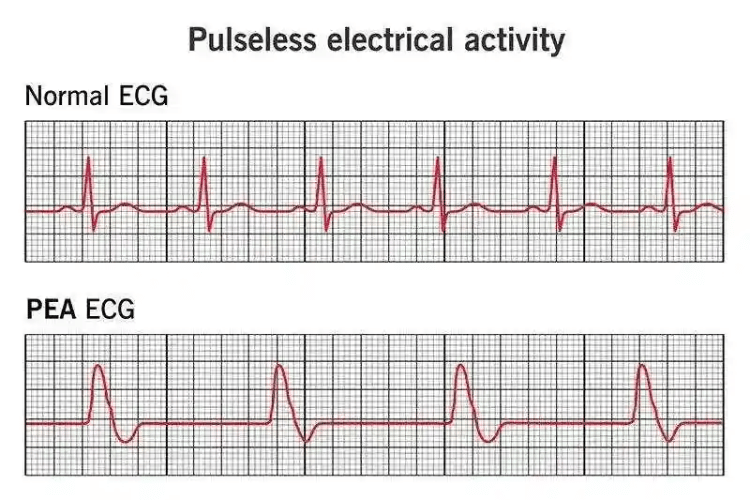
Pulseless Electrical Activity (PEA) is a life-threatening cardiac condition where organized electrical activity is present on an electrocardiogram (ECG), but no palpable pulse or effective cardiac output is detected. Unlike ventricular fibrillation (VF) or ventricular tachycardia (VT), PEA does not respond to defibrillation, making its management highly dependent on identifying and treating underlying causes. While PEA may seem like a rare occurrence, it is a critical condition encountered in emergency medicine, requiring rapid intervention to prevent fatal outcomes.
For the average person, cardiac arrest might seem synonymous with a "flatline" (asystole). Still, PEA represents a more complex scenario where the heart's electrical system appears functional, yet mechanical contraction fails. Medical professionals, particularly those in emergency and critical care, must understand the mechanisms, causes, and immediate interventions required to reverse PEA before irreversible damage occurs.
Let’s explore what PEA is, how it is diagnosed, the key underlying causes, and the latest advancements in its management.
Understanding PEA
PEA is a complex and often misunderstood condition that plays a significant role in cardiac arrest scenarios. This section provides a detailed examination of PEA, including its definition, underlying mechanisms, and its distinction from asystole. By understanding these aspects, healthcare providers and first responders can better identify and manage this life-threatening condition.
Definition of Pulseless Electrical Activity
Pulseless Electrical Activity (PEA) is a clinical condition characterized by the presence of organized electrical activity on an electrocardiogram (ECG) without a corresponding mechanical heartbeat or palpable pulse. In simpler terms, the heart's electrical system appears to be functioning, but the heart muscle fails to contract effectively, resulting in the absence of blood circulation.
PEA is not a specific rhythm but rather a clinical state that can occur with various underlying causes. It is one of the non-shockable rhythms in cardiac arrest, meaning that defibrillation is not indicated as the primary treatment. Instead, the focus is on identifying and addressing the reversible causes of PEA, often referred to as the "Hs and Ts," which include:
- Hypoxia: Insufficient oxygen levels in the blood.
- Hypovolemia: Severe blood or fluid loss.
- Hydrogen ion (acidosis): Imbalance in blood pH levels.
- Hyperkalemia or Hypokalemia: Abnormal potassium levels.
- Hypothermia: Critically low body temperature.
- Tension pneumothorax: Air trapped in the chest cavity, compressing the lungs and heart.
- Tamponade (cardiac): Fluid accumulation around the heart, restricting its ability to pump.
- Toxins: Drug overdoses or poisoning.
- Thrombosis (pulmonary or coronary): Blood clots in the lungs or coronary arteries.
The identification and treatment of these reversible causes are central to the management of PEA.
Mechanisms of Cardiac Arrest
To understand PEA, it is essential to explore the mechanisms of cardiac arrest, as PEA represents one of the potential rhythms observed during this critical event. Cardiac arrest occurs when the heart suddenly stops pumping blood effectively, leading to a cessation of circulation and oxygen delivery to vital organs.
The mechanisms of cardiac arrest can be broadly categorized into:
- Electrical Dysfunction Abnormalities in the heart's electrical system can disrupt the coordination of muscle contractions. This includes arrhythmias such as ventricular fibrillation (VF) and ventricular tachycardia (VT), which are shockable rhythms, as well as non-shockable rhythms like PEA and asystole.
