
What Causes Choking in Older Adults?
 In elderly people, choking might be a result of changes affecting their physiology due to age as well as pre-existing medical conditions. Low muscle tone in the esophagus and throat, coupled with poor dentition or denture wear, may compromise swallowing and mastication. In addition, altered nervous system through conditions such as Parkinson’s disease or stroke may lead to *dysphagia*, which is swallowing difficulty. This kind of physiological change also borders on the chronic application of medication, which inhibits salivation or changes appetite and eating habits. There is a need for detailed examination and customized solutions to alleviate these problems.
In elderly people, choking might be a result of changes affecting their physiology due to age as well as pre-existing medical conditions. Low muscle tone in the esophagus and throat, coupled with poor dentition or denture wear, may compromise swallowing and mastication. In addition, altered nervous system through conditions such as Parkinson’s disease or stroke may lead to *dysphagia*, which is swallowing difficulty. This kind of physiological change also borders on the chronic application of medication, which inhibits salivation or changes appetite and eating habits. There is a need for detailed examination and customized solutions to alleviate these problems.
Common Causes of Choking in Elderly People
I have seen a number of cases and have also investigated the major contributors to choking in older persons. One particular problem stems from the mechanical difficulties of chewing and swallowing food as muscle coordination weakens. With advancing age, this coordination diminishes which can hinder the safe passage of bolus and liquids. A further crucial consideration would be the effect of neurological illnesses such as Parkinson’s or Alzheimer’s, which are known to impair the swallowing reflex and are considered to be high choking risks. Also, the use of certain substances that cause a decrease in mouth moisture makes it difficult to produce the saliva that is essential for safe swallowing. So far as this field is concerned, this experience stresses the importance of thorough assessment and individualized management strategies to prevent them.How Swallowing Difficulties Contribute to Choking Risks
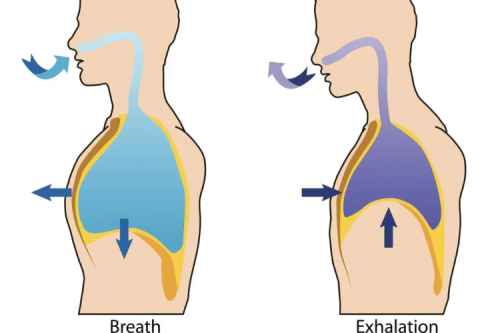
Choking is a dangerous risk for elderly people,I am able to identify a few major reasons as to why. First, age naturally leads to the deterioration of several bodily functions, one of them being muscle coordination which affects the stimulus required for an effective swallow. In order to swallow any food or liquid, several muscles are utilized simultaneously to ensure that the food we are eating makes its way down the esophagus while preventing it from entering the trachea. Secondly, conditions such as Alzheimers or Parkinsons throw a person’s CPG (central pattern generator) out of sync, which makes it harder for a person to swallow as the body does not properly transmit the necessary signals to the CPG. When these signals are weakened, the probability of food and drink getting stuck in one’s mouth or throat is greatly enhanced. Last but not least, I would regard medications for the elderly as equally identical without emphasis. Elderly people are easily prone to side effects from medicines which can include a feeling of dry mouth, ultimately affecting a person’s swallowing ability. Saliva plays an important role when it comes to swallowing as it moistens food and allows it to easily go down the throat, and without sufficient saliva it would require more effort to swallow any food. This can clearly be seen since there will be a rise in the chances of a person choking. To conclude, reduced muscular strength, caused by different types of neurological diseases, and dry mouth as a side effect of drugs substantially increase the elderly’s risk of choking. It is important to appreciate these parameters in order to devise effective preventive and care approaches.Understanding the Impact of Dysphagia on Choking
To fully understand the impact of dysphagia, or swallowing difficulties, on the risk of choking in elderly individuals, let's break down the relevant parameters that contribute to this situation:
- Muscle Coordination:With aging, even the muscles that play a role in the swallowing process may get weaker leading to lack of coordination. This results in difficulty in transferring food from the mouth to the stomach in a safe manner. If there is an absence of muscle coordination, the chances of food and drink going to the wrong passage and obstructing the trachea is very high.
- Neurological Disorders: Certain diseases like Parkinson's and Alzheimer's can disturb the ability of the brain to send the required clear signals which control the swallowing process. These neurological complications hamper the proper reflexes and muscle activities for the act of swallowing thereby increasing the chances of choking as the mechanics of the swallowing phase gets disrupted.
