Understanding the different types of bleeding is crucial for effective emergency response, as it equips individuals with the knowledge to act swiftly and appropriately. Quick identification and treatment can mean the difference between life and death, highlighting the importance of recognizing the severity and nature of bleeding in critical situations.
What is Arterial Bleeding?
Definition and Characteristics
Arterial bleeding is a severe and potentially life-threatening condition that occurs when an artery, one of the blood vessels responsible for carrying oxygen-rich blood from the heart to the rest of the body, is damaged. Unlike venous bleeding, which involves blood flowing steadily from a vein, arterial bleeding is characterized by bright red blood that spurts or gushes in rhythm with the heartbeat. This pulsating flow is due to the high pressure within the arteries, making this type of bleeding more dangerous and harder to control. The rapid loss of blood associated with arterial bleeding can lead to hypovolemic shock. In this condition, the body cannot maintain adequate blood pressure and oxygen delivery to vital organs. Immediate intervention is critical to prevent severe complications or death. Understanding the unique characteristics of arterial bleeding is essential for recognizing and responding to this medical emergency effectively.
Arterial Bleeding
Causes and Common Scenarios
Arterial bleeding can result from a variety of causes, most of which involve significant trauma or injury. Some of the most common scenarios include:- Penetrating Injuries: Stab wounds, gunshot injuries, or deep lacerations caused by sharp objects can sever arteries, leading to arterial bleeding.
- Blunt Force Trauma: High-impact accidents, such as car crashes or falls from a height, can rupture arteries, especially in areas where they are close to the surface or unprotected by bone.
- Surgical Complications: In rare cases, arterial bleeding may occur as a complication during or after surgical procedures, particularly those involving major blood vessels.
- Medical Conditions: Certain conditions, such as aneurysms or arterial ulcers, can weaken the walls of arteries, making them more prone to rupture.
- Industrial or Workplace Accidents: Injuries involving heavy machinery or tools can also lead to arterial damage, especially in high-risk professions.
Symptoms and Visual Indicators
Recognizing the symptoms and visual signs of arterial bleeding is crucial for timely intervention. The most distinctive indicator is the bright red color of the blood, which is due to its high oxygen content. Unlike venous bleeding, which is darker and flows steadily, arterial bleeding is marked by spurts or jets of blood that correspond to the heartbeat. Other symptoms and signs include:- Rapid Blood Loss: The high pressure in arteries causes blood to escape quickly, leading to significant blood loss in a short period.
- Pulsating Flow: The rhythmic spurting of blood is a hallmark of arterial bleeding and indicates the involvement of a major artery.
- Shock Symptoms: As blood loss progresses, the individual may exhibit signs of shock, such as pale or clammy skin, rapid breathing, dizziness, confusion, or loss of consciousness.
- Pain and Swelling: Depending on the location of the injury, there may be intense pain and localized swelling around the wound.
- Visible Arterial Damage: In some cases, the damaged artery may be visible within the wound, further confirming the source of the bleeding.
What is Venous Bleeding?
Definition and Characteristics
Venous bleeding occurs when a vein, the blood vessel responsible for carrying deoxygenated blood back to the heart, is damaged. Unlike arterial bleeding, which is characterized by bright red, spurting blood, venous bleeding typically involves a steady, slow-to-moderate flow of darker red blood. This darker color is due to the lower oxygen content in venous blood. While venous bleeding is generally less forceful than arterial bleeding, it can still be dangerous, especially if a large vein is involved or the bleeding is not controlled promptly. One of the defining characteristics of venous bleeding is its consistent flow, which does not pulse in rhythm with the heartbeat. However, if a major vein, such as the femoral or jugular vein, is injured, the blood loss can be rapid and life-threatening. Immediate action is necessary to control the bleeding and prevent complications such as hypovolemic shock or air embolism, which can occur if air enters the damaged vein.
Causes and Common Scenarios
Venous bleeding can result from a variety of injuries or medical conditions. Some of the most common causes and scenarios include:- Lacerations and Cuts: Accidental cuts from sharp objects, such as knives or glass, can sever veins, leading to venous bleeding.
- Blunt Trauma: Injuries from falls, car accidents, or sports-related impacts can damage veins, especially those close to the skin's surface.
- Surgical Procedures: Venous bleeding may occur during or after surgery, particularly in procedures involving veins or areas with dense vascular networks.