- Mechanical Failure In some cases, the heart's electrical activity may remain intact, but mechanical issues prevent effective blood circulation. This is the hallmark of PEA, where the heart muscle fails to contract despite organized electrical signals.
- Combined Electrical and Mechanical Failure Conditions such as severe myocardial infarction (heart attack) or advanced heart failure can lead to both electrical and mechanical dysfunction, culminating in cardiac arrest.
Understanding these mechanisms is crucial for tailoring resuscitation efforts to the specific type of cardiac arrest rhythm.
Difference Between PEA and Asystole
While both PEA and asystole are classified as non-shockable rhythms in cardiac arrest, they differ significantly in their presentation and underlying physiology.
- Electrical Activity
-
- PEA: Displays organized electrical activity on the ECG, resembling normal or near-normal rhythms. However, this activity does not result in effective heart contractions or a palpable pulse.
- Asystole: Represents a complete absence of electrical activity, appearing as a flatline on the ECG.
- Prognosis
-
- PEA: The prognosis depends on the rapid identification and treatment of reversible causes. If the underlying issue is addressed promptly, there is potential for recovery.
- Asystole: Generally associated with a poorer prognosis, as it often indicates prolonged cardiac arrest or severe underlying conditions.
- Management Approach
-
- PEA: Focuses on high-quality cardiopulmonary resuscitation (CPR) and identifying reversible causes. Defibrillation is not indicated unless the rhythm transitions to a shockable state.
- Asystole: Emphasizes high-quality CPR and supportive care, with a focus on determining the cause of the arrest.
By distinguishing between PEA and asystole, healthcare providers can implement appropriate interventions and improve the chances of successful resuscitation.
Understanding PEA and its nuances is a critical component of managing cardiac emergencies. By recognizing its definition, mechanisms, and differences from asystole, responders can take targeted actions to address this life-threatening condition effectively.
Causes of Pulseless Electrical Activity
In the previous section, we explored the definition and distinguishing features of Pulseless Electrical Activity (PEA) in the context of cardiac arrest. Building on that foundation, this section delves into the causes of PEA, examining the common triggers, the underlying pathophysiology, and the risk factors that predispose individuals to this critical condition. Understanding these aspects is essential for identifying and addressing the root causes of PEA during resuscitation efforts.
Common Causes of PEA
Pulseless Electrical Activity is not a standalone diagnosis but rather a clinical manifestation of various underlying conditions. These causes are often categorized into reversible and non-reversible factors, with the reversible causes being the primary focus during resuscitation.
- Reversible Causes (The Hs and Ts)
-
- Hypoxia: Insufficient oxygen in the blood, often due to respiratory failure or airway obstruction.
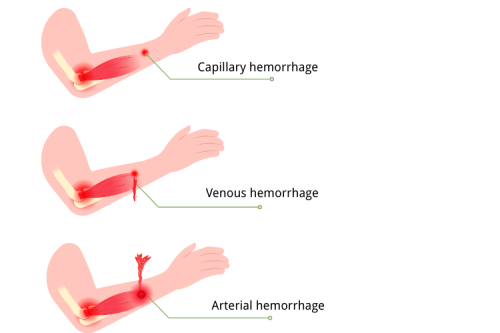
- Hypovolemia: Severe blood or fluid loss, leading to inadequate circulation.
- Hydrogen Ion (Acidosis): Metabolic or respiratory acidosis, causing a critical imbalance in blood pH.
- Hyperkalemia or Hypokalemia: Abnormal potassium levels that disrupt cardiac electrical activity.
- Hypothermia: Critically low body temperature, impairing cellular and organ function.
- Tension Pneumothorax: Air trapped in the chest cavity, compressing the lungs and heart.
- Tamponade (Cardiac): Fluid accumulation in the pericardial sac, restricting heart movement.
- Toxins: Drug overdoses or poisoning that interfere with cardiac or respiratory function.
- Thrombosis (Pulmonary or Coronary): Blood clots in the lungs or coronary arteries, obstructing blood flow.
- Non-Reversible Causes While less common, non-reversible causes such as advanced cardiac disease, severe trauma, or prolonged cardiac arrest may also result in PEA. These conditions often indicate a poor prognosis.
Identifying the specific cause of PEA is critical for tailoring resuscitation efforts and improving the likelihood of successful outcomes.
