
Allergic rhinitis, commonly known as hay fever, is a condition that affects millions of people worldwide. It occurs when the immune system overreacts to allergens like pollen, dust mites, or pet dander, leading to symptoms such as sneezing, nasal congestion, and itchy eyes. While it may seem like a minor inconvenience, allergic rhinitis can significantly affect daily life, leading to fatigue, disrupted sleep, and reduced productivity.
Understanding the causes, symptoms, and treatments of allergic rhinitis is essential for effective management. In this blog, we’ll explore everything you need to know about this common condition, from identifying triggers to finding the best treatment options. Keep reading to take control of your allergies and improve your quality of life!
What Is Allergic Rhinitis?
Allergic rhinitis, commonly known as hay fever, is an allergic reaction to airborne allergens like pollen, dust mites, or pet dander. It primarily affects the respiratory system, eyes, and skin. When exposed to an allergen, the immune system overreacts by releasing immunoglobulin E (IgE) antibodies. These antibodies cause mast cells to release histamine and other chemicals into the bloodstream. This process leads to inflammation in the nasal passages and sinuses, causing the hallmark symptoms of the condition.
In more persistent cases, this inflammation can lead to chronic nasal congestion and discomfort. The airways become sensitive, and symptoms like sneezing, itching, and a runny nose can appear within minutes of exposure. This reaction can significantly impact a person's quality of life. Understanding that this is an immune response to harmless substances is key to effectively managing allergic rhinitis.
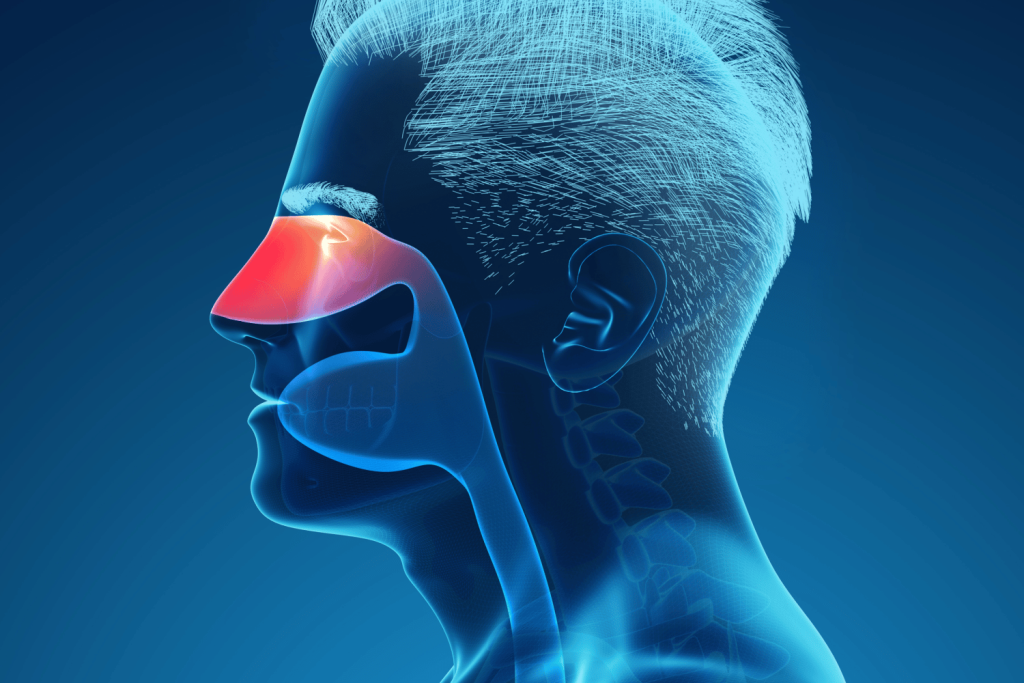
Ray Picture of Man Showing Respiratory System with Nasal Cavity on Blue Background, Illustration
Common Allergic Rhinitis Triggers You Need to Know
Various allergens can trigger allergic rhinitis. Therefore, people should be aware of allergens that they may be sensitive to and that can cause reactions. Moreover, they should try to avoid these triggers to prevent or reduce symptoms. Some of the most common allergens are discussed as follows:
Pollen
Pollen from trees, grasses, and weeds is the most common cause of seasonal allergic rhinitis, or hay fever. These tiny grains are released into the air to fertilize other plants. When inhaled by someone with an allergy, they trigger symptoms like sneezing, a runny nose, and itchy eyes. The type of pollen and the time of year it's prevalent can vary depending on the plant and geographic location.