- Varicose Veins: In individuals with varicose veins, even minor injuries can cause significant venous bleeding due to the increased pressure within the veins.
- Puncture Wounds: Injuries caused by needles, nails, or other pointed objects can penetrate veins, resulting in bleeding.
Symptoms and Visual Indicators
Recognizing the symptoms and visual signs of venous bleeding is essential for effective first aid and medical intervention. The most noticeable indicator is the steady flow of dark red blood from the wound, which contrasts with the bright red, spurting blood seen in arterial bleeding. Other symptoms and signs include:- Consistent Blood Flow: The bleeding is typically continuous and steady, without the pulsating rhythm associated with arterial bleeding.
- Dark Red Color: The blood appears darker due to its lower oxygen content, making it a key visual cue for identifying venous bleeding.
- Swelling Around the Wound: As blood pools in the surrounding tissues, swelling may develop near the injury site.
- Pain and Tenderness: Depending on the severity and location of the injury, the individual may experience localized pain or tenderness.
- Signs of Blood Loss: In cases of significant venous bleeding, symptoms such as dizziness, weakness, pale skin, or rapid breathing may indicate the onset of shock.
Key Differences Between Arterial and Venous Bleeding
Detailed Comparison Table
Below is an expanded comparison table highlighting the key differences between arterial and venous bleeding, including additional criteria such as healing time, risk of complications, and first aid measures:
| Criteria | Arterial Bleeding | Venous Bleeding |
|---|---|---|
| Source of Bleeding | Arises from arteries that carry oxygen-rich blood away from the heart. | Originates from veins that transport deoxygenated blood back to the heart. |
| Color of Blood | Bright red due to high oxygen content. | Dark red or maroon due to low oxygen levels. |
| Flow Pattern | Blood spurts rhythmically in sync with the heartbeat. | Blood flows steadily and continuously without spurting. |
| Pressure | High pressure, making it difficult to control. | Lower pressure, making it easier to manage. |
| Severity | Extremely severe and life-threatening if untreated. | Less severe but still requires prompt attention to prevent complications. |
| Control Measures | Requires firm pressure, elevation, and often a tourniquet for severe cases. | Controlled with direct pressure, elevation, and clean dressings. |
| Associated Symptoms | Rapid blood loss, pale skin, shock, fainting, and loss of consciousness. | Swelling, bruising, pooling of blood, and lightheadedness in severe cases. |
| Healing Time | Longer healing time due to the high pressure and potential for tissue damage. | Generally shorter healing time if properly treated and no complications arise. |
| Risk of Complications | High risk of shock, organ failure, and death if not treated immediately. | Risk of infection, blood clots, or venous insufficiency if left untreated. |
| Common Causes | Severe trauma, deep lacerations, or punctures to major arteries. | Cuts, lacerations, or punctures to veins, often from accidents or minor injuries. |
| First Aid Approach | Immediate medical attention, firm pressure, and tourniquet application if necessary. | Direct pressure, elevation, and monitoring for signs of infection or complications. |
First Aid for Arterial Bleeding
Step-by-Step Guide to Managing Arterial Bleeding
Arterial bleeding is a medical emergency that requires immediate action to prevent life-threatening blood loss. Follow these steps to control the bleeding effectively:- Call Emergency Services: Dial emergency services immediately. Arterial bleeding is life-threatening, and professional medical help is essential. While waiting for help, proceed with first aid.
- Apply Direct Pressure: Use a clean cloth, gauze, or bandage to press firmly on the wound. Direct pressure helps slow the bleeding by compressing the damaged artery. If the bleeding soaks through the material, do not remove it; instead, add more layers and continue applying pressure.
- Elevate the Wounded Area: If possible, raise the injured limb above the level of the heart. Elevation reduces blood flow to the area, making it easier to control the bleeding. Be cautious not to move the limb excessively, as this could worsen the injury.
- Use a Tourniquet (If Necessary): If the bleeding cannot be controlled with pressure alone and you are trained to use a tourniquet, apply it above the wound. Tighten it until the bleeding stops. Note the time of application and inform medical personnel upon their arrival.
- Monitor for Signs of Shock: Keep an eye on the injured person for symptoms of shock, such as pale skin, rapid breathing, or fainting. If signs of shock are present, lay the person down, elevate their legs slightly, and keep them warm with a blanket.