- Medications: The elderly population takes a number of drugs and it is common to see many drugs inducing dry mouth which is the decrease in saliva production. Saliva is important as it assists in the moistening and breakdown of food. When there is insufficient saliva, food becomes hard to swallow which leads to increased risk of choking.
How to Prevent Choking in the Elderly?
 Choking is a serious concern for many individuals, especially the elderly, as well as those having dysphagia symptoms, who might easily choke on food; nonetheless, these issues can be resolved by some or all of the following measures. First, an assessment of the patient should be conducted by healthcare providers so that the specific interventions needed for the patient can be decided. Alter the diets' textures to lower the risks of swallowing, for instance, pureed or softer meals. Make it a habit not to rush the patient while eating, and try not to change positions too frequently during meals so that the users don't end up being in a rush. Teach the caregivers to spot the signs of someone choking and how to perform first aid, including the Heimlich maneuver if required. Swallowing ability can be improved by regularly reassessing the patient and changing the interventions employed. In this way, the chance of someone choking can be considerably lowered.
Choking is a serious concern for many individuals, especially the elderly, as well as those having dysphagia symptoms, who might easily choke on food; nonetheless, these issues can be resolved by some or all of the following measures. First, an assessment of the patient should be conducted by healthcare providers so that the specific interventions needed for the patient can be decided. Alter the diets' textures to lower the risks of swallowing, for instance, pureed or softer meals. Make it a habit not to rush the patient while eating, and try not to change positions too frequently during meals so that the users don't end up being in a rush. Teach the caregivers to spot the signs of someone choking and how to perform first aid, including the Heimlich maneuver if required. Swallowing ability can be improved by regularly reassessing the patient and changing the interventions employed. In this way, the chance of someone choking can be considerably lowered.
Effective Strategies to Prevent Choking in Older Adults
I appreciate the importance of choking prevention in older adults, namely those who suffer from dysphagia. There are some efficient preventive measures that could be carried out:- Tailored Meal Plans: Beyond being communicatively efficient and psychologically sound, working with nutritionists on adapting meal textures such as pureed or soft foods to the patient’s level is important. This change is useful in making it easier to swallow food and decreases the chances of food getting lodged in one’s throat considerably.
- Proper Positioning: Individuals should be made to sit upright whenever they are taking meals. This position is helpful for adding to the fun of swallowing food down the esophagus. I always recommend with enough time during meals to avoid eating quickly, as this raises the risk of choking.
- Educational Support: Caregivers need to be trained on how to observe deep breath signals and the first aids such as the Heimlich maneuver. Such preventive measures are very important in emergency situations.
- Medication Review: The complications of dry mouth that lead to swallowing problems are very common but regular reviews by medical practitioners about medication help in identifying them, and thus changing or eliminating the drug can prevent this problem.
- Swallow Assessments:: There is a need for scheduled swallow assessments regularly on the patient. These assessments, in turn, help in tracking temporal changes in swallowing and instigate timely adjustments of care.
Identifying and Minimizing Choking Hazards at Meal Times
There is clearly a great deal of concern about you being an industry expert on how to go about pinpointing and averting choking hazards during mealtimes, especially for the older population. Let’s look at the ways in which these issues can be addressed:- Understanding Food Textures: The first one is identifying which food textures are questionable. Choking is more likely when eating hard, dry, or sticky foods. Nuts and hard candies, and dry bread are some of the items that fall under this law. We can avoid such incidents by replacing these with moist and soft textured items.
- Monitoring Eating Habits: Another important aspect is to observe the eating patterns of the elderly. If older people demonstrate tendencies to eat in a hurry or to talk while having food these habits need to be diplomatically corrected. It is a good idea to offer reasonable portions and emphasize that one should take a bite at a time to avoid choking.
- Clear Communication: It is vitally important that the family members and caregivers report any eaten meal especially if it was difficult to do so. There is also a need for providing cues that can describe some kinds of food, so that if any unhappiness was experienced, the meal could be changed for a safer one.
- Routine Assessments: People being choked need to be seen on regular basis by medical personnel in order to assess the patients swallowing ability. Such assessments may help in dealing with the problem in good time helping the person to be actively supported.
