cold, clammy skin
- Rapid, shallow breathing
- Confusion or difficulty focusing
- Weak, rapid pulse
What to do: If you or someone else experiences these symptoms, especially after an injury or illness, seek emergency medical help immediately. Acting quickly can prevent serious complications.
Postural Hypotension: Symptoms and Simple Fixes
Postural hypotension (orthostatic hypotension) happens when your blood pressure drops after standing up too quickly. This is common in older adults, people on certain medications, or those who are dehydrated. Symptoms include:
- Dizziness or lightheadedness right after standing.
- Blurred or “tunnel” vision.
- Weakness or feeling unsteady.
- Fainting in severe cases.
How to manage it:
- Stand up slowly, especially after sitting or lying down for a long time.
- Stay hydrated to maintain healthy blood volume.
- If symptoms persist, talk to your doctor about possible underlying causes or medication adjustments.
Causes of Low Blood Pressure
Everyday Triggers: What Can Cause Temporary Drops?
Low blood pressure often results from common, everyday factors that disrupt your body’s ability to maintain normal circulation. Here’s what to watch for:
- Dehydration: Losing more fluids than you take in—whether from sweating, vomiting, or diarrhea—reduces blood volume and lowers blood pressure. Staying hydrated is key, especially during hot weather or illness.
- Blood Loss: Injuries, surgeries, or internal bleeding can significantly reduce the amount of blood circulating in your body, leading to hypotension. Seek immediate medical attention if you suspect significant blood loss.
- Medications: Drugs like diuretics, beta-blockers, or antidepressants can lower blood pressure as a side effect. If you notice symptoms like dizziness or fatigue after starting a new medication, consult your doctor about possible adjustments.
What to do: These triggers are often temporary and manageable. Drink plenty of fluids, follow your doctor’s advice, and monitor your symptoms to prevent complications.
Underlying Health Conditions: When Low Blood Pressure Signals Something Serious
Chronic or severe hypotension may point to underlying health issues that need medical attention. Here are some common culprits:
- Heart Problems: Conditions like heart failure, a slow heart rate (bradycardia), or valve disorders can reduce blood flow and cause persistent low blood pressure.
- Endocrine Disorders: Hormonal imbalances from conditions like adrenal insufficiency or hypothyroidism can disrupt blood pressure regulation.
- Severe Infections (Sepsis): Infections that spread throughout the body can lead to septic shock, a life-threatening drop in blood pressure.
- Nervous System Disorders: Diseases like Parkinson’s or autonomic neuropathy can interfere with the body’s ability to regulate blood pressure effectively.
What to do: If you suspect an underlying condition, consult a healthcare provider for a thorough evaluation. Early diagnosis and treatment are crucial for managing persistent hypotension.
How High Blood Pressure Treatments Can Lead to Low Blood Pressure
Ironically, managing high blood pressure can sometimes result in blood pressure dropping too low. Here’s how:
- Overmedication: Taking too high a dose of antihypertensive drugs, like ACE inhibitors or calcium channel blockers, can cause excessive drops in blood pressure.
- Combination Therapies: Using multiple medications to control high blood pressure increases the risk of hypotension, especially in older adults.
- Lifestyle Changes: Healthy habits like weight loss or reduced salt intake can amplify the effects of medication, leading to unintended drops in blood pressure.
What to do: If you’re treating high blood pressure and notice symptoms of hypotension, such as dizziness or fainting, talk to your doctor. They can adjust your medication or treatment plan to find the right balance.
Types of Low Blood Pressure
Orthostatic Hypotension: Feeling Dizzy When You Stand
Orthostatic hypotension, or postural hypotension, happens when your blood pressure drops significantly after standing up. This occurs because gravity pulls blood toward your lower body, temporarily reducing blood flow to your brain. Symptoms to watch for:- Dizziness or lightheadedness right after standing.
- Blurred vision or a sense of instability.
- Fainting in severe cases.
- Stand up slowly, especially after sitting or lying down for a long time.
- Stay hydrated to maintain healthy blood volume.
- Consider wearing compression stockings to improve circulation.
- If symptoms persist or worsen, consult a healthcare provider to rule out underlying issues.

Neurally Mediated Hypotension (NMH): Fainting After Standing Too Long
Neurally mediated hypotension occurs when standing for extended periods causes a miscommunication between your heart and brain, leading to a sudden drop in blood pressure. This can result in fainting or near-fainting episodes. Symptoms to watch for:- Nausea, dizziness, or fatigue before fainting.