- Keep the Wound Covered: Once the bleeding is under control, cover the wound with a sterile dressing or bandage to protect it from infection. Avoid removing the dressing until medical professionals take over.
Common Mistakes to Avoid
When providing first aid for arterial bleeding, it’s crucial to avoid these common errors:- Delaying Action: Hesitating to apply pressure or call for help can lead to rapid blood loss. Act immediately to control the bleeding.
- Removing Soaked Dressings: Taking off blood-soaked gauze can disrupt clot formation and worsen the bleeding. Always add more layers instead of removing the existing ones.
- Improper Tourniquet Use: Applying a tourniquet incorrectly can cause additional damage. Only use a tourniquet if you are trained, and ensure it is placed above the wound, not directly on it.
- Failing to Monitor for Shock: Ignoring signs of shock can lead to severe complications. Always check for symptoms like pale skin, dizziness, or rapid breathing and take appropriate measures.
- Using Unclean Materials: Applying non-sterile items to the wound increases the risk of infection. Use clean or sterile materials whenever possible.
When to Use a Tourniquet and How to Apply It Safely
A tourniquet is a last-resort tool for controlling severe arterial bleeding when direct pressure and elevation are not enough. It is most effective for injuries to the arms or legs. Here’s how to use it safely:- Position the Tourniquet: Place the tourniquet 2-3 inches above the wound, avoiding joints like elbows or knees. Ensure it is on the upper part of the limb and not directly over the injury.
- Tighten the Tourniquet: Pull the strap tightly and secure it in place. Use the windlass (a rod or stick) to twist the tourniquet until the bleeding stops. Secure the windlass to maintain pressure.
- Note the Time: Record the exact time the tourniquet was applied. This information is critical for medical professionals, as prolonged use can cause tissue damage.
- Do Not Loosen the Tourniquet: Once applied, do not loosen or remove the tourniquet until medical help arrives. Loosening it can cause a sudden rush of blood and worsen the situation.
- Monitor the Patient: Keep the injured person calm and monitor for signs of shock. Reassure them that help is on the way.
First Aid for Venous Bleeding
Step-by-Step Guide to Managing Venous Bleeding
Venous bleeding, while less forceful than arterial bleeding, still requires prompt attention to prevent excessive blood loss and complications. Follow these steps to manage venous bleeding effectively:- Apply Direct Pressure: Use a clean cloth, gauze, or bandage to press firmly on the wound. Direct pressure helps slow the steady flow of blood and encourages clot formation. If the bleeding continues, do not remove the initial dressing; instead, add more layers on top and maintain pressure.
- Elevate the Affected Area: If possible, raise the injured limb above the level of the heart. Elevation reduces blood flow to the wound, making it easier to control the bleeding. Ensure the injured person is comfortable and avoid excessive movement of the limb.
- Secure the Dressing: Once the bleeding slows or stops, secure the dressing with a bandage or adhesive tape. This helps keep the wound protected and prevents further blood loss.
- Monitor for Continued Bleeding: Keep an eye on the wound to ensure the bleeding does not restart. If it does, reapply pressure and seek medical assistance.
- Seek Medical Attention: Even if the bleeding is controlled, it’s important to have the wound evaluated by a healthcare professional. This ensures proper cleaning, dressing, and assessment for deeper injuries.
Importance of Hygiene and Infection Prevention
Maintaining hygiene is critical when treating venous bleeding to prevent infections, which can complicate the healing process. Here are key hygiene practices to follow:- Use Sterile Materials: Always use clean or sterile gauze, bandages, or cloths to cover the wound. This minimizes the risk of introducing bacteria into the injury.
- Wash Hands Thoroughly: Before and after providing first aid, wash your hands with soap and water or use hand sanitizer if soap is unavailable.
- Avoid Touching the Wound: Refrain from directly touching the wound with your hands, even if they are clean. Use gloves if available.
- Clean the Surrounding Area: If possible, gently clean the skin around the wound with soap and water to remove dirt or debris. Avoid letting water or cleaning agents enter the wound itself.
- Change Dressings Regularly: Replace the dressing daily or whenever it becomes wet or dirty. This helps keep the wound clean and reduces the risk of infection.
Monitoring for Complications
Even after controlling venous bleeding, it’s essential to monitor the injured person for potential complications. Here are some signs to watch for:- Signs of Infection: Look for redness, swelling, warmth, or pus around the wound. These are common indicators of an infection that requires medical attention.