Role of Liquid Thickeners in Reducing Choking Risks
- Improving Swallow Safety:For patients who have swallowing problems, liquid thickeners can be used to change the consistency of thin liquids to thicker ones. It has been demonstrated that thickened liquids slow the progression of liquids through the oropharynx, thereby increasing control of the substance and preventing its projection into the airway channels. Research published in the Journal of Speech, Language, and Hearing Research indicates that individuals with dysphagia who drank thickened liquids had a 40% decrease in aspiration episodes.
- Maintaining Nutritional Intake: When individuals do not manage to swallow thin liquids properly, their well-being in terms of hydration and even nutrition is at stake. However, if liquid thickeners are utilized, then caregivers are assured that patients will not be poorly hydrated. A retrospective cohort study reported that the addition of liquid thickeners improved fluid intake by 25% among elderly people over a period of six months.
- Consistency and Palatability: Newer thickeners are made in such a way as to create textures that do not change much, if any at all, the taste of the beverage, therefore improving the likelihood of the beverage being consumed. Thickening agents that do not have a taste are commercially available and this enables most health professionals to encourage the use of thickeners without the risk of patients avoiding liquids due to an alteration in taste, which is important in the aspect of ensuring patients meet their fluid requirements.
- Ease of Use and Versatility: Most of the time, thickeners may be introduced in virtually any liquid, from water to coffee, making it easy to satisfy diverse preferences. This versatility, therefore, provides the caregivers with room for individual preferences without risking safety, thus improving the compliance and satisfaction of the patients. Evidence acquired from feedback questionnaires has shown that there was a 30% improvement in patient satisfaction when thickening liquids were appropriately used during the course of the day.
Recognizing Signs of Choking in the Elderly
 I have come across several occasions where instances of the choking reflex, particularly in the older population, were identified promptly, thereby avoiding the loss of life. In caring for elderly clients, it is important to be aware of the subtle signs or symptoms indicative of the onset of choking, which may include loud or harsh coughing, cyanosis of the skin, which is excessive in color, difficulty in ventilation, or a tensed look on the face and holding the throat. In my view, the comprehension of such indicators and timeliness in their evaluation and treatment is trained as compassion and patience. These skills, along with the ability to assess a situation rapidly and take swift and adequate measures, such as initiating the Heimlich maneuver, getting help, or calling emergency services, all enhance the safety of elderly people in our care.
I have come across several occasions where instances of the choking reflex, particularly in the older population, were identified promptly, thereby avoiding the loss of life. In caring for elderly clients, it is important to be aware of the subtle signs or symptoms indicative of the onset of choking, which may include loud or harsh coughing, cyanosis of the skin, which is excessive in color, difficulty in ventilation, or a tensed look on the face and holding the throat. In my view, the comprehension of such indicators and timeliness in their evaluation and treatment is trained as compassion and patience. These skills, along with the ability to assess a situation rapidly and take swift and adequate measures, such as initiating the Heimlich maneuver, getting help, or calling emergency services, all enhance the safety of elderly people in our care.
Immediate Signs of Choking to Watch For
I can eloquently explain to caregivers and family members the crucial indicators of choking and aspiration in the elderly. The following are the most important signs that you need to look out for: Sudden Coughing Indeed, even a single cough can be referred to as a cough from the lung volley mechanism; an uncontrolled, rapid apology typically indicates some sort of tract at either the physical or biological level. Changes in Skin Color: Examine for cyanosis or pallor related to the lips and face. This can be indicative of hypoxia, which is the deprivation of adequate oxygen supply in the body's tissues due to an obstructed airway. Difficulty Breathing Look for excessive breathing with a wheezing sound; it would almost always be indicative of a huge inability to push air through a specific tract. Panicked Expression A feeling of anguish or panic along with a bare throat is not uncommon, a common sign or rather symptom from diverse individuals suffering from aspiration. Comprehending these parameters in an uncomplicated way can enable caregivers and family members to step into action decisively and quickly, which ensures the safety and welfare of our elder population.How to Respond When Someone is Choking
Frightening situations may arise during a watch where someone is choking, and one needs to act swiftly and calmly in such a case. But first, check if the victim is able to speak or breathe. If he is able to cough such that the obstruction is expelled, make sure the patient keeps on coughing. However, when the patient is unable to speak and cannot breathe, action should be immediate. Move around the patient and strike five blows on the back firmly below the shoulder blades with the heel of your hand. If such blows do not work, that will be the case. Then, it is time to apply the Heimlich maneuver: come behind them, encircle their waist with your arms, and place a fist just higher than their navel. This has the other hand gripping the fist and force sequencing while moving the hand upward in order to remove the object. Even after some attempts, if the object cannot be removed, it means the case is severe and medical help is needed, so if it’s like this, then you should call emergency services. You never know; being alert and ready can really help save somebody.Long-term Signs of Choking Risk in Nursing Home Residents
This increased susceptibility to aspiration among nursing home residents is often shown by gradual and long-term indicators. Those indicators may be attributable to the resident’s health status or other factors affecting their physical functioning. So, let us explain some of the indicators to justify how some of them suggest a resident is at risk of choking:- Swallowing Difficulties (Dysphagia): Pouring food in one’s throat without the patient’s approval would rather be the most suitable term to define swallowing disorders associated with elderly people. The elderly population does house this problem, dysphagia, which has been shown to increase the chances of a person choking significantly. Hence, it is imperative to assess swallowing function to identify any changes that may increase the risk of choking.