For those with known pollen allergies, monitoring local pollen counts and limiting outdoor exposure on high-pollen days are necessary preventive measures. Keeping windows closed and using air purifiers with HEPA filters can help reduce indoor pollen levels. Over-the-counter antihistamines or nasal sprays can also relieve symptoms.
Dust Mites
Dust mites are microscopic organisms that live in house dust and are a common trigger for year-round allergic rhinitis. They thrive in warm, humid environments and are often found in bedding, upholstered furniture, and carpets. It is the dust mites' waste products, not the mites themselves, that cause the allergic reaction. Symptoms include sneezing, a runny nose, and nasal congestion, often worse in the morning.
Pet Dander
Proteins found in an animal's skin flakes (dander), saliva, or urine can trigger allergic rhinitis. The most common pets that cause allergies are cats and dogs, but other animals, such as rodents and horses, can also be a source. These allergens are lightweight and can remain airborne for long periods, easily sticking to furniture, clothes, and other surfaces. Even if a pet is not in the room, the dander can still be present and cause symptoms.
Mold Spores
Molds are fungi that can be found both indoors and outdoors. They release tiny spores into the air that can be inhaled, triggering allergic rhinitis symptoms in sensitive individuals. Indoors, mold thrives in damp, poorly ventilated areas like bathrooms, basements, and kitchens. Outdoor mold is common in soil, compost piles, and on wet leaves. Symptoms can be seasonal or year-round, depending on the type of mold and the climate.
Air Pollution and Irritants
A rare but recognized cause of non-allergic rhinitis symptoms is exposure to air pollutants and chemical irritants. This can include cigarette smoke, strong perfumes, cleaning products, and fumes from traffic or industry. While not a true allergic reaction involving the immune system, these irritants can inflame the nasal passages and mimic the symptoms of allergic rhinitis, such as sneezing and congestion. This condition can be managed by avoiding exposure to known irritants.
How to Identify Allergic Rhinitis Symptoms Before It’s Too Late
Allergic rhinitis symptoms can appear seasonally or year-round. Therefore, people experiencing these issues must understand what to look for and what complications can arise to manage them effectively:
Respiratory Symptoms
The most common symptoms of allergic rhinitis involve the respiratory system. These include frequent sneezing, a runny or stuffy nose (nasal congestion), and postnasal drip, where mucus drips down the back of your throat. An itchy nose, throat, or roof of the mouth is also very common. In some cases, this can lead to a persistent cough or a feeling of chest tightness.
Eye Symptoms
Allergic rhinitis often involves noticeable eye irritation. Itchy, watery, and red eyes (allergic conjunctivitis) are common symptoms. Your eyes may feel gritty or burn, and you might notice swelling or dark circles under your eyes, often called "allergic shiners." These symptoms occur when the same allergens that affect your nose also irritate the membranes covering your eyes.
General Symptoms and Fatigue
General feelings of being unwell are key signs of allergic rhinitis. These include fatigue and tiredness, often caused by poor sleep due to nasal congestion. You might also experience headaches, sinus pressure or pain, and a decreased sense of smell or taste. This overall feeling of being run-down can significantly impact your daily activities and quality of life.
Skin Reactions
While less common than respiratory or eye symptoms, the skin may also be affected. Some people experience itchy skin or develop hives (urticaria), which are raised, itchy welts. Eczema (atopic dermatitis) can also be worsened by exposure to allergens. These skin symptoms often occur alongside other signs of allergic rhinitis and may indicate a more significant allergic sensitivity.
Ear and Throat Symptoms
As nasal passages swell and become congested, it can affect surrounding areas. Itchy ears, a feeling of fullness, or ear popping can occur due to pressure changes in the Eustachian tube. A sore or scratchy throat is also common, often caused by postnasal drip irritating the throat lining. These symptoms show how the allergic response can extend beyond just the nose.
How Is Allergic Rhinitis Diagnosed?
Allergic rhinitis is diagnosed mainly by reviewing symptoms and medical history. The pattern of symptoms, such as sneezing, congestion, and itchy eyes, often points to an allergic cause. If you have symptoms of allergic rhinitis, here’s what you can expect:
Clinical Examination
The doctor begins by reviewing your medical history and assessing your symptoms, such as sneezing, a runny nose, nasal congestion, and itchy, watery eyes. The timing of these symptoms—whether they occur seasonally or year-round—is often enough to suggest a diagnosis of allergic rhinitis. The medical team will ask about potential triggers in your environment to help determine the cause.
Skin Prick Tests
To identify the specific allergens responsible for your symptoms, an allergy specialist may perform a skin prick test. During this test, small amounts of common allergens, such as pollen, dust mites, or pet dander, are introduced to the skin through tiny pricks. The skin is then monitored for any reaction, such as redness or a small, raised bump, which indicates an allergy to that substance.