- A feeling of weakness or instability after standing for too long.
- Avoid standing for long periods, especially in hot or crowded environments.
- Stay hydrated and consider increasing salt intake (only under medical supervision).
- In some cases, medications may be prescribed to help regulate blood pressure.
- If fainting episodes are frequent, consult a doctor for a tailored treatment plan.
Severe Hypotension: When It’s a Medical Emergency
Severe hypotension, also known as shock, is a life-threatening condition where blood pressure drops so low that vital organs like the brain, heart, and kidneys don’t get enough blood. Causes include:- Septic shock: Triggered by severe infections.
- Cardiogenic shock: Caused by heart failure.
- Hypovolemic shock: Due to significant blood or fluid loss.
- Anaphylactic shock: A severe allergic reaction.
- Cold, clammy skin.
- Rapid, shallow breathing.
- Confusion or difficulty concentrating.
- A weak, rapid pulse.
Diagnosis and Treatment
How Doctors Diagnose Low Blood Pressure: What to Expect
Diagnosing low blood pressure involves more than just a quick blood pressure reading. Here’s what you can expect during the process:- Medical History: Your doctor will ask about your symptoms, lifestyle habits, and any medications you’re taking. Be prepared to share details about when symptoms occur (e.g., after standing, eating, or exercising).
- Physical Exam: Blood pressure will be measured in different positions—lying down, sitting, and standing—to check for conditions like orthostatic hypotension.
- Diagnostic Tests:
- Blood Tests: To check for anemia, dehydration, or hormonal imbalances.
- Electrocardiogram (ECG): To detect heart rhythm issues or other cardiac problems.
- Echocardiogram: An ultrasound to assess the heart’s structure and function.
- Tilt Table Test: Used to diagnose conditions like neurally mediated hypotension by monitoring blood pressure and heart rate changes when your body is tilted upright.

Effective Treatments: From Lifestyle Adjustments to Medical Interventions
The right treatment for low blood pressure depends on its cause and severity. Here’s a breakdown of common approaches:- Lifestyle Adjustments:
- Stay hydrated by drinking plenty of water throughout the day.
- Avoid alcohol, which can lower blood pressure further.
- Stand up slowly, especially after sitting or lying down for long periods.
- Eat small, frequent meals to prevent blood pressure drops after eating.
- Medications:
- Fludrocortisone: Helps increase blood volume to raise blood pressure.
- Midodrine: Tightens blood vessels to improve circulation and prevent drops in blood pressure.
- Addressing Underlying Conditions:
- Treating heart problems, infections, or hormonal imbalances is crucial for long-term management.
Managing Blood Pressure with Practical Strategies
In addition to medical treatments, these everyday strategies can help you manage low blood pressure and reduce symptoms:- Diet:
- Increase your salt intake (only under medical supervision).
- Focus on small, balanced meals to avoid post-meal blood pressure drops.
- Hydration:
- Drink water consistently throughout the day to maintain blood volume.
- Consider electrolyte-rich drinks if you’re sweating excessively or feeling dehydrated.
- Compression Stockings:
- These can prevent blood from pooling in your legs, improving circulation and reducing symptoms of orthostatic hypotension.
Practical FAQs About Low Blood Pressure
What Are the Most Common Causes of Sudden Drops in Blood Pressure?
Sudden drops in blood pressure, or acute hypotension, can happen for several reasons. Here are the most common triggers and what to do:- Dehydration: Losing fluids through excessive sweating, vomiting, or diarrhea reduces blood volume.
- What to do: Drink water or an electrolyte-rich beverage to rehydrate quickly.
- Blood Loss: Injuries, surgeries, or internal bleeding can cause a rapid drop in blood pressure.
- What to do: Seek immediate medical attention if you suspect significant blood loss.
- Severe Infections (Sepsis): Infections spreading through the body can lead to septic shock.
- What to do: Call emergency services if symptoms like fever, confusion, or rapid breathing accompany low blood pressure.
- Allergic Reactions (Anaphylaxis): Severe allergies can cause blood vessels to widen, leading to a sharp drop in pressure.
- What to do: Use an epinephrine auto-injector (if available) and seek emergency care immediately.