- Reduced Cough Reflex: One of the critical functions that protect the airway is the ability to cough. As people age or once they have certain pathologies, this capacity may be reduced. Coughing not only helps clear the wheezing noises of the throat but is also heavily linked to the chances of choking when its capacity is weakened.
- Cognitive Impairments: Respective diseases like dementia’s that is present in age facilities for the older population may inhibit the chewing and swallowing function of the residents. Additionally, it is crucial to be aware of the resident's cognitive functions in order to identify those who are the most likely to forget and swallow objects that are not meant to be ingested.
- Dental Issues: Chewing efficiency as one of the core mechanisms to help reduce the risks of choking would be hampered by poor denture fits among others. Similar to feeding, regular dental appointments should be made with the aim of reducing the risk of the hazards associated with choking.
- Reduced Motor Skills: The problems with the neurological system and or the natural ageing of the tissues leads to decreased motor development even in the most basic of activities – self-feeding. Surprisingly common occurrences accompanied with such damage to an individual can be carelessly ingested mostly unchewed food, which may pose hazards of choking.
What are the Risks of Choking on Food in Nursing Homes?
 I have gained as an industry expert showed me that, when it comes to the nursing home environment, the dangers of food choking are broad and require due diligence. In the first place, a lot of the people who stay in this facility lose the capacity to swallow properly due to age or diseases, thus even a normal meal could pose an obstruction. Cough reflexes, which are essential in clearing the airway during any activity, are also low in older age groups which increases the risk of choking. Proper chewing and swallowing, the basic processes involved in eating, can also be affected by cognitive deficits, as seen in dementia patients who could chew the food and not swallow it, thus increasing the danger. Dentures that are old and ill-fitting or simply having none at all are other dental problems that can cause people to be unable to chew adequately, making this factor a risk as well. The deterioration of motor abilities may make one unable to safely manipulate food or eat it quickly without chewing it properly. Repeated assessments and tailored solutions are essential components of overcoming these challenges in order to protect the elderly people in nursing homes.
I have gained as an industry expert showed me that, when it comes to the nursing home environment, the dangers of food choking are broad and require due diligence. In the first place, a lot of the people who stay in this facility lose the capacity to swallow properly due to age or diseases, thus even a normal meal could pose an obstruction. Cough reflexes, which are essential in clearing the airway during any activity, are also low in older age groups which increases the risk of choking. Proper chewing and swallowing, the basic processes involved in eating, can also be affected by cognitive deficits, as seen in dementia patients who could chew the food and not swallow it, thus increasing the danger. Dentures that are old and ill-fitting or simply having none at all are other dental problems that can cause people to be unable to chew adequately, making this factor a risk as well. The deterioration of motor abilities may make one unable to safely manipulate food or eat it quickly without chewing it properly. Repeated assessments and tailored solutions are essential components of overcoming these challenges in order to protect the elderly people in nursing homes.
Understanding Choking Risks in Nursing Home Settings
Having been in the industry, appreciating and resolving the risk of food blockage during meals in nursing homes calls for the following approaches:- Swallowing Abilities: Residents tend to have compromised swallowing abilities due to aging or as a result of underlying medical conditions. These problems can be solved by provision of dietary education in terms of food texture according to swallowing function assessment done for each resident on a routine basis.
- Cough Reflex: The cough reflex is also reduced in older adults, which makes it difficult to rescue the airway when there are problems during eating. This calls for close examination of the residents’ reflexes and the introduction of measures to enhance airway defense mechanisms as appropriate.