- Persistent Bleeding: If the bleeding resumes or does not stop despite applying pressure, seek immediate medical help.
- Swelling or Bruising: While some swelling is normal, excessive swelling or discoloration could indicate deeper tissue damage or a blood clot.
- Lightheadedness or Weakness: If the injured person feels faint, weak, or dizzy, it may be a sign of significant blood loss or shock. Lay them down and elevate their legs while waiting for medical assistance.
- Delayed Healing: If the wound does not show signs of healing within a few days, consult a healthcare provider to rule out complications.
How to Identify the Type of Bleeding in an Emergency
Practical Tips for Quick Identification
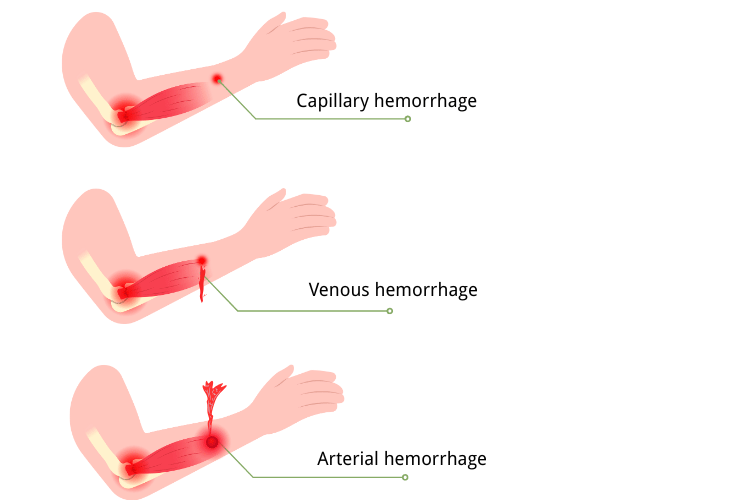
In an emergency, identifying the type of bleeding is crucial for determining the appropriate first aid response. The three main types of bleeding—arterial, venous, and capillary—each have distinct characteristics that can help you quickly assess the situation. Here are practical tips to identify the type of bleeding:- Observe the Color of the Blood:
- Bright Red Blood: Indicates arterial bleeding due to the high oxygen content in the blood.
- Dark Red or Maroon Blood: Suggests venous bleeding, as the blood is deoxygenated.
- Bright Red with Minimal Flow: Points to capillary bleeding, which is usually superficial and less severe.
- Check the Flow Pattern:
- Pulsating or Spurting Blood: Arterial bleeding is characterized by spurts of blood that sync with the heartbeat, making it harder to control.
- Steady, Continuous Flow: Venous bleeding flows at a consistent rate without spurting.
- Slow Oozing: Capillary bleeding typically oozes slowly and is easier to manage.
- Assess the Pressure and Severity:
- High Pressure and Rapid Loss: Arterial bleeding is under high pressure and can lead to significant blood loss quickly.
- Moderate Pressure: Venous bleeding occurs under lower pressure but can still result in substantial blood loss if untreated.
- Low Pressure: Capillary bleeding is low-pressure and usually stops on its own with minimal intervention.
- Look for Associated Symptoms:
- Shock Symptoms: Arterial bleeding often leads to symptoms like pale skin, rapid breathing, and fainting due to rapid blood loss.
- Swelling or Bruising: Venous bleeding may cause localized swelling or pooling of blood near the wound.
- Minimal Symptoms: Capillary bleeding rarely causes systemic symptoms unless the wound becomes infected.
Real-Life Examples or Scenarios
Understanding how to identify bleeding types in real-life situations can help you respond effectively. Here are some common scenarios:- Car Accident with Deep Cuts: A person involved in a car accident has a deep wound on their leg. The blood is bright red and spurting in rhythm with their heartbeat. This is a clear sign of arterial bleeding, requiring immediate pressure and possibly a tourniquet to control the blood loss.
- Kitchen Injury with a Knife: While chopping vegetables, someone accidentally cuts their hand. The blood is dark red and flows steadily without spurting. This indicates venous bleeding, which can be managed with direct pressure and elevation of the hand.
- Child Falls and Scrapes Their Knee: A child falls while playing and scrapes their knee. The wound oozes bright red blood slowly and stops after a few minutes. This is capillary bleeding, which can be cleaned and covered with a bandage to prevent infection.