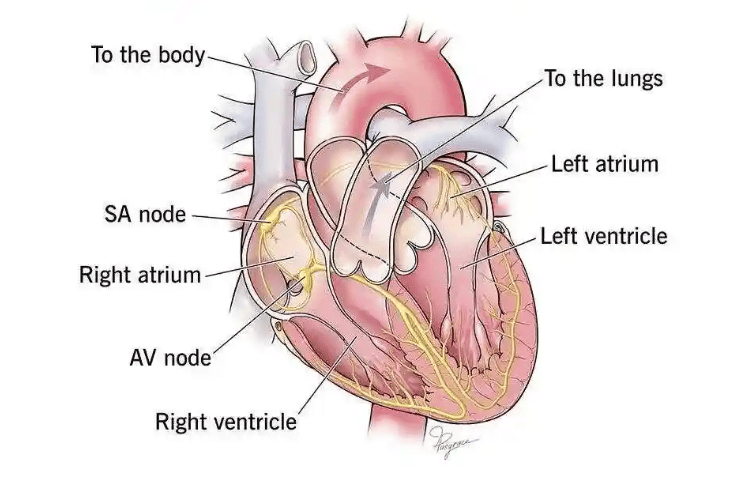
Pathophysiology Behind PEA
The pathophysiology of Pulseless Electrical Activity lies in the disconnect between the heart's electrical and mechanical functions. In a normal heart, electrical signals generated by the sinoatrial (SA) node coordinate the contraction of the heart muscle, resulting in effective blood circulation. However, in PEA, this coordination breaks down due to one or more underlying issues.
- Electrical Activity Without Mechanical Contraction In PEA, the heart's electrical system may appear functional on an electrocardiogram (ECG), but the mechanical contraction of the heart muscle is either absent or insufficient to generate a palpable pulse. This can occur due to:
-
- Severe hypovolemia, where the lack of circulating blood volume prevents effective contraction.
- Cardiac tamponade, where fluid pressure around the heart restricts its ability to pump.
- Impaired Oxygen Delivery Hypoxia and acidosis disrupt the heart's ability to generate energy for contraction. Without adequate oxygen, the myocardium (heart muscle) cannot sustain effective mechanical activity, even if electrical signals are present.
- Electrolyte Imbalances Abnormal levels of potassium, calcium, or magnesium can interfere with the heart's electrical conduction system, leading to ineffective or uncoordinated contractions.
- Obstructive Pathologies Conditions like tension pneumothorax or pulmonary embolism create physical barriers to blood flow, preventing the heart from maintaining circulation despite normal electrical activity.
Understanding the pathophysiology of PEA highlights the importance of addressing the underlying cause to restore the heart's mechanical function and circulation.
Risk Factors Associated with PEA
Certain individuals are at a higher risk of developing Pulseless Electrical Activity due to predisposing medical conditions or situational factors. Recognizing these risk factors can aid in early identification and prevention.
- Pre-Existing Medical Conditions
-
- Cardiovascular Disease: Conditions such as coronary artery disease, heart failure, or previous myocardial infarction increase the likelihood of PEA.
- Chronic Respiratory Disorders: Diseases like chronic obstructive pulmonary disease (COPD) or severe asthma can lead to hypoxia, a common cause of PEA.
- Electrolyte Imbalances: Chronic kidney disease or endocrine disorders may predispose individuals to abnormal potassium or calcium levels.
- Acute Medical Events
-
- Severe Trauma: Blood loss or chest injuries can directly lead to PEA.
- Drug Overdose: Certain medications or illicit drugs can depress cardiac or respiratory function, resulting in PEA.
- Sepsis: Severe infections can cause metabolic acidosis and cardiovascular collapse, contributing to PEA.
- Environmental Factors
-
- Hypothermia: Prolonged exposure to cold environments can impair cardiac function.
- High-Altitude Illness: Reduced oxygen availability at high altitudes may lead to hypoxia and PEA.
By understanding these risk factors, healthcare providers can implement preventive measures and improve the management of patients at risk for PEA.
In summary, the causes of Pulseless Electrical Activity are multifaceted, involving a combination of reversible and non-reversible factors, complex pathophysiological mechanisms, and identifiable risk factors. Addressing these elements is essential for effective resuscitation and improving patient outcomes.
Diagnosis of PEA
Clinical Signs and Symptoms
Diagnosing Pulseless Electrical Activity (PEA) begins with recognizing key clinical signs and symptoms. Patients with PEA often present with unresponsiveness, absent palpable pulses, and no measurable blood pressure despite organized electrical activity on the monitor. It is crucial to promptly assess for reversible causes such as hypoxia, hypovolemia, and electrolyte imbalances that could contribute to the condition.