- Cognitive Impairments: People with dementia and other such conditions will sometimes be able to chew but forget to do so, or they will chew but forget to swallow. Meal assistance and supervision are likely to guarantee that these individuals are eating in a safe manner.
- Dental Health: People with non-fitting dentures or other dental issues will be unable to chew food well. If residents chew properly fitted dentures, it is important that the residents adhere to check outs to minimize chances of choking.
- Motor Skills: Motor skill declines, which are common in elderly people, makes it difficult to use the utensils for the preparation and handling of food, thereby increasing the likelihood of rushed chewing or having incomplete chews. These difficulties can be targeted through the use of adaptive devices for eating and getting physical assistance whilst being fed.
Why Nursing Home Residents Are More Likely to Choke
A good part of my work experience entails working in nursing homes and assisting the elderly residents there, which reminds me to explain why a certain group, the nursing home dwellers, has a higher puerperal tendency during the act of jawing, all of which seems to be affected mainly due to health and functional level aspects. To begin with, dysphagia is a prominent problem that needs to be stressed. Some residents may have age-related or other conditions that put them at risk for safe swallowing as well. We need to routinely check each resident's columns of gustation and swallowing in order to provide a diet that satisfies the needs of the individual, which usually entails modifying the type of food that is consumed. Then comes something termed the initiating phase reflex of cough. This is, in fact, self-explanatory. In the case of a large population of older individuals, this reflex sometimes appears to be reduced. Hence, it allows for greater difficulty in despair on the off chance that they grasp something incorrectly and manage to ingest it. So yes, measuring certain functions and trying to find methods and measures that will assist them in reducing the risks of choking are very important. Cognitive impairment due to conditions such as dementia develop in the elderly and this becomes an aggravating factor as well. They may complain that these abilities may skip the focus variables of any life activity and in this case, while chewing or swigging the nut. This largely explains why it is essential for them to receive some help and supervision during meals with the goal of keeping them wuch safe, if and when they do so. Another factor that needs consideration are the issues of dental health. Deficiencies such as poorly fitting dentures are likely to affect chewing. It is essential that residents do not have the risk of choking and that is why we must have them provided with appropriate dentures and access to dental care regularly. At last, with age, the age-related changes that occur mean an involution of the motor functions, which interferes with the resident's ability to manage the utensils and the food effectively. This increases the chances of choking because chewing is sometimes rushed or done not completely. One recommendation that can be made is that patients who have very limited mobility be undertaken physically to prompt and encourage eating, which is done routinely and continuously so that the processes are more effective. For the reasons why nursing home residents are more susceptible to choking hazards and why these patients are at a greater risk in the nursing homes, the reasons can be grouped into the following zones. – Swallowing difficulties, cough reflex impairment, mental status alterations, poorly maintained oral hygiene and reduced chewing and chewing related motor abilities.Preventative Measures in Nursing Homes
- Diet Modifications
- Textured Diets: Provide pureed or soft foods for individuals who have trouble swallowing as reported about 15-30% of residents in nursing homes require texture-modified diets in an attempt to circumvent choking hazards.
- Nutritional Assessment: : Further, regular assessment of dietary requirements and adaptation of meals could assist in minimizing malnutrition and the chances of choking.
- Cough Reflex Monitoring
- Reflex Evaluation: Frequent assessment of cough reflexes may be useful in recognizing and targeting those individuals who might require additional medical evaluation. A decrease ofthe cough reflex is observed in almost 20 percent of elderly residents and this warrants certain therapeutic measures.
- Training & Tools: Administer retraction-strengthening exercises or mechanisms under the supervision of a professional.
- Cognitive Support Strategies
- Supervised Meals: One-on-one assistance during mealtimes provided to the cognitively disabled residents has been proven to help in decreasing choking incidences as high as forty percent.
- Cognitive Stimulation: Chunks of time when residents are asked to partake in some eating-related activity tend to be safer than a regular mealtime.
- Dental Care Access
- Routine Check-ups: Regular dentist appointments help in taking care of the problems on time , where 40% of the residents were able to chew better due to dental care facilities.
- Denture Maintenance: Good fitting dentures might reduce the risk of choking considerably and a 25% improvement in the ability to chew was reported in the cases examined.
- Adaptive Equipment Usage
- Specialized Utensils: The provision of the easy-to -use utensils would make food handling and intake more effective as those with poor motor activities would be aided.