- Industrial Accident with Severe Trauma: In a workplace accident, a worker suffers a severe injury to their arm from heavy machinery. The blood spurts forcefully and the person shows signs of shock, such as pale skin and dizziness. This is arterial bleeding, requiring immediate first aid and emergency medical attention.
- Sports Injury with Swelling: During a soccer game, a player sustains a deep cut on their shin. The blood is dark red and pooling around the wound, accompanied by swelling. This is venous bleeding, and applying pressure and elevating the leg can help control it.
Long-Term Complications of Untreated Bleeding
Risks of Untreated Bleeding: Shock, Infection, and Organ Damage
Failing to address bleeding promptly can lead to severe and sometimes irreversible complications. The risks vary depending on the type and severity of the bleeding, but the following are the most common long-term consequences:- Hypovolemic Shock: One of the most immediate and life-threatening risks of untreated bleeding is hypovolemic shock. This condition occurs when the body loses a significant amount of blood, reducing the volume available to maintain adequate circulation and oxygen delivery to vital organs. Symptoms include pale skin, rapid breathing, confusion, and fainting. If left untreated, hypovolemic shock can lead to organ failure and death.
- Infections: Open wounds that are not properly cleaned and treated can become breeding grounds for bacteria, leading to infections. Localized infections, such as cellulitis, can cause redness, swelling, and pain around the wound. More severe cases may result in systemic infections like septicemia, where bacteria enter the bloodstream, potentially causing widespread inflammation and organ damage.
- Organ Damage: Prolonged blood loss can deprive critical organs, such as the brain, heart, and kidneys, of the oxygen and nutrients they need to function. This can result in permanent damage or failure of these organs. For example, reduced blood flow to the brain can cause cognitive impairments, while kidney damage may lead to chronic kidney disease.
- Tissue Death (Necrosis): In cases of severe arterial bleeding, the lack of oxygenated blood reaching tissues can result in necrosis, or tissue death. This is particularly common in extremities, where prolonged blood loss may necessitate amputation to prevent the spread of infection or further complications.
- Chronic Swelling and Venous Insufficiency: Untreated venous bleeding can lead to chronic venous insufficiency, a condition where blood flow back to the heart is impaired. This can cause long-term swelling, pain, and the development of venous ulcers, which are difficult to heal and prone to infection.
- Blood Clots and Embolism: Prolonged venous bleeding or damage can increase the risk of blood clots forming in the veins, a condition known as deep vein thrombosis (DVT). If a clot dislodges and travels to the lungs, it can cause a life-threatening pulmonary embolism, leading to difficulty breathing and chest pain.
Preventative Measures to Avoid Complications
Preventing long-term complications from bleeding requires prompt and effective first aid, as well as ongoing care to ensure proper healing. Here are some key preventative measures:- Immediate First Aid:
- Apply direct pressure to the wound to control bleeding.
- Elevate the injured area above the heart to reduce blood flow.
- Use a tourniquet if necessary and trained to do so, especially for severe arterial bleeding.
- Proper Wound Cleaning:
- Clean the wound with sterile water or saline to remove dirt and debris.
- Avoid using harsh chemicals like hydrogen peroxide, which can damage healthy tissue.
- Use of Sterile Dressings:
- Cover the wound with a sterile dressing or bandage to protect it from bacteria.
- Change the dressing regularly to maintain cleanliness and prevent infection.
- Monitor for Signs of Infection:
- Watch for redness, swelling, warmth, or pus around the wound.
- Seek medical attention if these symptoms appear, as they may indicate an infection.
- Seek Medical Attention for Severe Bleeding:
- Always consult a healthcare professional for deep or large wounds, as they may require stitches, surgical intervention, or antibiotics.
- Follow-Up Care:
- Attend follow-up appointments to ensure the wound is healing properly.
- Adhere to prescribed treatments, such as antibiotics or wound care instructions, to prevent complications.
- Prevent Blood Clots:
- For venous injuries, encourage gentle movement of the affected limb to promote circulation and prevent clot formation.
- In some cases, doctors may recommend blood-thinning medications to reduce the risk of clots.