Use of Electrocardiograms
Electrocardiograms (ECGs) play a vital role in diagnosing PEA by identifying the presence of organized electrical activity without corresponding mechanical heart function. While the rhythm on the ECG may resemble a normal sinus rhythm or another organized pattern, physical examination remains essential to confirm the absence of a pulse. ECG findings also aid in identifying underlying factors, such as prolonged QT intervals or signs of cardiac ischemia.
Distinguishing PEA from Other Rhythms
To differentiate PEA from other cardiac rhythms, it is important to discern whether the electrical activity on the monitor correlates with effective cardiac output. Conditions such as ventricular fibrillation or asystole exhibit distinctive ECG patterns, unlike the organized activity seen in PEA. The absence of a pulse alongside organized electrical activity confirms PEA rather than other shockable rhythms, guiding appropriate treatment strategies.
Treatment Strategies for PEA
In the previous section, we examined the causes and pathophysiology of Pulseless Electrical Activity (PEA), highlighting the importance of identifying reversible factors to improve outcomes. Building on that foundation, this section focuses on the treatment strategies for PEA, including immediate resuscitation techniques, the role of medications, and the critical steps involved in post-cardiac arrest care. A structured and timely approach to PEA management can significantly enhance the chances of survival and recovery.
Immediate Resuscitation Techniques
The cornerstone of PEA treatment lies in prompt and effective resuscitation efforts. Since PEA is a non-shockable rhythm, the focus is on high-quality cardiopulmonary resuscitation (CPR) and addressing the underlying causes.
- High-Quality CPR
-
- chest compressions: Delivering consistent, high-quality chest compressions is essential to maintain blood flow to vital organs. Compressions should be performed at a rate of 100–120 per minute and a depth of at least 2 inches in adults, allowing full chest recoil between compressions.
- Minimizing Interruptions: Interruptions in chest compressions should be minimized to ensure continuous circulation. Any pauses should be limited to essential tasks, such as rhythm checks or airway management.
- Airway and Breathing Support
-
- Ventilation: Providing adequate oxygenation is critical in PEA management. This can be achieved through bag-mask ventilation or advanced airway placement, such as endotracheal intubation.
- Oxygen Delivery: Administering 100% oxygen helps address hypoxia, one of the reversible causes of PEA.
- Identifying and Treating Reversible Causes
-
- The "Hs and Ts" framework (e.g., hypoxia, hypovolemia, tension pneumothorax, toxins) should guide the resuscitation team in identifying and addressing the underlying cause of PEA. For example:
-
- Administering fluids for hypovolemia.
- Performing needle decompression for tension pneumothorax.
- Using antidotes for specific toxins or drug overdoses.
- Monitoring and Feedback
-
- Continuous monitoring of the patient’s rhythm and pulse is essential to assess the effectiveness of resuscitation efforts. Capnography can also be used to measure end-tidal CO2 levels, which provide an indication of perfusion quality.
Medications for PEA Management
Medications play a supportive role in the management of PEA, primarily to address underlying causes and improve the chances of return of spontaneous circulation (ROSC).
- Epinephrine
-
- Mechanism of Action: Epinephrine is a vasopressor that increases coronary and cerebral perfusion by constricting blood vessels.
- Administration: It is administered intravenously or intraosseously at a dose of 1 mg every 3–5 minutes during resuscitation. Early administration of epinephrine is associated with improved outcomes in PEA.
- Reversible Cause-Specific Medications
-
- Sodium Bicarbonate: Used to correct severe metabolic acidosis, particularly in cases of prolonged cardiac arrest or hyperkalemia.
- Calcium Chloride: Administered in cases of hyperkalemia or hypocalcemia to stabilize cardiac membranes.
- Antidotes: Specific antidotes, such as naloxone for opioid overdose or atropine for bradycardia-related PEA, may be required based on the underlying cause.
- Fluids and Electrolytes
-
- Intravenous fluids, such as normal saline or lactated Ringer’s solution, are used to treat hypovolemia. Electrolyte imbalances, such as hypokalemia or hyperkalemia, should be corrected promptly with appropriate supplementation or medications.
- Advanced Therapies
-
- In some cases, advanced therapies like extracorporeal membrane oxygenation (ECMO) may be considered to provide circulatory support while addressing the underlying cause of PEA.
Post-Cardiac Arrest Care
Achieving ROSC is only the first step in the management of PEA. Post-cardiac arrest care is critical to optimize recovery and prevent further complications.
- Hemodynamic Stabilization
-
- Blood Pressure Management: Maintaining adequate blood pressure is essential to ensure organ perfusion. Vasopressors, such as norepinephrine, may be used to support blood pressure.