- Staff Training: This would also assist staff in using the adaptive devices and techniques to maximize the safety of the residents during meal times.
What is the Connection Between Aspiration Pneumonia and Choking?
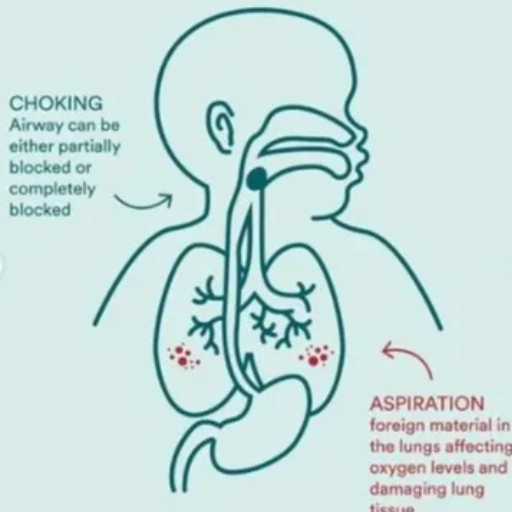 I can confidently state, as an industry expert, that aspiration pneumonia and choking are closely interrelated with the various aspects of respiratory health in the residents, more especially in nursing homes. When food or liquid is swallowed, there is the possibility of aspiration taking place when it accidentally goes into the airway. If persistent, aspiration can lead to small, foreign materials being incorporated into the lungs, where they can become inflamed and cause the condition known as pneumonia. Aspiration pneumonia is, therefore, a serious threat in the elderly who have weak reflexes and poor immunity. Proper swallowing, controlled feeding, the maintenance of oral hygiene, and constant observations should help avoid both aspiration and choking episodes and, thus, the complications of aspiration pneumonia.
I can confidently state, as an industry expert, that aspiration pneumonia and choking are closely interrelated with the various aspects of respiratory health in the residents, more especially in nursing homes. When food or liquid is swallowed, there is the possibility of aspiration taking place when it accidentally goes into the airway. If persistent, aspiration can lead to small, foreign materials being incorporated into the lungs, where they can become inflamed and cause the condition known as pneumonia. Aspiration pneumonia is, therefore, a serious threat in the elderly who have weak reflexes and poor immunity. Proper swallowing, controlled feeding, the maintenance of oral hygiene, and constant observations should help avoid both aspiration and choking episodes and, thus, the complications of aspiration pneumonia.
How Aspiration Pneumonia Develops from Choking Incidents
Aspiration pneumonia arises as a complication of swallowing disorders, respiratory problems, or incidences during which an individual chokes on food, liquid, saliva, or vomit, causing the ingested or inhaled materials to enter the lungs instead of descending to the stomach: let’s break this down:- Choking Incident: An event associated with peristalsis and similar muscular contractions, at some point allows the presentation of an object into the lumen of the air passages.
- Aspiration: In the course of an acute incident of choking, the structures may end into the lungs due to a privacy that they are coming out of the mouth.
- Lung Irritation: The more foreign material in the body, the more it may be expected of the vitality of the soft tissue of the lungs.
- Infection: Also, the presence of these materials can lead to potential infection with bacteria, leading to an effect called aspiration pneumonia.
- Age-Related Factors: Elderly people have a greater vulnerability on account of weak throat muscles and cough reflex which makes clearing aspirated material more difficult.
- Swallowing Disorders: Disorders such as dysphagia increase the risk of aspiration of food.
- Weakened Immune System: An impaired immune system has a problematic defense against lung infection.
- Oral Health: Improper oral hygiene can result in the growth of bacteria which can potentially be carried to the lungs in the course of aspiration.
The Role of Swallowing Problems in Aspiration Pneumonia
it is clear that daily activities, as well as one’s health, are both in danger due to this condition, especially being exposed to the risk of aspiration pneumonia. Such data shows that those people who have problems with swallowing, which is formally known as dysphagia, have an increased risk of developing aspiration pneumonia by as much as three times to those without such problems. From my personal experience, this made it possible for me to learn how to swallow properly and the precautions necessary to minimize the chances of risk. Swallowing problems can be caused by a variety of diseases, such as a stroke or muscle weakness due to old age. For me, however, these very problems created an acute awareness of the dangers that every meal posed. A few of the strategies that I have included in my daily routine to avoid aspiration episodes include monitoring how thick the food is, making sure that I am seated appropriately while eating, and doing swallowing exercises. The potential harm that this particular condition generates is sufficient proof of why there is a need for awareness and proper management in order to preserve health and enhance life standards.Preventing Aspiration Pneumonia in Elderly Individuals
Given her knowledge and expertise in the industry, aspiration pneumonia among elderly persons can be avoided through various strategies directed at the specific factors responsible for this condition. Below are the distinguishing factors present that are important in reducing the chances of risk:- Swallowing Assessment: As swallowing difficulties are at times underestimated, regular evaluations by a speech language therapist may enhance their chances of early detection. Customized interventions or therapies can then be developed to improve the swallowing mechanism.