Prevention and Preparedness
Importance of First Aid Training
First aid training is a critical skill that equips individuals with the knowledge and confidence to respond effectively during emergencies. Whether it’s a minor injury or a life-threatening situation, having the ability to provide immediate care can make a significant difference in outcomes. For example, knowing how to control bleeding, perform CPR, or treat burns can save lives and prevent complications before professional medical help arrives. Beyond physical care, first aid training also helps individuals remain calm and composed under pressure, enabling them to make quick, informed decisions. Moreover, first aid training fosters a sense of responsibility and preparedness within communities. When more people are trained, the likelihood of timely intervention during emergencies increases, creating a safer environment for everyone. This is particularly important in workplaces, schools, and public spaces where accidents are more likely to occur. By investing in first aid education, individuals not only protect themselves and their loved ones but also contribute to the well-being of their communities.Recommended Courses and Certifications
To ensure you are well-prepared for emergencies, enrolling in a certified first aid course is highly recommended. These courses provide hands-on training and cover a wide range of topics, from basic wound care to advanced life-saving techniques. Here are some popular courses and certifications to consider:- Basic First Aid Certification: This course covers essential skills such as treating cuts, burns, and fractures, as well as managing choking and minor medical emergencies. It’s ideal for beginners and those looking to build a strong foundation in first aid.
- CPR and AED Training: Cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) training are crucial for responding to cardiac emergencies. These courses teach participants how to perform chest compressions, use an AED, and provide rescue breaths effectively.
- Advanced First Aid: Designed for individuals in high-risk professions or remote areas, advanced first aid courses delve deeper into topics like managing severe trauma, administering oxygen, and stabilizing patients until professional help arrives.
- Wilderness First Aid: This specialized course is tailored for outdoor enthusiasts and adventurers. It focuses on handling emergencies in remote locations where access to medical facilities may be delayed.
- Pediatric First Aid: For parents, caregivers, and teachers, pediatric first aid courses provide training on managing injuries and illnesses specific to infants and children, such as choking, allergic reactions, and fever management.
- Online and Blended Learning Options: Many organizations, such as the American Red Cross and St. John Ambulance, offer online or hybrid courses that combine virtual learning with in-person practice. These flexible options make it easier to fit training into busy schedules.
Building a First Aid Kit for Emergencies
A well-stocked first aid kit is an essential component of emergency preparedness. Having the right supplies on hand can help you respond quickly and effectively to injuries or medical situations. Here’s a guide to building a comprehensive first aid kit:Basic Supplies:
- Adhesive Bandages: Include a variety of sizes for minor cuts and scrapes.
- Sterile Gauze Pads and Rolls: Useful for covering larger wounds and controlling bleeding.
- Medical Tape: Secures dressings in place without causing irritation.
- Antiseptic Wipes and Solutions: Clean wounds to prevent infection.
- Antibiotic Ointment: Promotes healing and reduces the risk of infection.
- Scissors and Tweezers: For cutting bandages and removing debris from wounds.
- Disposable Gloves: Protect both the caregiver and the injured person from contamination.
Advanced Items:
- CPR Mask or Shield: Ensures safe and hygienic rescue breathing during CPR.
- Tourniquet: Essential for controlling severe arterial bleeding.
- Instant Cold Packs: Reduces swelling and provides pain relief for sprains or bruises.
- Elastic Bandages: Useful for wrapping sprains or securing dressings.
- Thermometer: Monitors body temperature during illness or fever.
- Emergency Blanket: Helps retain body heat in cases of shock or hypothermia.
Medications:
- Pain Relievers: Include over-the-counter options like ibuprofen or acetaminophen.
- Antihistamines: Useful for allergic reactions or insect bites.
- Hydrocortisone Cream: Relieves itching and inflammation.
- Oral Rehydration Salts: Prevent dehydration during heat exhaustion or illness.
Additional Items:
- First Aid Manual: Provides step-by-step instructions for handling various emergencies.
- Flashlight and Extra Batteries: Ensures visibility in low-light situations.
- Emergency Contact Information: Include phone numbers for local emergency services, family members, and healthcare providers.
Tips for Maintenance:
- Regularly check the kit to ensure all items are in good condition and within their expiration dates.
- Replace used or expired supplies promptly.
- Customize the kit based on specific needs, such as including personal medications or items for children and pets.
Conclusion
In conclusion, understanding the different types of bleeding and the importance of quick identification and treatment is vital for effective emergency response. By learning first aid and staying prepared, you can make a significant difference in critical situations and potentially save lives.














 Login with Google
Login with Google Login with Facebook
Login with Facebook