- Oxygenation and Ventilation: Targeting an oxygen saturation of 94–98% and avoiding hyperventilation are key to preventing secondary brain injury.
- Neurological Assessment and Care
-
- Targeted Temperature Management (TTM): Cooling the patient to 32–36°C for 24–48 hours can reduce the risk of neurological damage following cardiac arrest.
- Neurological Monitoring: Regular assessments, including imaging and clinical evaluations, help determine the extent of brain injury and guide further care.
- Identifying and Treating Underlying Causes
-
- Post-cardiac arrest care should include a thorough evaluation to identify and address the cause of the initial cardiac arrest. This may involve imaging studies, laboratory tests, or cardiac catheterization.
- Multidisciplinary Care
-
- A team-based approach involving cardiologists, neurologists, intensivists, and rehabilitation specialists is essential for comprehensive post-cardiac arrest care.
- Long-Term Recovery
-
- Patients who survive PEA may require long-term follow-up to address physical, cognitive, and emotional challenges. Cardiac rehabilitation programs can play a vital role in improving quality of life.
By combining immediate resuscitation techniques, appropriate medication use, and comprehensive post-cardiac arrest care, healthcare providers can improve outcomes for patients experiencing PEA. This structured approach underscores the importance of timely intervention and multidisciplinary collaboration in managing this life-threatening condition.
Frequently Asked Questions
What is pulseless electrical activity (PEA) and how does it relate to heart rhythms?
Pulseless electrical activity (PEA) is a condition where there is organized electrical activity in the heart, but it does not result in an effective pulse or adequate cardiac output. This condition can occur during cardiac arrest and is often associated with various underlying causes, making it crucial to identify and treat these causes promptly.
How does CPR assist patients with out-of-hospital cardiac arrest?
Cardiopulmonary resuscitation (CPR) is vital for patients experiencing out-of-hospital cardiac arrest. It helps maintain blood flow to vital organs until advanced medical help arrives. Immediate CPR can improve survival rates and outcomes for those in cardiac arrest, including those with PEA.
What are the common causes and treatment options for pulseless electrical activity?
The causes of pulseless electrical activity can range from hypoxia and hypovolemia to tension pneumothorax and cardiac tamponade. Treatment involves addressing these reversible causes while providing high-quality CPR and considering advanced interventions such as medications or advanced cardiovascular life support (ACLS).
What is the survival rate for patients with PEA?
The survival rate for patients with pulseless electrical activity varies depending on factors such as the underlying cause and the timeliness of intervention. Early recognition and treatment are crucial, and studies suggest that survival to hospital discharge is possible, especially when effective CPR is initiated promptly.
How does the presence of organized cardiac electrical activity affect treatment?
The presence of organized cardiac electrical activity suggests that the heart may still respond to treatment. In cases of PEA, recognizing this organized activity can guide clinicians in the management of the patient and indicate the potential for return of spontaneous circulation if the underlying cause is addressed effectively.
What distinguishes asystole from pulseless electrical activity?
Asystole is characterized by a complete absence of electrical activity in the heart, whereas pulseless electrical activity presents with organized electrical activity without an effective pulse. Understanding this distinction is crucial in the management of cardiac arrest patients, as the treatment protocols differ significantly.
How is the management of pulseless electrical activity approached in an in-hospital setting?
In an in-hospital setting, the management of pulseless electrical activity involves immediate assessment and intervention. This includes ensuring high-quality CPR, administering medications, and identifying reversible causes such as electrolyte imbalances or cardiac tamponade, all while following advanced cardiovascular life support protocols.
What is the role of the heart’s electrical system in cardiac arrest rhythms?
The heart's electrical system is responsible for coordinating the heart's beats and maintaining an effective heart rhythm. In cases of cardiac arrest, disruptions in this electrical activity can lead to rhythms such as PEA or ventricular fibrillation, making understanding this system essential for effective treatment and resuscitation efforts.
The Bottom Line
PEA is a complex and time-sensitive condition requiring a systematic approach to identify and treat reversible causes. Unlike shockable rhythms, its management hinges on high-quality CPR, rapid diagnosis of underlying etiologies, and targeted interventions.
For medical professionals, mastering PEA protocols is essential, as every minute without effective circulation decreases survival chances. Future advancements in resuscitation science, including ECMO and AI-assisted diagnostics, may further refine PEA management, but for now, adherence to ACLS guidelines remains the gold standard.
When faced with PEA, remember: "Pump and Probe"—sustain perfusion while relentlessly searching for the cause. The right intervention at the right time can mean the difference between life and death.




 Login with Google
Login with Google Login with Facebook
Login with Facebook