Blood Tests
In some cases, a blood test may be used to confirm an allergy. This test measures the amount of specific immunoglobulin E (IgE) antibodies in your blood. The immune system produces IgE antibodies in response to an allergen. Elevated IgE levels to a specific allergen can confirm the diagnosis and identify the trigger of your allergic rhinitis.
Effective Treatments for Allergic Rhinitis
Treatment for allergic rhinitis must be consistent to manage symptoms effectively. The primary goal is to reduce symptoms and improve quality of life. Several therapies are available, depending on the severity of the reaction and the specific triggers. The major steps taken for the treatment of allergic rhinitis are as follows:
Antihistamines
The first-line treatment for mild allergic rhinitis is often an antihistamine. Antihistamines work by blocking histamine, the chemical released by the immune system during an allergic reaction. They are effective at relieving sneezing, itching, and a runny nose. Oral antihistamines are available over the counter and by prescription. They should be taken as needed or daily during allergy season for best results.
Nasal Corticosteroids
Nasal corticosteroid sprays are highly effective for reducing inflammation in the nasal passages. They help relieve nasal congestion, sneezing, and a runny nose. These sprays are often recommended for moderate to severe allergic rhinitis and are considered safe for long-term use. Unlike decongestant sprays, they are not habit-forming and work best when used consistently every day.
Decongestants
Decongestants may be used to provide short-term relief from severe nasal congestion. They work by narrowing the blood vessels in the nose, which reduces swelling and stuffiness. However, oral decongestants can raise blood pressure, and nasal decongestant sprays should not be used for more than a few days, as they can cause rebound congestion, worsening symptoms.
Immunotherapy
In cases of persistent or severe allergies, immunotherapy may be recommended. This treatment involves exposing the body to small, increasing amounts of an allergen, either through allergy shots or sublingual (under-the-tongue) tablets. Over time, this desensitizes the immune system to the allergen, reducing the severity of allergic reactions. This is a long-term solution that can provide lasting relief.
Lifestyle Adjustments
Patients should make lifestyle changes to avoid known triggers. This can include using air purifiers with HEPA filters, keeping windows closed during high pollen seasons, and washing bedding frequently in hot water to kill dust mites. Avoiding triggers is a key part of managing allergic rhinitis and can significantly reduce the need for medication.
Top Strategies to Avoid Allergic Rhinitis Triggers
The best course of action when dealing with allergens is to know the prevention strategies. This may involve avoiding known triggers and taking steps to reduce exposure in your daily environment. The following are some of the preventive measures you can adopt to avoid allergic rhinitis triggers:
Minimize Exposure
Avoidance is the most effective prevention strategy. Individuals with known pollen allergies should stay indoors on dry, windy days and during high pollen seasons. Keep windows and doors closed and use an air conditioner with a clean filter. Investing in a high-efficiency particulate air (HEPA) filter can also help remove allergens from the air inside your home.
Maintain Cleanliness
For indoor allergens like dust mites and pet dander, keeping your home clean is crucial. Regularly vacuum carpets and upholstery with a HEPA-filter vacuum. Wash bedding, curtains, and stuffed toys in hot water at least once a week to kill dust mites. Using allergen-proof covers on mattresses and pillows can also create a barrier against these common triggers.
Monitor Air Quality
In some cases, an allergist may recommend monitoring daily pollen and mold counts. Local weather reports or specific apps can provide this information. On days when pollen or pollution levels are high, it's best to limit outdoor activities, especially during the morning when pollen counts are typically at their peak. Planning outdoor time for later in the day can help reduce your exposure.
Use Protective Gear
When you can't avoid exposure to allergens, protective gear can help. Wear a mask when doing yard work, like mowing the lawn or raking leaves, to prevent inhaling pollen and mold spores. Wearing sunglasses can also help protect your eyes from airborne allergens. If you've been outside, changing your clothes and showering can remove pollen from your skin and hair.
Stay Safe and Manage Allergic Rhinitis Effectively!
Allergic rhinitis is a common condition that can significantly impact daily life. Consistent access to treatment, including antihistamines and nasal sprays, is essential for effectively managing symptoms. Individuals with allergic rhinitis should work with a healthcare professional to identify their triggers and create a personalized management plan.
Enrolling in a first aid course that covers allergy management can equip individuals with the necessary skills to respond to their own or others' symptoms. Knowledge and readiness significantly enhance the ability to control allergic rhinitis and improve overall quality of life.















 Login with Google
Login with Google Login with Facebook
Login with Facebook