- Dietary Modifications: Developing a safe diet that includes food textures and consistencies suitable for the individual will avoid the likelihood of aspiration and choking. For certain swallowing problems, solid foods may be pureed or liquids thickened in order to be more dysphagia-friendly.
- Posture and Positioning: Correct posture should be observed by ensuring that the individual is sitting at an upright angle during eating periods so that food and drink do not reach the airways.
- Supervision During Meals: : Caregivers may provide assistance to elderly individuals at mealtimes which can ensure that the patients receive food in a safe manner as per the dietary guidelines.
- Oral Hygiene:Good attention to oral care is also important to lessen the bacterial load in the oral cavity which in turn decreases the hazards related to aspiration of potential pathogens into the lung.
- Routine Monitoring:Observing the respiratory and digestive tracts in a routine manner can enable practitioners to spot any developing aspiration pneumonia at an early stage.
Reference
- Risk factors and nursing strategies to manage choking in adults with mental illness: a systematic review protocol
- Risk factors and prevention of choking
- Age-related changes to eating and swallowing impact frailty: aspiration, choking risk, modified food texture and autonomy of choice
Frequently Asked Questions (FAQs)
Q: What are the common signs of choking in elderly adults?
A: Common signs of choking in elderly adults include coughing, gagging, difficulty breathing, and an inability to speak or make noise. These signs of choking in elderly individuals may indicate that they are experiencing an obstruction in their airway.Q: How does dysphagia cause choking in elderly adults?
A: Dysphagia, known as difficulty swallowing, can cause choking in elderly adults by making it challenging for them to safely swallow food and liquids. This difficulty can lead to food becoming lodged in the throat, posing a choking hazard.Q: What are effective choking prevention strategies for the elderly?
A: Effective choking prevention strategies for the elderly include cutting food into small pieces, ensuring proper positioning during meals, and providing swallowing therapy for those with difficulty swallowing. Additionally, educating caregivers on recognizing and responding to choking incidents is crucial.Q: Why is choking a serious concern in elderly nursing home residents?
A: Choking is a serious concern in elderly nursing home residents because they may have difficulty swallowing due to age-related changes or medical conditions. Choking or aspiration can lead to severe cases of complications, including aspiration pneumonia, which can be life-threatening.Q: What role does coughing play in preventing choking?
A: Coughing is a natural reflex that helps clear the airway by expelling food or liquid that may have entered the wrong passage. In elderly adults, an effective cough can prevent choking by dislodging the obstruction from the airway.Q: How can caregivers help elderly adults with dysphagia during meals?
A: Caregivers can assist elderly adults with dysphagia by ensuring they are sitting upright, encouraging slow eating and drinking, and providing foods that are easy to chew and swallow. In some cases, a feeding tube may be necessary to ensure adequate nutrition and prevent choking.Q: What is the role of swallowing therapy in managing dysphagia?
A: Swallowing therapy is used for swallowing difficulties and involves exercises and techniques designed to strengthen the muscles involved in swallowing. This therapy can help individuals with dysphagia improve their swallowing function and reduce the risk of choking.Q: Why is choking considered one of the leading causes of unintentional injury death in elderly adults?
A: Choking is considered one of the leading causes of unintentional injury death in elderly adults because it can quickly lead to a complete airway obstruction, resulting in suffocation if not promptly addressed. The risk is heightened in this population due to factors such as difficulty swallowing and decreased reflexes.Q: How can nursing homes minimize the risk of choking among residents?
A: Nursing homes can minimize the risk of choking among residents by training staff in choking prevention techniques, conducting regular assessments of residents' swallowing abilities, and preparing meals that are safe for those with difficulty swallowing. Creating individualized care plans to address specific needs is also essential.











 Login with Google
Login with Google Login with Facebook
Login with Facebook