How Can I Recognize and Respond to Symptoms of Hypotension?
Low blood pressure symptoms can range from mild to severe. Here’s how to identify and respond:- Common Symptoms: Dizziness, fainting, blurred vision, fatigue, or nausea.
- Severe Symptoms: Confusion, cold or clammy skin, rapid breathing, or a weak pulse.
- Sit or Lie Down Immediately: Prevent falls and improve blood flow to the brain.
- Elevate Your Legs: This helps blood return to your heart and brain more quickly.
- Drink Water: If dehydration is a possible cause, rehydrate as soon as possible.
- Seek Medical Help: If symptoms persist, worsen, or occur after an injury or illness, consult a healthcare provider.
Can Low Blood Pressure Lead to Serious Health Risks?
Yes, while mild hypotension is often harmless, severe or chronic low blood pressure can pose significant risks:- Shock: A life-threatening condition where blood flow to vital organs is critically reduced.
- Organ Damage: Prolonged low blood pressure can impair the function of the brain, heart, and kidneys.
- Falls and Injuries: Dizziness or fainting increases the risk of accidents, especially in older adults.
What Role Do Blood Vessels Play in Regulating Blood Pressure?
Blood vessels are key players in maintaining stable blood pressure. Here’s how they work:- Vasoconstriction: Narrowing of blood vessels increases pressure to ensure adequate blood flow during low-pressure situations.
- Vasodilation: Widening of blood vessels reduces pressure when necessary, such as during rest or after exercise.
Frequently Asked Questions
Q: What are the common causes of low blood pressure?
A: Low blood pressure, or hypotension, happens due to several factors. Common causes include blood loss, which reduces blood volume, and dehydration, which decreases blood flow. Certain medications, heart conditions, and severe allergic reactions can also trigger dizziness and sudden drops in blood pressure.Q: What symptoms of low blood pressure should I watch for?
A: Watch for symptoms like dizziness, fainting, fatigue, and blurred vision. A sudden drop in blood pressure may also cause nausea or confusion. Monitoring these signs is crucial, as they might indicate the need for medical attention.Q: How does postural hypotension relate to low blood pressure?
A: Postural hypotension occurs when blood pressure drops significantly after standing up, leading to dizziness or fainting. This happens because a sudden change in position affects blood flow, causing temporary symptoms.Q: What types of low blood pressure are there?
A: Low blood pressure includes types like orthostatic hypotension and neurally mediated hypotension. Orthostatic hypotension occurs when standing causes a sudden drop in blood pressure, while neurally mediated hypotension happens after standing for long periods, often resulting in fainting.Q: Can low blood pressure lead to serious health issues?
A: Yes, low blood pressure can cause serious problems, such as shock, if left untreated. A severe drop in blood pressure reduces blood flow to vital organs, potentially causing damage. Identifying the cause and seeking treatment is essential to prevent complications.Q: How can I treat low blood pressure effectively?
A: You can treat low blood pressure by making lifestyle changes, such as drinking more fluids, increasing salt intake (under medical supervision), or wearing compression stockings. In some cases, doctors may prescribe medications to raise blood pressure and improve circulation.Q: What can cause a sudden drop in blood pressure?
A: Sudden drops in blood pressure can result from dehydration, blood loss, or severe allergic reactions. Standing up too quickly can also cause a temporary drop, leading to dizziness or lightheadedness.Q: How does high blood pressure relate to low blood pressure?
A: High blood pressure treatments can sometimes lead to low blood pressure. Medications used to lower high blood pressure may cause it to drop too much, resulting in symptoms of hypotension like dizziness or fatigue.Q: What role do blood vessels play in low blood pressure?
A: Blood vessels are key to regulating blood pressure. When blood vessels dilate or widen, blood pressure decreases. Conditions that affect blood flow, such as heart failure or reduced blood volume, can also contribute to low blood pressure.Concluding Summary
Low blood pressure may seem harmless, but its impact on your health can vary widely depending on the cause and severity. From everyday triggers like dehydration to more serious conditions such as heart problems or septic shock, recognizing the signs and understanding the underlying factors is essential. With proper diagnosis, lifestyle adjustments, and medical interventions, managing hypotension is entirely possible. By staying informed and proactive, you can take control of your blood pressure and safeguard your overall health.















 Login with Google
Login with Google Login with Facebook
Login with Facebook